History and Physical Examination of the Hip
Hal David Martin
Key Points
• Perform a standardized history and physical examination protocol of the hip.6,7
• Perform examinations of the hip with consistent technique.
• Use quality radiographic10 and three-planar osseous assessment through magnetic resonance imaging (MRI) or computed tomography (CT).14
• Do intra-articular/extra-articular injection tests to aid in diagnosis.
Introduction
The goal of the clinical examination of the hip is to assess the four layers: the osseous, capsulolabral, musculotendinous, and neurovascular. It is important to understand the balance and interrelationship that each system has with the other in a static and dynamic fashion, as the hip assumes an essential role in most activities. Not only is the hip responsible for distributing weight between the appendicular and axial skeletons, it is also the joint from which motion is initiated and executed. During running and jumping, forces upon the hip joint can reach three to five times body weight.1 Hip pain often stems from a sports-related injury,2 and some athletes are prone to hip injury and secondary degenerative hip disease.3,4
Currently, 60% of intra-articular disorders are misdiagnosed initially.5 An organized physical examination is designed to assess the hip, the back, and abdominal, neurovascular, and neurologic systems. Comorbidities often coexist with complex hip pathology; therefore it is important that physical examination of the hip be inclusive enough to rule out other joints as a dominant cause of complaint. The hip is recognized early as the source of pain when a consistent method of interpreting the history and clinical examination of the hip is followed. The goals of this chapter are (1) to review pertinent information required for a detailed patient history, (2) to describe how clinical examination of the hip are performed, and to explain why these tests are important, and (3) to discuss current controversies and future considerations related to physical examination of the hip.
History and Physical Examination
History
A complete patient history is obtained before physical examination of the hip is performed. The first factors in consideration of treatment are the age of the patient and the presence or absence of trauma.1 A description of the present condition is documented, including date of onset, mechanism of injury, pain location, and factors that increase or decrease the pain.6,7 Previous consultations, surgical interventions, and injuries are documented. Treatments to date, such as rest, physical therapy, ice, heat, nonsteroidal anti-inflammatories, surgery, injections, orthotics, and the use of support aids, must be delineated. Limitations to patient function are detailed; these may involve getting into or out of the bathtub or car, performing activities of daily living, jogging, walking, or climbing stairs. Symptoms related to the back, the neurologic system, or the abdomen and lower extremity complaints must be recognized.7 Lumbar problems occasionally are confused with problems in the hip as a partial or dominant cause of complaint. Associated complaints, such as pain in the abdomen or back, numbness, weakness, cough, or sneeze exacerbation, help the clinician to identify lumbar issues.7
The vascular supply to the femoral head and any possible sources of disruption are screened, including metabolic disorders such as abnormalities in lipids, thyroid, homocysteine, and clotting mechanisms.7 The social history of the patient is reviewed to identify the presence or use of tobacco, alcohol, steroids, or altitude issues, all of which can affect the blood supply to the femoral head. A history of sports and recreational activities helps to reveal the type of injury.3,6,7 Rotation sports, such as golf, tennis, ballet, and martial arts, have been commonly associated with injury to the intra-articular structures, including the labrum, iliofemoral ligament, and ligamentum teres.
The history and physical examination of the hip will direct the differentiation of intra-articular versus extra-articular sources of pain, along with location of the presenting pain and the presence or absence of popping/locking. Extra-articular sources of pain often respond well to nonoperative treatment, and intra-articular sources require further workup, which may include x-rays,8–13 magnetic resonance imaging (MRI),14,15 MRI arthrogram,16–19 or injection tests. Patient goals and realistic expectations of treatment are discussed. Communication, understanding, empathy, and compassion are important in obtaining an accurate history. Figure 30-1 provides an example of a complete hip history form.
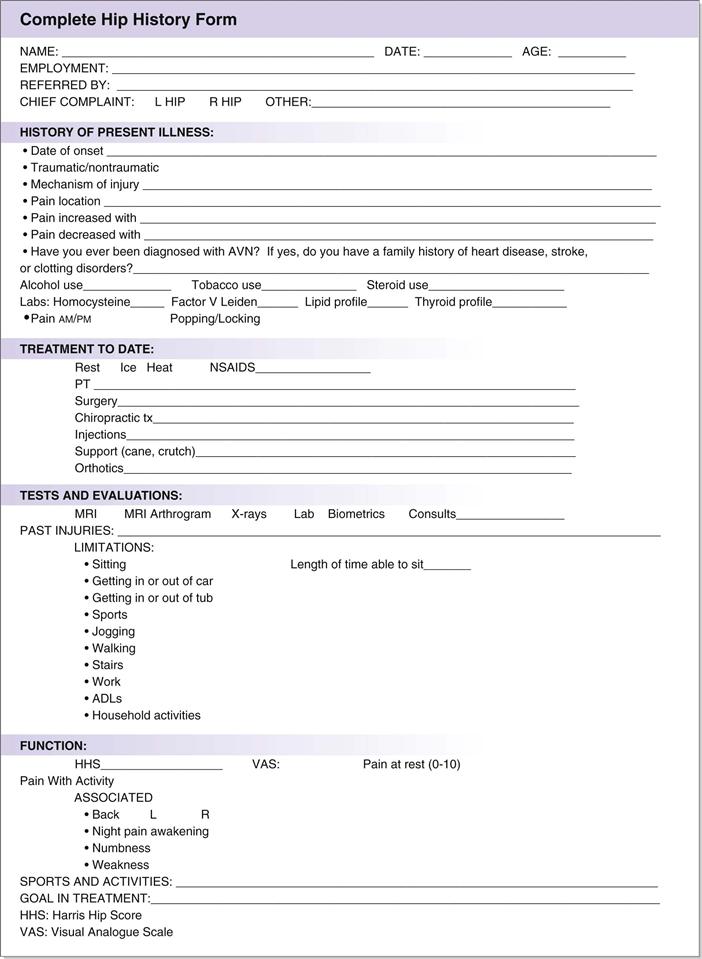
Figure 30-1 Complete hip history form.
Several questionnaires that provide quantitative and qualitative descriptions of a patient’s functional ability are available. The modified Harris Hip Score20 (HHS), the most documented and standardized functional score to date, is a quantitative score based on pain and function. Other hip scores that have been outlined with quantification in more specific patient populations include Merle d’Aubigné21 (MDA), the Non-Arthritic Hip Score22 (NAHS), the Musculoskeletal Function Assessment23 (MFA), Short Form-3624 (SF-36), and the Western Ontario and McMaster University Osteoarthritis Index (WOMAC).25 A verbal analogue score is also subjectively useful.
Physical Examination of the Hip
A consistent hip examination is performed quickly and efficiently to screen the hip, the back, and abdominal, neurovascular, and neurologic systems. It is important that physical examination of the hip is inclusive enough to rule out other joints as a dominant cause of complaint. The technique of physical examination is dependent on the examiner’s experience and efficiency. Interobserver consistency and practice account for some of the most important aspects of the evaluation.26 Figure 30-2 shows an example of a physical examination of the hip intake form.
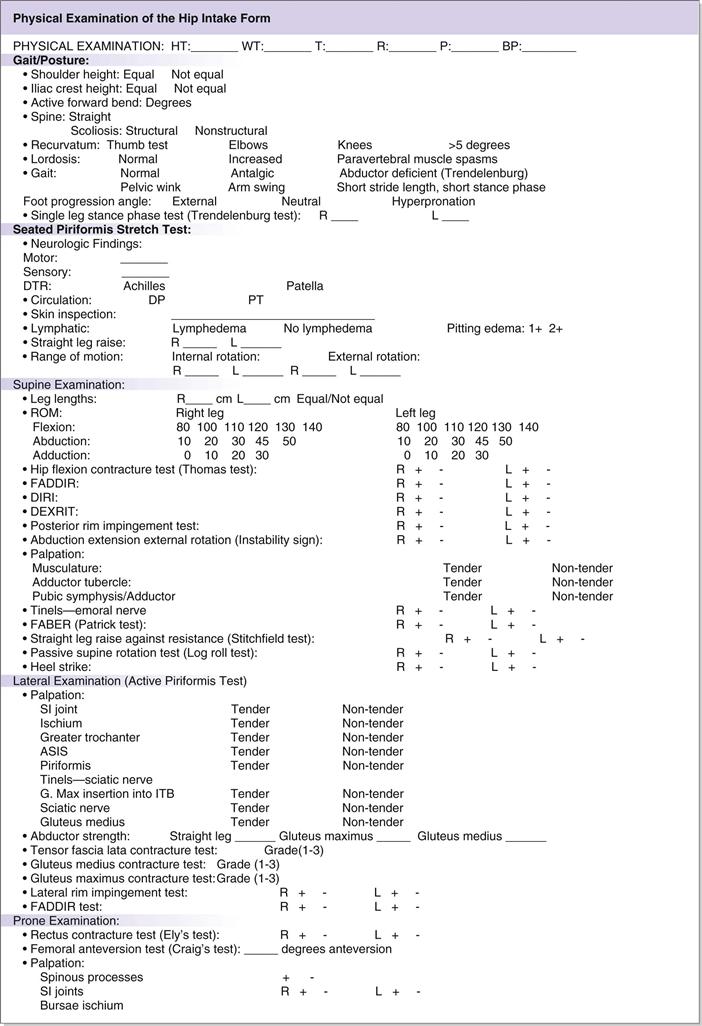
Figure 30-2 Physical examination of the hip intake form.
The physical examination consists of a variety of tests involving wide ranges of motion and palpation; therefore loose-fitting clothing about the waist is needed. A trained assistant provides accurate documentation by recording the examination on a written form. The order of the examination is designed to be easy on the patient and to flow for the physician; it begins with standing tests, which are followed by seated, supine, lateral, and prone tests. A comprehensive assessment requires scheduling adequate time with the patient. For international clarification among clinicians, each test is given a descriptive functional title.
Standing Examination
The general area of pain is noted by having the patient point with one finger. The groin region directs suspicion of an intra-articular problem, and laterally based pain is primarily associated with both intra-articular and extra-articular aspects. A characteristic sign of patients with hip pain is the “C sign.”26 The patient holds his or her hand in the shape of a C and places it above the greater trochanter, with the thumb positioned posterior to the trochanter and fingers extending into the groin.26 This can be misinterpreted as lateral soft tissue pathology such as trochanteric bursitis or the iliotibial band; however, the patient may often describe deep interior hip pain.26 Posterior-superior pain necessitates a complete evaluation for differentiating hip and back pain. Often, back issues are noted, along with musculotendinous hip pathology.7
As the patient stands (Table 30-1), general body habitus is assessed, and shoulder height and iliac crest heights are evaluated for leg length discrepancies. Placing incremental wooden blocks under the short-side heel will aid in orthotic considerations. Issues of ligamentous laxity are determined by the thumb test or by hyperextension of the elbows or knees. Forward bending allows assessment of spinal alignment and differentiation of structural versus nonstructural scoliosis. The degree of flexion at the waist is recorded, and side-to-side bending is helpful.
Table 30-1
Standing Examination Assessment
| Examination | Assessment/Association |
| Abductor deficient gait | Abductor strength, proprioception mechanism |
| Antalgic gait | Trauma, fracture, synovial inflammation |
| Pelvic rotational wink | Intra-articular pathology, hip flexion contracture, increased femoral anteversion, anterior capsular laxity |
| Foot progression angle with excessive external rotation | Femoral retroversion, increased acetabular anteversion, torsional abnormalities, effusion, ligamentous injury |
| Foot progression angle with excessive internal rotation | Increased femoral anteversion or acetabular retroversion, torsional abnormalities |
| Short leg limp | Iliotibial band pathology, true/false leg length discrepancy |
| Single-leg stance phase test | Abductor strength, proprioception mechanism |
| Spinal alignment | Shoulder/iliac crest height, lordosis, scoliosis, leg length |
| Laxity | Ligamentous laxity in other joints: thumb, elbows, shoulders, or knee |
An understanding of mechanical load transfer in the hip in both static and dynamic situations is essential for assessment and diagnosis of hip pathology. Comprehensive knowledge of normal gait will aid the physician in discriminating between normal and abnormal gait patterns. Abnormal gait patterns can indicate where abnormal transfer of load is applied across the hip joint; this can result in improper force load transfer to the lower back and knee joints.27 Irregularities in gait are derived most often by compensating for pain perceived in stride. The musculature of the lower limbs produces the forces required for ambulation, and the ligamentous capsule maintains hip stability.27 This relationship emphasizes the importance of adequate postoperative rehabilitation, especially with connective tissue disorders and improper osseous alignment.
Adequate space such as a hallway is needed, so that a full gait of six to eight stride lengths can be assessed. Gait evaluation includes observation of foot rotation (internal/external progression angle), pelvic rotation in the coronal and sagittal planes, stance phase, and stride length. The foot progression angle will indicate osseous or static rotatory malalignment, which occurs with increased or decreased femoral anteversion, versus a capsular or musculotendinous problem. Simultaneous observation of the knee and thigh is critical in assessment of rotatory parameters. Secondary abnormal hip rotation may be caused by holding the knee in internal or external rotation in an effort to maintain proper patellofemoral joint alignment. This abnormal motion or battle between the hip and the knee for a comfortable position will affect the gait; this is usually seen in cases of severe increased femoral anteversion. In cases of a painful gait, it is important to document the anatomic location of pain and the phase within the gait cycle during which pain is experienced. Pain alleviated with an abducted gait raises suspicion for the possibility of dysplasia.
Careful observation of iliac crest rotation and terminal hip extension will assess pelvic rotation. On average, normal gait requires 8 degrees of hip rotation and 7 degrees of pelvic rotation, equaling a total rotation of 15 degrees.28 Excessive rotation in the axial plane toward the affected hip is demonstrative of a pelvic wink. The pelvic wink produces extension and rotation through the lumbar spine to attain terminal hip extension. The winking gait can be associated with laxity or hip flexion contracture, which can be exacerbated by increased lumbar lordosis or a forward-stooping posture. Ischiofemoral impingement can also produce a lumbar pelvic flexion to gain hip extension. Spinal function and mechanics can be affected by gait abnormalities. In cases of excessive femoral anteversion, the patient will try to create greater anterior coverage with a rotated pelvis to achieve terminal hip extension. Anterior capsular injury or laxity can also attribute to a winking gait.
During the stance phase, body weight must be supported by a single leg, with the gluteus maximus, gluteus medius, and gluteus minimus providing the majority of support forces.27,28 Heel strike occurs at 30 degrees of hip flexion, thus generating maximum ground reactive forces to the hip.28 Neuromuscular abnormalities, trauma, and leg length discrepancies can be indicated by a shortened stance phase. Abductor weakness or disrupted proprioception can be attributed to abductor deficient gait (common nomenclature, Trendelenburg gait or abductor lurch). The abductor deficient gait is an unbalanced stance phase, which may present in two ways: a pelvic shift away from the body (“dropping out” of the hip on the affected side), or a weight shift over the adducted leg (shift of the upper body “over the top” of the affected hip). Antalgic gait, a self-protecting limp caused by pain, is characterized by a shortened stance phase on the painful side, limiting the duration of weight bearing. Differentiation of a short leg gait involves a drop of the shoulder in the direction of the short leg.
The single-leg stance phase test (traditionally known as the Trendelenburg test) is an assessment of hip joint function that simulates the single-leg stance phase with load on the examined hip. The single-leg stance phase test is performed bilaterally, with the nonaffected side examined first and serving as a baseline reference for the affected side (Fig. 30-3). The examiner observes the single-leg stance phase test from behind and in front of the patient, while carefully assessing the bony landmarks of the iliac crests, shoulder heights, knees, and ankles. The patient stands with feet shoulder width apart and brings one leg forward by flexing the leg to 45 degrees at the hip and 45 degrees at the knee. The single-leg stance phase position is held for 6 seconds. As the patient lifts and holds one foot off the ground, the contralateral hip abductor musculature and the neural loop of proprioception are being evaluated. If the musculature is weak, or if the neural loop of proprioception is disrupted, the pelvis will tilt toward or away from the unsupported side. Normal dynamic midstance translocation is 2 cm during a normal gait pattern,28 and a shift in either direction of greater than 2 cm constitutes a positive shift. This test is also performed in a dynamic fashion.

Figure 30-3 The single-leg stance phase test. The single-leg stance phase test is performed bilaterally and is observed from behind and in front of the patient. The patient holds this position for 6 seconds. A pelvic shift of greater than 2 cm is a positive, indicating abductor weakness or proprioception disruption. A, Right leg, front view. B, Left leg, front view (note the positive pelvic shift). C, Left leg, rear view.
Seated Examination
A thorough neurologic and vascular examination is performed during the seated hip examination (Table 30-2). Criteria for the care of the patient, as well as for coding, are available; therefore it is important to check the basics even in apparently healthy individuals.7 The posterior tibial pulse is checked first, any swelling of the extremity is noted, and inspection of the skin is performed at this time. A straight-leg raise test is performed by the examiner by passively extending the patient’s knee into full extension; this will detect any radicular neurologic symptoms, such as stretching of an entrapped nerve root.
Table 30-2
Seated Examination Assessment
| Examination | Assessment/Association |
| Neurologic | Sensory nerves originating from the L2-S1 levels, DTR of patella (L2-L4 spinal nerves and femoral nerve) and Achilles (L5-S1 sacral nerves) |
| Straight-leg raise | Radicular neurologic symptoms |
| Vascular | Pulses of the dorsalis pedis and posterior tibial artery |
| Lymphatic | Skin inspection for swelling, scarring, or side-to-side asymmetry |
| Internal rotation | Normal between 20 and 35 degrees |
| External rotation | Normal between 30 and 45 degrees |
DTR, Deep tendon reflex.
Loss of internal rotation is one of the first signs of the possibility of intra-articular disorder29–34; therefore one of the most important assessments is that of internal and external rotation in the seated position. The seated position ensures that the ischium is square to the table, thus providing sufficient stability at 90 degrees of hip flexion and a reproducible platform for accurate rotational measurement. Gently perform passive internal and external rotation until a firm endpoint or pain is involved, and compare bilaterally (Fig. 30-4). Seated rotation range of motion is also compared and contrasted with extended hip position during the prone examination.

Figure 30-4 Seated internal and external rotation range of motion. Passive internal and external rotation testing is compared from side to side. In the seated position, the ischium is square to the table, thus providing sufficient stability at 90 degrees of hip flexion. Internal and external rotation in the seated position offers a reproducible platform for accurate rotational measurement.
Musculotendinous, ligamentous, and osseous control of internal and external rotation is complex; therefore any differences in seated versus extended positions may raise the question of ligamentous versus osseous abnormality. For proper hip function, sufficient internal rotation is needed. At the midstance phase of normal gait should be at least 10 degrees of internal rotation; however, less than 20 degrees is poorly tolerated for normal activity. Diagnoses such as arthritis, effusion, internal derangement, slipped capital femoral epiphysis, femoroacetabular impingement, and muscular contracture can be related to loss of internal hip rotation.7 Significant side-to-side differences can be related to femoroacetabular impingement or to rotational constraint from increased or decreased femoral acetabular anteversion. Increased internal rotation combined with decreased external rotation may indicate excessive femoral anteversion, although hip capsular function will require further radiographic and biometric assessment.14,35
Supine Examination
The supine position (Table 30-3) helps to further distinguish internal from extra-articular sources of hip symptoms. The supine position allows assessment of any leg length discrepancies with the hip in an unloaded state. Passive hip flexion range of motion is assessed as both knees are brought up to the chest, and the degree of flexion is recorded (Fig. 30-5). It is important to note the pelvic position, as the hip may stop early in flexion with the end range of motion being predominantly pelvic rotation. From this position, the hip flexion contracture test (also known as the Thomas test) is performed by having the patient extend and relax one leg down toward the table. Any lack of terminal hip extension, noted by inability of the thigh to reach the table, demonstrates a hip flexion contracture. Both sides are assessed for comparison of the difference. An important aspect of the hip flexion contracture test is obtaining the zero set point for the lumbar spine. Patients with hyperlaxity or connective tissue disorder could receive a false negative. In these patients, the zero set point can be established with an abdominal contraction. The hip flexion contracture test could be falsely negative if lumbar spine hyperlordosis due to previous spinal fusion is present.
Table 30-3
Summary of Supine Examinations and Assessment
| Examination | Assessment/Association |
| Range of motion | Flexion, abduction, adduction |
| FADDIR | Anterior femoroacetabular impingement, torn labrum |
| Hip flexion contracture test (Thomas test) | Hip flexor contracture (psoas), femoral neuropathy, intra-articular pathology, abdominal origin |
| FABER (Patrick/Faber) | Distinguish between back and hip pathology, specifically, sacroiliac joint pathology |
| Dynamic internal rotatory impingement test (similar to McCarthy test) | Anterior femoroacetabular impingement, torn labrum |
| Dynamic external rotatory impingement test (similar to McCarthy test) | Superior femoroacetabular impingement, torn labrum |
| Posterior rim impingement test | Posterior femoroacetabular impingement, torn labrum |
| Passive supine rotation test (log roll) | Trauma, effusion, synovitis |
| Heel strike | Trauma, femoral fracture |
| Straight-leg raise against resistance (Stitchfield) | Hip flexor strength |
| Palpation | |
| 1. Abdomen | Fascial hernia, associated Gastrointestinal/genitourinary pathology |
| 2. Pubic symphysis | Osteitis pubis, calcification, fracture, trauma |
| 3. Adductor tubercle | Adductor tendinitis |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








