CHAPTER 23 Idiopathic Scoliosis
Idiopathic scoliosis is the most common cause of spinal deformity; 80% of all scoliosis cases are due to idiopathic scoliosis. Before arriving at the diagnosis of idiopathic scoliosis in a patient, other causes, such as congenital, neuromuscular (developmental or acquired), functional, inflammatory or infectious, pathologic, and intraspinal, have to be discounted. Ponseti and Friedman1 first described early-onset scoliosis in 1950. Dickson2 expounded further on that concept and proposed that idiopathic scoliosis be divided into early (0 to 5 years old) and late onset (>5 years old), based on spinal growth velocity noted in these two age groups. Presently, idiopathic scoliosis is divided into three categories based on chronologic age: infantile (birth to 2 years + 11 months), juvenile (3 years to 9 years + 11 months), and adolescent (10 years to 17 years + 11 months).3 The radiographic diagnosis necessitates measuring the coronal plane angle, using the Cobb method, as equal to or greater than 10 degrees. Patients with curves less than 10 degrees are considered to have spinal asymmetry.4,5
Epidemiology
Infantile and juvenile scoliosis are less prevalent than adolescent idiopathic scoliosis. Infantile idiopathic scoliosis is more common in Europe, constituting less than 1% of idiopathic scoliosis cases in the United States, and tends to comprise left-sided thoracic curves, typically occurring in boys. More recent reviews suggest that there might be a decline in its incidence.6 Juvenile cases are typically diagnosed at age 7 years in girls and 5 years in boys and account for about 10% to 20% of idiopathic scoliosis cases.3 In contrast to infantile idiopathic scoliosis, juvenile cases tend to occur predominantly in girls and tend to comprise right-sided curves. Between the ages of 3 and 6 years, there seems to be a similar distribution between boys and girls, however, again becoming predominant in girls after age 6 years.
Adolescent idiopathic scoliosis is more prevalent than other types of idiopathic scoliosis. Among adolescents, the prevalence of 10-degree curves is less than 3%, with about 5% of curves showing progression of greater than 30 degrees.4 This prevalence decreases as a function of curve magnitude, however, to about 0.3% to 0.5% and 0.1% in curves measuring 20 degrees and 40 degrees.7 The prevalence of curves greater than 10 degrees is higher among girls, with a 4 : 1 ratio of girls to boys.8
Etiology
Infantile scoliosis occurs roughly in 1 of 10,000 births. Possible causes are thought to occur from intrauterine molding or postnatal pressure on the spinal column from supine positioning while sleeping. Other etiologic factors that have been considered in idiopathic scoliosis include dysfunction in proprioception to maldevelopment in central pattern generators in the spinal cord9–11 and connective tissue, hormonal, and muscle structural changes.12 More recent reports in the literature strongly suggest a genetic link. The growth spurt noted among adolescents seems to play a role in progression, as a critical buckling load is reached on the existing curve as the spine grows. In a review of the literature, Kouwenhoven and Castelein13 concluded many factors may play a role in the initiation and progression of adolescent idiopathic scoliosis at a certain age. The literature suggests, however, that in the observed deformation of the spine, genetics and the unique mechanics of the fully erect posture, which is exclusive to humans, play an important role.
Genetics
The genetics of idiopathic scoliosis seem to be similar in all idiopathic groups. The incidence rate is 11% among first-degree relatives, 2.4% among second-degree relatives, and 1.4% among third-degree relatives.14 Concordance among monozygotic and dizygotic twins has been reported to range from 73% to 92% and 36% to 63%.15,16 In 2007, Anderson and colleagues17 published a population-based study taken from the Danish Twin Registry in which 46,418 twins were registered. From the 34,944 respondents, the concordance rate for monozygotic twins was 13% versus 0% for dizygotic twins. In 2007, Gao and colleagues18 published a report providing evidence of linkage and association with 8q12 loci. Through further investigation, they discovered the first gene (CHD7) associated with a susceptibility to idiopathic scoliosis. In 2008, Kulkarni and colleagues19 mapped a developmentally critical CHD gene to 15q26.1 and when taken together with CHD7, this suggested a possible role for CHD2 in the embryonic development of the spine. More recently in 2009, Gurnett and colleagues20 published a report of a single multigenerational family in which adolescent idiopathic scoliosis and pectus excavatum segregated as an autosomal dominant condition. Through linkage analysis, the investigators identified a genetic locus for the two conditions on chromosome 18q. Although genetic mapping for idiopathic scoliosis is still in its infancy, great strides are being made to help clinicians better understand the etiology and prevalence of this condition.
Natural History
About 90% of infantile curves show spontaneous resolution, especially among infants who are younger than 1 year when idiopathic scoliosis is diagnosed.6,21 The curves that typically progress are double curves with a thoracic component. Insight into the curves that can progress can be obtained from the rib-vertebral angle difference (RVAD) and “phase of the rib head.”22 In terms of phase of the rib head, if the head and neck of the convex rib of the vertebral body at the apex of the curve does not overlap the vertebral body, it is termed phase I; if it does overlap, it is termed phase II. In terms of the latter, curves with RVAD greater than 20 degrees or phase II angles are very likely to progress. Phase II angles are almost certain to progress; RVAD calculation is unnecessary when a curve is noted to be phase II type. Juvenile curves less than 25 degrees also can spontaneously resolve. These curves tend to progress, however, if they are discovered before age 6 years and idiopathic scoliosis is diagnosed or if they are greater than 30 degrees. About 70% of juvenile curve types tend to progress. The RVAD has not proved to be useful as a predictor of curve progression.
Many factors are considered in the natural history of adolescent idiopathic scoliosis. Growth potential, skeletal maturity, curve magnitude, and curve location are important considerations when assessing progression of adolescent idiopathic scoliosis. Although family history, gender, and rotation do not seem to have an effect on progression, growth potential seems to have a significant effect. Peak height growth seems to correlate best with, and is a better predictor of, progression than skeletal maturity. In terms of biomechanics, this likely is secondary to attaining vertebral column height, which leads to a critical buckling load and greater bending moments with eventual curve progression. In girls, peak height growth seems to occur 6 to 12 months before the onset of menarche. In boys, peak height growth seems to correlate with the closure of triradiate cartilages. Larger or double curves tend to progress more than single curves. Additionally, curves can progress after skeletal maturity; thoracic curves greater than 50 degrees and thoracolumbar/lumbar curves greater than 30 degrees can progress on average 1 degree per year.23,24
Evaluation
History and Physical Examination
A complete history and physical examination is completed, and any family history of scoliosis is noted. With infantile and juvenile cases in particular, a thorough prenatal and birth and developmental history is obtained. In adolescent cases, growth spurt history, if any at the time of presentation, is noted. This information is imperative in determining peak growth velocity and its implications on curve progression. Symptoms of pain or weakness and how the patient perceives his or her appearance relative to the deformity are especially important with adolescent idiopathic scoliosis.25 Age at onset of menarche and voice changes in boys are noted as well because they are likely predictors of growth potential and possible curve progression.
Trunk shift is evaluated with the patient standing and the hips and knees fully extended. The relationship of the patient’s head to the pelvis is also noted in evaluating the overall coronal and sagittal balance. Any shoulder, breast, or pelvic asymmetry is noted.26 Curve rotation is assessed by performing an Adams forward-bend test and is quantified with a scoliometer. This assessment is modified in infants by laying the patient on the examiner’s knee. This test also helps assess the rigidity of the curve, which is an important factor in terms of prognostication. Leg-length discrepancy and pelvic obliquity are evaluated. Alternatively, a sitting forward test can be performed. The latter maneuver can also help rule out plagiocephaly and developmental hip dysplasia, especially in infants. When leg-length discrepancy is the likely cause of the deformity, a shoe lift is used to reevaluate the patient to determine if the curve corrects.
A thorough neurologic examination is performed. The neurologic examination includes all cranial nerves; motor strength; reflexes (including abdominal reflexes), often associated with Chiari malformations; sensory modalities; and gait.27 Finally, other possible causes of scoliosis, such as congenital, neuromuscular, and syndromic types, must be ruled out. Infection, neoplasms, and spondylolisthesis also must be discounted.
Radiographic Evaluation
Posteroanterior and lateral 36- × 14-inch long cassette views including bending films—with appropriately placed bolsters—for further curve classification and planning bracing or surgical intervention are obtained, and the Cobb angles are measured.5 Curves greater than 20 degrees in infants and children, neurologic symptoms in all patients with idiopathic scoliosis, and left-sided, sharp angular or irregular curve patterns require further investigation, including screening total spine magnetic resonance imaging (MRI).28,29 When anomalies of the nervous system are present on MRI, a neurosurgical consultation is indicated.
Classification Systems
There is no formal curve classification system for infantile or juvenile scoliosis. The first treatment-based adolescent idiopathic scoliosis classification was developed in 1983 by King and colleagues.30 They reported on a series of 405 patients with adolescent idiopathic scoliosis, developing a uniplanar system based on thoracic curves and analyzing only the coronal plane. This system allowed for surgical planning and helped in assessing whether or not a King II curve could be selectively fused.31 Interobserver and intraobserver reliability of this traditional thoracic classification system is fair at best, however.32,33 Additionally, coronal decompensation has been reported after selective fusions.
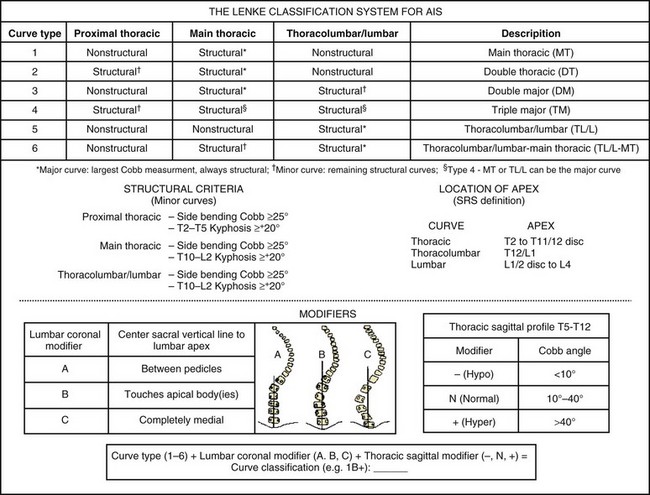
Lenke and colleagues34 developed a comprehensive, practical two-dimensional classification system in 2001, which included the sagittal plane as well (Fig. 23–1). The Lenke curve classification includes not only thoracic curves, but also thoracolumbar/lumbar curve patterns. Additionally, this classification allows the surgeon to assess curves in coronal and sagittal planes, and it has been proven reliable in terms of interobserver and intraobserver reliability.32,33 Its definition of the structural characteristics of a proximal thoracic curve has been deemed reliable, leading to shorter proximal fusions when this curve pattern is nonstructural.35 The Lenke classification allows a stricter structural curve evaluation, permitting a more objective analysis of when a given curve would tolerate a selective fusion leading to a balanced outcome.36,37 The latter is clinically significant because one of the most important principles in preventing postoperative decompensation is proper identification of curve patterns, including curves that tolerate selective fusion.31,38 This three-tiered classification combines a curve type (1 through 6) and coronal lumbar and sagittal thoracic modifiers to produce a triad comprehensive curve classification (e.g., 1A−).
More recently, the addition of a lower end vertebra (LEV) modifier has been proposed for the Lenke classification. The LEV of the lowest structural curve was found to be a highly reliable vertebral landmark, and comparison of the LEV with a selected lowest instrumented vertebra (LIV) is an important consideration in the overall evaluation of the surgical treatment of adolescent idiopathic scoliosis.39 A more detailed postoperative assessment of the distal fusion length is theoretically allowed by comparing the LIV with the LEV. Such a modifier aids in a more thorough evaluation of the Lenke curve classification (e.g., 5CN-L3 when L3 is the LEV of the curve being classified).
Three-Dimensional Classification
Although the Lenke classification system has criteria in the coronal and the sagittal planes that have an impact classification, it still has shortcomings because scoliosis is a known three-dimensional deformity, and the axial or transverse plane is not a component of this system. A task force of the Scoliosis Research Society has been charged with developing a clinically useful three-dimensional analysis and ultimate classification of scoliosis.40 The key factor in this assessment would be the plane and maximal curvature, which is the three-dimensional deformity that occurs as the spine translates and rotates out of the normal sagittal profile in scoliosis deformities. It is expected that in the next decade much more information will be provided so that three-dimensional analysis and classification will become a standard for all practitioners.
Nonoperative Treatment Options and Indications
Three fundamental treatment options exist for idiopathic scoliosis: observation, bracing and casting, and surgery. These treatment modalities are based on the natural history of idiopathic scoliosis or the potential or probability of curve progression.4,41 Many modalities have been proposed to slow or halt curve progression, such as electrical stimulation and physical therapy; however, none of these modalities have been scientifically proven to be a viable alternative in the treatment of scoliosis.42,43
Observation
Most infantile curves are left-sided; these curves have been known to resolve spontaneously up to 90% of the time, but they can progress.41 Deciphering which curves will progress can be guided by the RVAD and the relationship of the apical rib head to the vertebral body (i.e., phase I or II).22 Typically, curves less than 20 degrees are expectantly followed every 6 to 8 months. Infants with curves less than 25 degrees and RVAD less than 20 degrees and children with curves less than 25 degrees should be followed clinically and radiographically every 6 months. Treatment is instituted for curves greater than 25 degrees. Treatment is also started for a progression of 5 degrees or greater in two consecutive visits or 10 degrees or greater in one follow-up visit. Juvenile curves more often require operative intervention, however.
Bracing and Casting
Bracing44 is the nonoperative treatment of choice in small but progressive scoliosis in growing children and teens. In about 75% of cases, bracing can control the curve and avoid progression, rendering the curve small enough so that the risk of progression after growth is unlikely.42 In a younger child, whose growth potential remains a significant issue, bracing allows for continued growth until the patient requires eventual operative treatment because of curve progression. With infantile cases, molded casting followed by bracing used to be the mainstay in nonoperative management. Bracing and casting of these patients comes with potential consequences, however, that include pulmonary restriction, which can have future ramifications.45,46 Sanders and colleagues47 found serial casting to be beneficial in the treatment of infantile scoliosis. They reported that curves less than 60 degrees often fully corrected in infants if casting was started before age 20 months.
Bracing is usually started the first office visit when the patient is skeletally immature (Risser ≤2) and presents with a 25- to 40-degree curve. Several brace options exist, and deciding which brace to use depends on the apex of the curve and physician preference. Curves with an apex above T6 would likely require the use of a Milwaukee (cervicothoracolumbosacral orthosis) brace.48 Conversely, curves with apices at T7 or below and above L2 do well in a Boston underarm thoracolumbosacral orthosis brace, and these braces are more socially acceptable because of the lack of a cervical extension. The Charleston bending brace is an option if the child is noncompliant to brace-wear. This brace is typically worn at night, and some studies have shown its efficacy.49,50 The efficacy of a brace seems to depend on the length of time the brace is worn.51 When bracing is initiated and pad placement is deemed appropriate, patient follow-up occurs every 4 to 6 months, with in-brace radiographic evaluation and appropriate fitting adjustments made when necessary.
Modifications to the standard thoracolumbosacral orthosis include variations of the Chêneau brace (Jacques Chêneau, Münster, Germany) and the SpineCor dynamic brace (SpineCorporation, Chesterfield, UK). The Chêneau 2000 orthosis allows for a greater amount of initial correction by using a hypercorrected mold and pads, which provide derotational forces.52 This brace is the first that uses the theory of expansion to allow for active correction by respiratory movements.53 The SpineCor54 and TrIAC (Boston Brace International, Avon, MA) are nonrigid braces. They work by using straps, which correspond to a specific correcting movement depending on the curve pattern, producing a progressive positional change, dynamic curve correction, and appropriate muscle balance.
Operative Intervention
Operative intervention is usually recommended for patients whose curves progress despite nonoperative management.54 In infants, operative intervention is controversial; it is occasionally performed in infants with curves greater than 45 degrees or thoracolumbar/lumbar curves greater than 40 degrees. Children are typically more prone to curve progression and are more likely to require operative intervention. Other patients who are likely to benefit from operative intervention are skeletally immature patients with adolescent idiopathic scoliosis with a greater than 40- to 45-degree curve and mature patients with curves greater than 50 degrees.23,55
Surgical Techniques
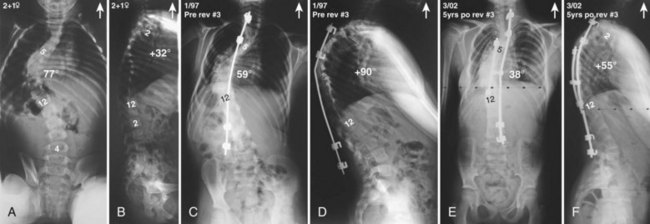
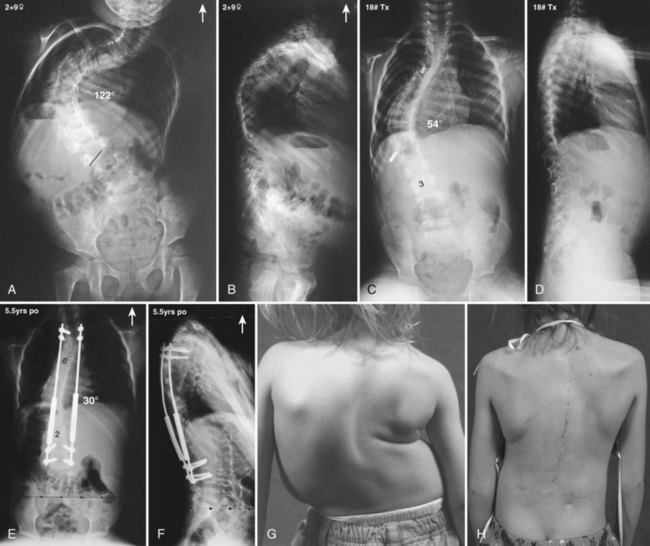
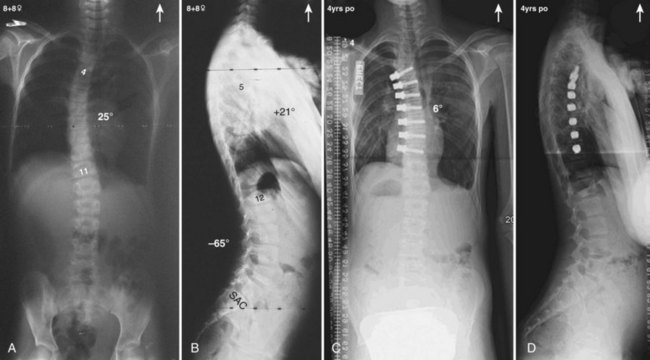
Currently, anterior-only, posterior-only, and circumferential procedures are the mainstay of surgical treatment options.57 The prevalence of anterior-only and circumferential procedures has declined with a concomitant increase in posterior-only procedures. Surgeons have become aware more recently that early intervention with a definitive anteroposterior fusion for progressive infantile and juvenile curves leads to loss of trunk height development, which can lead to chest wall and lung underdevelopment.58,59 This problem has promoted innovative techniques to try to control progressive curves surgically without definitive fusion, which include epiphysiodesis,60,61 growing rod placement (Figs. 23-2 and 23-3),62 intervertebral stapling (Fig. 23–4),86 spinal tethering (Fig. 23–5),66 and the vertical expandable prosthetic titanium rib67; the last-mentioned is used more in progressive early-onset scoliosis in which rib and chest wall deformities can be quite severe.64
Many surgeons today still prefer to perform an anterior approach in younger patients when there is risk of crankshaft development and especially for thoracolumbar and lumbar major curves (Lenke type 5). With the introduction of pedicle screws, a posterior approach has shown numerous benefits over an anterior procedure, such as better maintenance of the obtained correction, providing more powerful corrective forces, three-column control, and obviating the need for anterior releases and thoracoplasties.68–74 In addition, a posterior approach avoids the negative consequences of chest cage disruption and pulmonary compromise that can result from an open anterior approach (Fig. 23–6).75–77 In addition, the thoracic aorta is at risk if an anteriorly placed screw penetrates the vertebral cortex on the opposite side.78,79
< div class='tao-gold-member'>
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree