Chapter 97 Historic Development, Classification, and Characteristics of Knee Prostheses
Early Prosthetic Models
Interposition and Resurfacing Prostheses
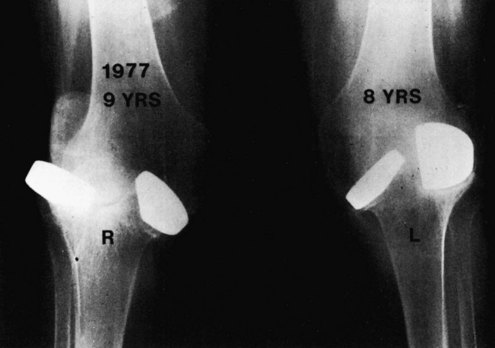
The concept of improving knee joint function by modifying the articular surfaces has received attention since the 19th century. In 1860, Verneuil295 suggested the interposition of soft tissues to reconstruct the articular surface of a joint. Subsequently, pig bladder, nylon, fascia lata, prepatellar bursa, and cellophane were some of the materials used for this purpose. The results were disappointing. In 1860, Ferguson82 resected the entire knee joint, which resulted in mobility of the newly created subchondral surfaces (Fig. 97-1). When more bone was removed, the patients enjoyed good motion but lacked the necessary stability, whereas with less bone resection, spontaneous fusion often resulted. These early attempts were usually performed on knees damaged by tuberculosis or other infectious processes, along with concomitant ankylosis and deformity. The results of this procedure were sufficiently poor to discourage anything more than occasional attempts in severe cases.
Encouraged by the relative success of hip cup arthroplasty, Campbell50 reported the successful use of a metallic interposition femoral mold in 1940. A similar type of arthroplasty was developed and used at Massachusetts General Hospital. The results, published by Speed and Trout280 in 1949 and by Miller and Friedman209 in 1952, were not very good, and this type of knee arthroplasty never achieved wide recognition.
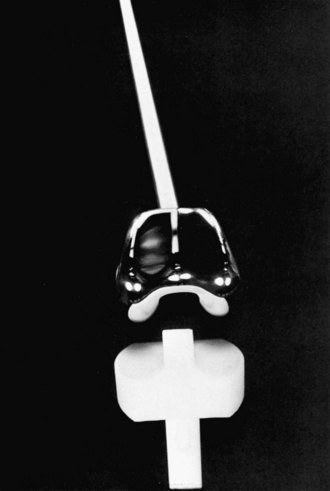
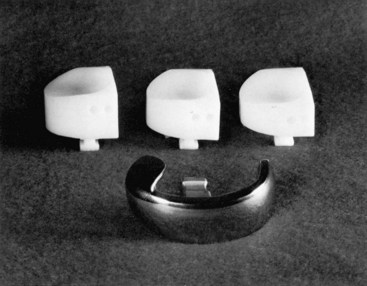
In 1958, MacIntosh191 described a different type of hemiarthroplasty that he had used in treating painful varus or valgus deformities of the knee. An acrylic tibial plateau prosthesis was inserted into the affected side to correct deformity, restore stability, and relieve pain. Later versions of this prosthesis190 were made of metal (Fig. 97-2), and the somewhat similar McKeever prosthesis75,205,253 showed considerably more success and was extensively used, particularly in patients with rheumatoid arthritis. Gunston113 carried MacIntosh’s ideas a step further and, instead of using a simple metal disk interposed within the joint, substituted metallic runners embedded in the femoral condyles that articulated against polyethylene troughs attached to the tibial plateau. To make a four-part system of this type feasible, it was necessary to find a means of fixing the components rigidly to the bone. The solution was provided by acrylic cement.
Although the Gunston polycentric prosthesis113 was the first cemented surface arthroplasty of the knee joint, the work of Freeman and colleagues90,97 has had an even greater influence on the direction of both prosthetic design and surgical technique. The design objectives for a prosthesis (Fig. 97-3) were outlined in 1973 by Freeman and colleagues.97 The most important of these objectives are the following:
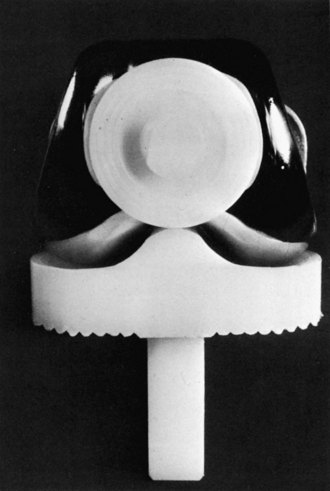
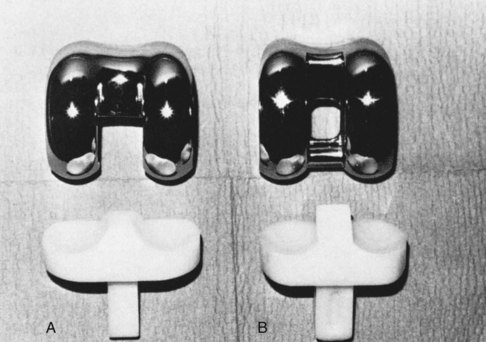
Other early examples of resurfacing prostheses (Figs. 97-4 and 97-5) were the Geometric,61,62,292 Duocondylar,234,274 UCI (University of California at Irvine),308 and Marmor.197–201
Constrained Prostheses
A second line of development in knee arthroplasty occurred parallel to the concepts of interposition and, later, surface replacement. In 1951, Walldius302 developed the hinged prosthesis that bears his name. The device was initially made of acrylic and later of metal.
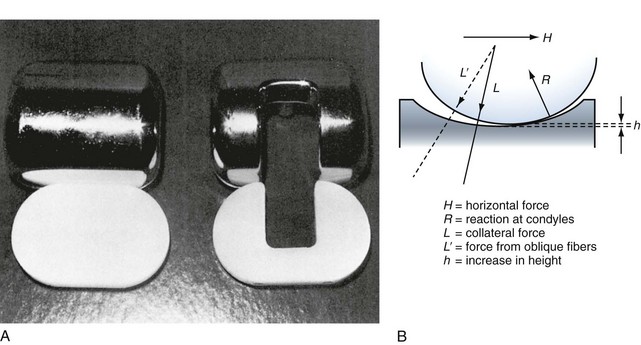
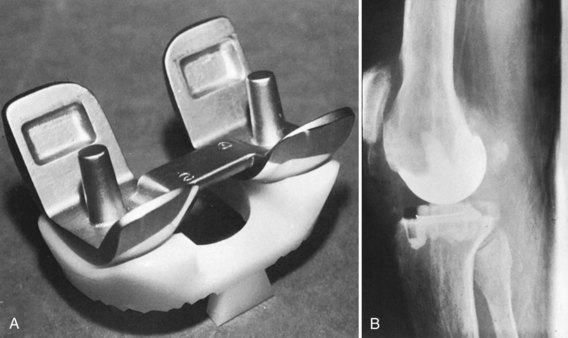
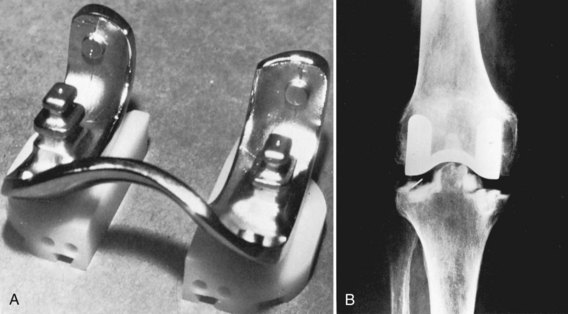
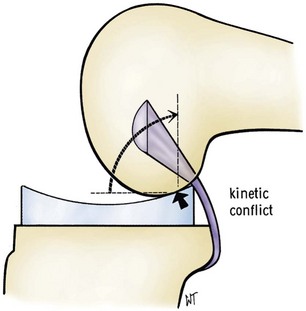
Shortly thereafter, Shiers266 described a similar device with even simpler mechanical characteristics (Fig. 97-6). A hinged prosthesis has considerable appeal. Technically, it is easy to use because the intramedullary stems make the prosthesis largely self-aligning and all the ligaments and other soft tissue constraints can be sacrificed because the prosthesis is self-stabilizing. The extent of damage to the knee is therefore of no consequence, and even the most extreme deformities can be corrected by dividing the soft tissues and resecting sufficient bone. Of course, the early hinged designs were uncemented, although later developments such as the GUEPAR (Fig. 97-7) were designed from the outset to be used with methylmethacrylate cement. Because of inherent limitations with a simple hinge, including limited range of motion and transmission of stress to the prosthesis-cement interface, the early hinged prostheses were supplanted by rotating hinge devices that constrain the prosthesis in the coronal and sagittal planes, but allow rotation in the axial plane. Early designs included the Spherocentric (Fig. 97-8) prosthesis; current models include the Zimmer Rotating Hinge Knee and the DePuy SROM-Noiles prosthesis. In cases in which the maximal constraint offered by a linked hinge is not required, unlinked but constrained devices have been extensively used in revision and complex primary TKR. Historical devices include the Total Condylar Prosthesis III (TCP III; Fig. 97-9)68 and the Constrained Condylar Knee (CCK)168; their modern counterparts include the DePuy PFC Sigma TC3 and Zimmer Legacy Constrained Condylar Knee (LCCK). The primary characteristic of these devices is a cam and post mechanism, similar to that found in a posterior-stabilized (PS) prosthesis, but thicker and taller, and it provides resistance not only to posterior translation but also to varus and valgus stress. At the present time, the use of cemented or uncemented stems with both hinged and constrained but unlinked devices is based on surgeon preference.
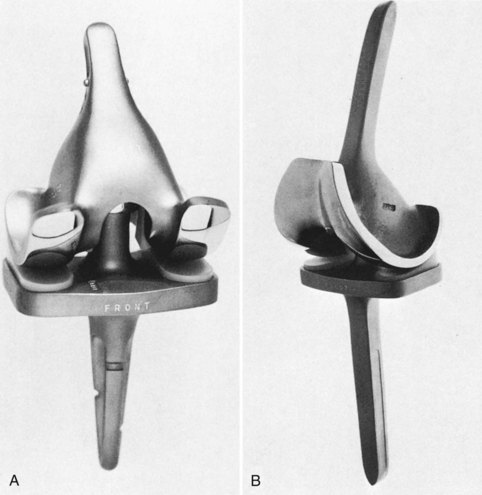
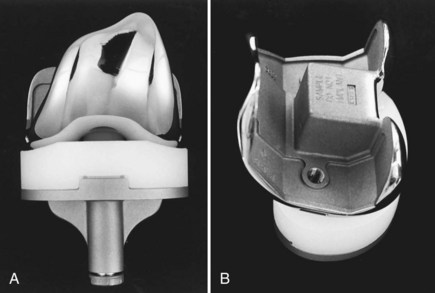
Figure 97-8 Spherocentric prosthesis. A, Standard version. B, Long-stemmed variant with a patellar flange.
(Courtesy Dr. H. Kauffer and Dr. L.S. Matthews.)
Evolution of Prosthetic Design
The prostheses discussed up to this point are now more or less obsolete. Although the early results were encouraging, further follow-up demonstrated various problems. The literature relevant to TKR includes many articles that report the clinical results of designs no longer in common use.*
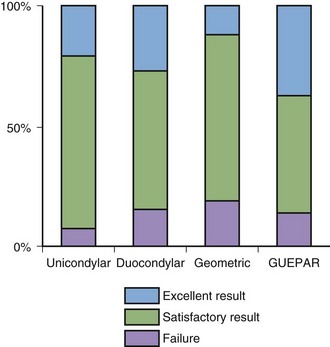
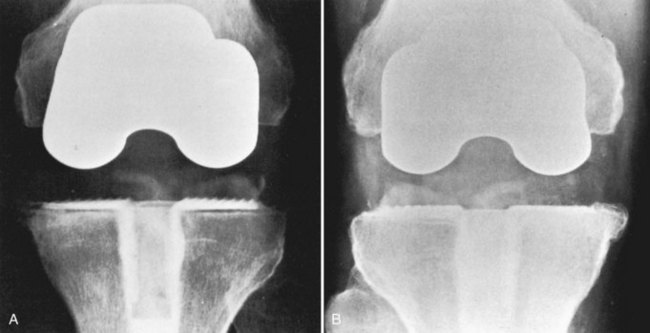
These published reports on early models are somewhat difficult to compare because different rating methods were used. A review conducted at the Hospital for Special Surgery (HSS) between 1971 and 1973 is probably representative. This review136 compared four different models (Fig. 97-10): the unicondylar (Fig. 97-11), Duocondylar, Geometric, and GUEPAR (see Fig. 97-7). The results were expressed by using the HSS 100-point knee rating scale.
Postoperative knees were classified into four groups according to their scores on the HSS scale:
Considering the entire group of 178 arthroplasties studied in the four different models (23 unicondylar, 60 Duocondylar, 50 Geometric, and 45 GUEPAR), the results were considered excellent in 47 (26%), good in 66 (37%), fair in 37 (21%), and poor in 28 (16%; Fig. 97-12). There was no statistically significant difference among the results obtained with each of the four prostheses studied. However, because it is easier to improve a bad knee than a relatively good one, the percentage of improvement was much greater with the GUEPAR than with the unicondylar (120% versus 45%).
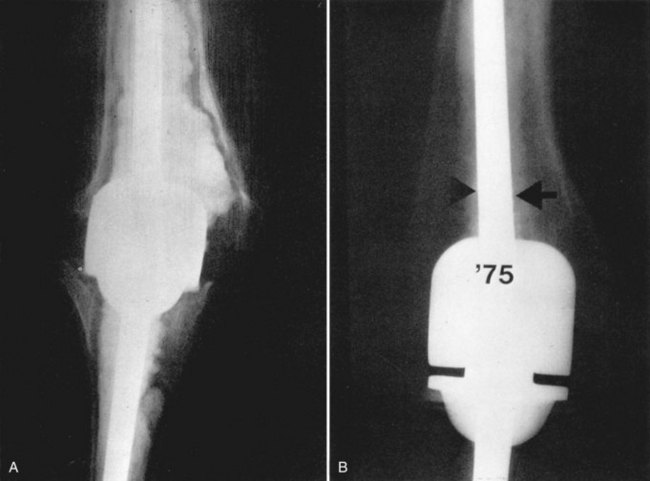
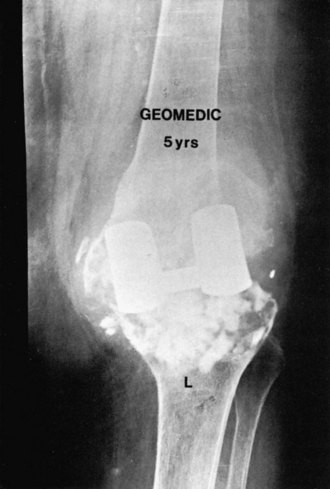
Three specific problems were identified from this study: patellar pain, component loosening, and surgical technique. However, because the GUEPAR hinge was inserted into the worst knees originally, it gave the greatest percentage of improvement in the HSS knee rating scale. At the time of the study, the conclusion reached was that the GUEPAR prosthesis appeared superior in a number of ways. It had been selected for use in the most severely involved knees and yet equaled any of the other prostheses in the quality of results in rheumatoid arthritis and osteoarthritis. It also gave the lowest proportion of failures and was the only model to improve range of motion postoperatively. However, the potential problems of loosening and mechanical failure with the GUEPAR prosthesis were noted. More than 100 GUEPAR prostheses were used at the HSS almost 40 years ago, and these expected problems materialized to a large extent. Approximately 80% of the prostheses were loose clinically and radiographically at long-term follow-up, although they are not necessarily symptomatic (Fig. 97-13A). There were also numerous cases of stem breakage (see Fig. 97-13B) and, as noted later, infection became a major problem. This study therefore reached some erroneous conclusions because of short follow-up—a point of great relevance today when many new prostheses are being used in patients with scant clinical follow-up to support their merits.
Patellar Pain
None of the four early prosthetic models studied made any provision for patellofemoral function. Patellectomy did not seem to offer a solution to the problem of patellofemoral arthritis (Fig. 97-14). In our early study, 38 patellectomies were performed in the group as a whole, 3 of which were done at a later date than the arthroplasty because of persistent patellar pain. Importantly, pain after patellectomy was as frequent as in patients in whom patellectomy had not been performed. In addition, patients who underwent patellectomy suffered from inadequacy of the extensor mechanism. In the GUEPAR group of 45 knees, pain on patellar compression was found in 22 on follow-up, and patellar erosion was observed in 5 patients. Patellar subluxation frequently occurred with the GUEPAR prosthesis, despite wide lateral release of the patellar retinaculum at the time of arthroplasty (Fig. 97-15). Nonetheless, the subluxation was often not apparent to the patient and was considered an incidental finding. Subluxation of the patella did not necessarily correlate with complaints of postoperative pain. However, with the Geometric prosthesis, 29 of 50 knees had pain on patellofemoral compression. Patellar subluxation was found in nine knees and all were painful.
Loosening
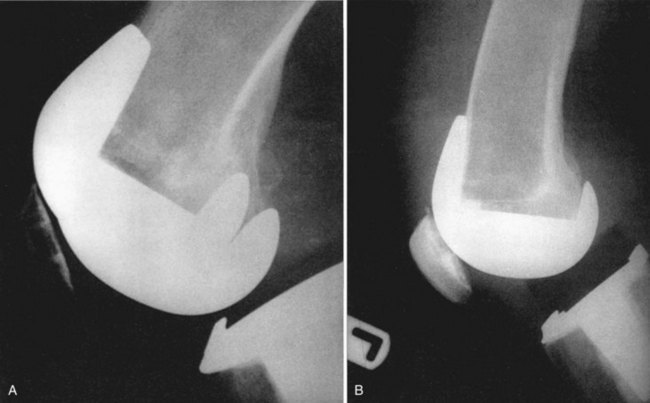
A radiolucent line surrounding the prosthetic components was seen with great frequency. With the condylar replacements, the radiolucency was usually observed around the tibial component. It was present in 70% of knees with the unicondylar, 50% with the Duocondylar, and 80% with the Geometric prosthesis. A radiolucent line was observed around the femoral component in 45% of the patients with a GUEPAR prosthesis. The radiolucent line was slightly more frequent in patients with osteoarthritis than in those with rheumatoid arthritis and it was observed in all knees with osteoarthritis in which the Geometric prosthesis was used. Radiolucent lines are by no means always symptomatic, but when complete, progressive, and associated with pain on weight bearing, they generally indicate failure of fixation. Our subsequent experience has shown that the incidence of partial radiolucencies for a particular prosthesis does not correlate with the eventual amount of component loosening. On the strength of a 10- to 12-year follow-up on one particular cemented prosthesis (the Total Condylar), we concluded that a detailed study of partial radiolucent lines about cemented knee replacements is worthless and a poor predictor of future failure (Fig. 97-16).
On the basis of early analysis of these data, it was clear that tibial loosening represented a failure in prosthetic design. The flat cancellous surface of the upper part of the tibia is not a suitable bed for a flat prosthetic component because of poor resistance to shear stress. Moreover, this bone is not of sufficient strength to resist subsidence of the tibial component, even if excavations are made to accommodate fixation fins or lugs on the bottom of the tibial prosthesis (Figs. 97-17 and 97-18). It was concluded that some form of cortical fixation would be essential for a successful TKR series.
Prosthesis Selection and Surgical Technique
Like many others, we initially believed in the concept of a graduated system, in which selection of a prosthesis depended on the severity of damage found in the arthritic knee (see Fig. 97-10). For example, knees with cartilage erosion restricted to one femorotibial compartment were replaced with a unicondylar prosthesis, whereas a hinged prosthesis was used in the most severely damaged and deformed knees. The bicondylar prosthesis occupied an intermediate position with respect to the severity of arthritis. Although the use of a hinged prosthesis is not technically demanding, the early condylar designs were difficult to insert and align, and there was very little margin for error. Obviously, the advantage of even the most sophisticated prosthetic design is lost if surgical placement is incorrect. Furthermore, an inherent drawback in a graduated system of prostheses is that a model may be used for degrees of deformity exceeding the limits for which the prosthesis was intended. This error can itself be a cause of failure (e.g., dislocation; Fig. 97-19). Clearly, there is no purpose in selecting one prosthetic design over another unless some advantage can be shown. For example, in our comparative study, we did not find that the unicondylar prosthesis offers any advantage over bicondylar models. The merits of graduated knee systems still remain a source of debate.
Infection
Although deep periprosthetic infection was not a frequent cause of failure for the condylar designs, it has subsequently proved to be a major problem with the GUEPAR prosthesis. With further follow-up, 15 of 108 prostheses (14%) became infected (4 early and 8 late). There have been reports of similar occurrences in the literature.12
At the HSS, dissatisfaction with the early prostheses led to the design of the Total Condylar and Duopatellar prostheses, which were based on different concepts of how to manage the posterior collateral ligament (PCL).232,245,252 During the 1980s, prosthetic characteristics diverged further and were generally linked to whether the prosthesis was designed to substitute for or preserve the PCL. However, during the 1990s, there was a convergence of prosthetic designs, particularly in the United States.
Types of Prostheses
Most simply, a prosthesis can be a surface replacement or a constrained design. These two categories may be further subdivided. Surface replacements comprise unicondylar and bicondylar designs. Unicondylar prostheses are discussed elsewhere in this text.*
Early Surface Replacement Designs
In the following sections, we discuss early surface replacement designs.298 Supplemental information about the individual innovators and the tremendous advances in TKR during the early years of the modern era can be found in the three historical reviews by Robinson,245 Ranawat,232 and Scott252 that should be compulsory reading for all students of knee arthroplasty. Much of the early debate about prosthesis design and the techniques used to implant the components, including how to address the cruciate ligaments, arose from conceptual differences among the pioneers about whether it was better to design a knee prosthesis from an anatomic or functional perspective. The current generation of prostheses has converged in many ways, with most designs incorporating characteristics from each category that seem to have optimized long-term outcomes—for example, side-specific femoral components with optimized trochlear geometries from the anatomic approach and the moderately conforming coronal and sagittal geometry that was more associated with the functional approach.
Total Condylar Prosthesis
Although originally coined as the name of a specific prosthesis, the term total condylar prosthesis has been used generically to describe a whole range of surface replacement prostheses that share general characteristics with the original (Fig. 97-20).*
The TCP, designed in 1973, was a true total replacement of the knee in that the patellofemoral joint was replaced as well as the femorotibial compartment. Designed from a functional perspective, the inherent geometry of the prosthesis was intended to substitute for the anatomic function of the cruciate ligaments, native articular geometry, and menisci. The salient features of the design are discussed in the following sections.245
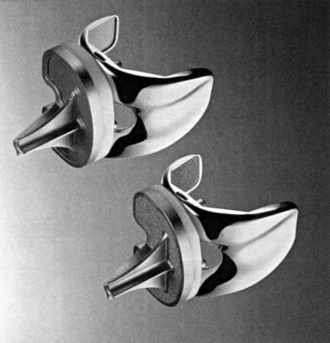
Duopatellar Prosthesis
The Total Condylar Prosthesis was designed for cruciate excision. In contrast, the Duopatellar prosthesis,81 a sibling prosthesis designed from an anatomic perspective at the HSS as a replacement for the Duocondylar model, was intended to preserve existing cruciate ligaments, particularly the PCL.232,245,252 The general shape of the tibial runners was anatomic in the sagittal plane. Coronally, the condyles were flat with a median curvature.
Cruciate Excision, Retention, and Substitution
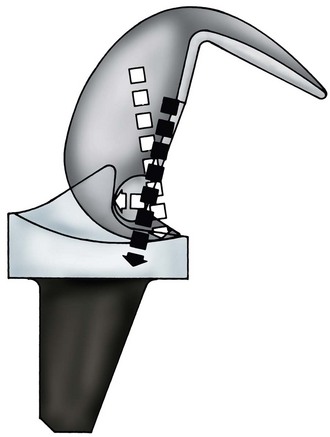
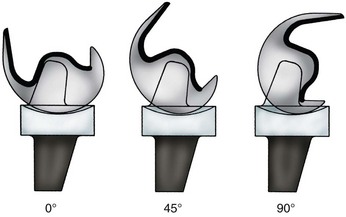
The TCP and Duopatellar prosthesis were designed for cruciate excision and retention, respectively.7,10,69,92,96 Subsequent modifications to the TCP incorporated a cam on the femoral component and a central post on the tibial polyethylene (Fig. 97-21). This cam and post mechanism was designed to act as a functional substitute for the PCL and produce femoral rollback during flexion. With the development of this so-called posterior-stabilized prosthesis, it was apparent that cruciate excision alone was not optimal. However, the relative merits of PCL retention versus PCL substitution have been debated vigorously within the orthopedic community for many years. The development of total knee prostheses has occurred along two distinct evolutionary paths based on these different principles.245 The anatomic function of the cruciate ligaments, relative advantages and disadvantages of cruciate excision, and PCL retention versus PCL substitution will be reviewed here. It has also become clear that if the PCL is retained, the function of the ligament must be optimized through a balancing technique. Difficulties with balancing the PCL, as well as late PCL rupture leading to flexion instability, have led to the development of the so-called deep dish polyethylene inserts that are offered as part of many cruciate-retaining prosthesis systems. These inserts have moderately conforming articular surfaces in the coronal and sagittal planes, together with an anterior lip that limits paradoxical anterior translation of the femur on the tibia. This is one example of how prosthesis design has converged in the past 2 decades, thus making it more difficult to trace the origins of any particular design.
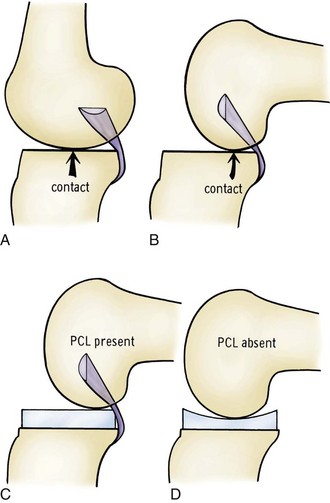
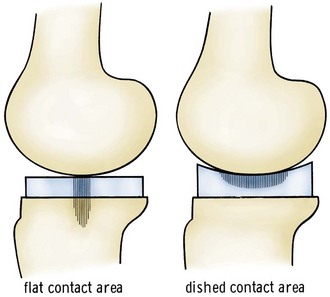
Anatomic Functions of the Cruciate Ligaments
One function of the cruciate ligaments, in addition to providing static anterior and posterior stability, is to impose certain movements on the joint surfaces relative to one another. The anterior cruciate ligament (ACL) is often absent in arthritic knees and has not been thought to be of much consequence in TKR. The importance of the ACL may have been underestimated inasmuch as unconstrained prostheses have increased sagittal plane laxity and fail more often when the ACL is absent.313 Although the PCL is often attenuated in arthritic knees, it is usually present. It has been considered the collateral ligament for the medial compartment of the knee.74 The PCL causes the femoral condyles to glide and roll back on the tibial plateau as the knee is flexed.149 In a normal knee, the shape of the plateau does not restrain this motion and the laxity of the meniscal attachments allows the menisci to move posteriorly with the femur. This femoral rollback is crucial in prosthetic design. If the cruciates are excised, a more conforming tibial polyethylene component can be used to provide some degree of anterior and posterior stability. However, without the function of the PCL, femoral rollback will not occur, which theoretically limits the ultimate flexion that can be obtained. If the PCL is retained, the tibial surface must be flat or even sloped posteriorly (Fig. 97-22). If a more conforming component is used in these circumstances, posterior impingement will occur (Fig. 97-23). Substitution of the PCL with a cam and post mechanism not only re-creates femoral rollback but also allows a conforming articulation to be used without risk of posterior impingement. These considerations were reflected in the design of the Total Condylar, Duopatellar, Posterior-Stabilized, and various PCL-retaining (cruciate-retaining [CR]) prostheses.
Arguments for and Against Cruciate Excision
Arguments can be made in favor of and against cruciate excision, and will be presented here.
Posterior Cruciate Ligament Retention versus Substitution
Kinematics
Retention of the PCL was initially believed to allow preservation of normal knee kinematics after TKR. In particular, preservation of the normal femoral rollback caused by tightening of the PCL, which acts to move the tibiofemoral contact point posteriorly during flexion, thereby increasing quadriceps efficiency and range of motion, was thought to be critical in activities such as stair climbing. The natural PCL was initially perceived to be better in performing this kinematic function than the cam and post mechanism used in PS knee prostheses. However, fluoroscopic studies by Stiehl and coauthors285 and Dennis and colleagues65 have demonstrated that CR prostheses do not replicate the kinematics of the normal knee. Instead, in many cases, a paradoxical roll forward of the femur occurs with anterior translation of the tibiofemoral contact area. This motion, which is the direct opposite of normal knee kinematics, may result from improper tension of the PCL (Fig. 97-24). Adverse consequences may include decreased flexion, reduced quadriceps efficiency, and posterior tibial polyethylene wear. In addition, Dennis and associates65 have demonstrated that although PS prostheses do not completely reproduce normal knee kinematics, reliable rollback does occur. Surgeons who advocate the use of CR prostheses have emphasized the importance of balancing the PCL with techniques such as PCL release and recession.244,255 However, the success of using these techniques to restore normal knee kinematics has still not been proven.
Range of Motion
Early experience with use of the cruciate-sacrificing TCP produced flexion of about 90 to 95 degrees, which is near the theoretical limit for this type of prosthesis. Improved flexion with PS and CR prostheses has been reported. Pooled data from numerous studies have demonstrated mean flexion of approximately 100 to 115 degrees with both types of prostheses.24,220 Again, the importance of PCL recession and balancing in helping to produce optimal results with CR prostheses has been advocated.244,255 With careful surgical technique, reliable flexion of 110 to 115 degrees should be obtainable with either type of prosthesis. However, because of the experience and attention that seem to be required to tension the PCL correctly, we believe that the PS prosthesis is less technically challenging and produces more consistent results. The consequences of inadequately tensioning the PCL have been reported. Arthroscopic release of a tight PCL seems to be successful in improving flexion for select patients with PCL-retaining prostheses.318
Modifications to the latest generation of PS prostheses, the Zimmer Nex Gen Legacy PS (LPS; Fig. 97-25), which is directly descended from the original Insall-Burstein Posterior-Stabilized (IB PS) knee, and before that the TCP, included redesign of the trochlea to accommodate the natural patella. This change necessitated posterior translation of the cam and post mechanism. As a result, the cam engages the post at approximately 70 degrees and then rides down the post, before eventually moving up the post with extreme flexion. This modification effectively increased the jump distance, thereby allowing greater flexion before dislocation. Further evolution of this device has included modifications to the posterior condyles to optimize the contact area in high flexion, as well as anterior scalloping of the polyethylene to reduce impingement on the extensor mechanism anteriorly. These changes have resulted in a new type of high flexion prosthesis, the Zimmer Nex Gen LPS Flex-Fixed, which is intended for use in patients with good preoperative motion in whom high postoperative flexion is anticipated (Fig. 97-26). Improvements in surgical technique, such as restoration of the posterior condylar offset and resection of posterior osteophytes, have also been emphasized in these cases to maximize postoperative motion. Similar design modifications have been made to other PS knee prostheses that are also intended for the high-flexion environment above 130 degrees, such as the Smith & Nephew Genesis II-HF, DePuy PFC Sigma PS and Biomet Vanguard PS prostheses, as well as to CR prostheses, such as the Zimmer Nex Gen CR Flex-Fixed.
Proprioception
Both cruciate ligaments contain mechanoreceptors, and therefore advocates of PCL retention have proposed that preserving the natural ligament would lead to superior proprioception after TKR. However, the current literature has not demonstrated a clear advantage. Simmons and associates271 were unable to identify any advantage in proprioception in patients who had a CR prosthesis versus those with a PS prosthesis. Warren and coworkers305 noted slightly different results. After TKR, all patients experienced improved proprioception regardless of whether a CR or PS prosthesis had been used. However, the improvement was greater in patients with a CR prosthesis. The improved proprioception in both groups was speculated to be caused by elimination of pain, restoration of articular congruity, and retensioning of the collateral ligaments and soft tissues. These inconclusive results may be to the result of the inherent qualities of the PCL in patients with arthritic knees. Kleinbart and colleagues162 have observed significant degenerative changes in the PCLs of patients with arthritic knees that exceed those in age-matched controls. Therefore, a PCL that is preserved in a patient with a CR prosthesis is likely to be abnormal and should not be expected to function normally, either biomechanically or proprioceptively. The effects of PCL recession on the proprioceptive function of the ligament are not known.
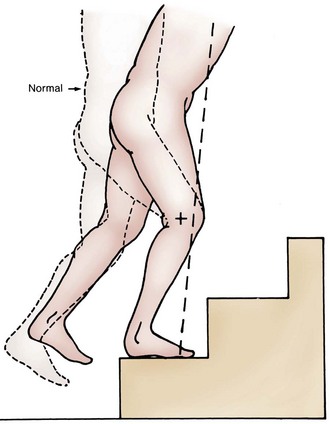
Gait Analysis
Initial studies suggested that the mechanics of walking and stair climbing, in particular, is different in patients with CR and PCL-substituting prostheses.7,155 Andriacchi and colleagues7,9 have described a characteristic forward lean of the trunk with less knee flexion in patients with PCL-substituting prostheses during stair climbing when compared with patients with PCL-retaining prostheses (Fig. 97-27). This observation was suggested to represent a compensatory mechanism for the absence of the PCL. However, gait analyses in two studies have disputed these findings. Bolanos and coworkers33 were unable to identify any significant differences in spatiotemporal gait parameters or knee range of motion during level walking or stair climbing in patients with CR or PS prostheses. Wilson and colleagues320 also did not identify any differences in these parameters during stair climbing between patients with PS prostheses and normal age-matched controls. However, differences between patients after TKR and controls were identified during level walking and descending stairs. This evidence suggests that although gait patterns after TKR are different from those in normal controls, there is no clear effect of prosthesis type.
Correction of Deformity
Patients with significant preoperative fixed varus, valgus, or flexion deformities can be successfully managed with the use of CR prostheses. However, because the PCL is one deforming factor in these cases, careful balancing with PCL release or recession may be required to achieve flexion and extension space symmetry.87,244,255 Balancing of the PCL may be difficult and is experience-dependent. The development of deep dish polyethylene inserts for use in cruciate-retaining prostheses when the PCL is impossible to tension accurately reflects the difficulties in accomplishing this task. Laskin178 has reported inferior results in patients with fixed varus deformities exceeding 15 degrees in whom CR rather than PS designs were used. In most circumstances, we believe that the use of a PS prosthesis is technically less challenging and allows more reliable correction of the preoperative deformity. Failure to tension the PCL appropriately may lead to reduced flexion or flexion instability.221,307,318
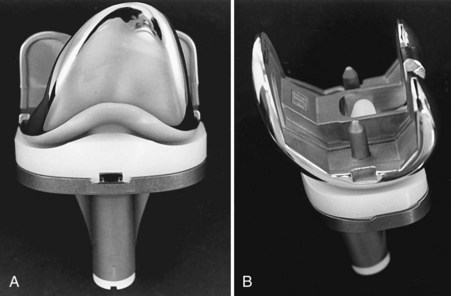
Stability
The more conforming tibial insert and cam and post mechanisms of PS prostheses do not provide any constraint in the medial-lateral directions (Fig. 97-28). Neither the CR nor the PS prosthesis is designed to compensate for instability in this plane and therefore requires intact collateral ligaments. In the anterior and posterior directions, the inherent characteristics of the designs are different, and different problems are encountered if flexion-extension balance is not achieved. As noted, a less conforming tibial polyethylene insert should be used in CR prostheses because of the kinematic conflict that results during femoral rollback in flexion if a more conforming insert is used. If the PCL is functionally incompetent or stretches, posterior instability may occur because the minimally conforming or flat insert does little to prevent posterior translation of the femur. The phenomenon of symptomatic flexion instability in patients with CR prostheses as a result of an incompetent PCL has now gained more widespread recognition.221,307 The consequences of overtensioning of the PCL have been discussed earlier. Biomechanical studies have suggested that it is difficult to obtain the appropriate tension in the PCL.129,193 However, the results of techniques used to balance the PCL have not been directly evaluated.
Although PS prostheses eliminate the PCL as a factor in preventing adequate flexion-extension balancing, anterior and posterior instability can still occur. In some patients with significant flexion instability, the jump distance of the cam and post mechanism may be exceeded during extreme flexion and acute dislocation results (Fig. 97-29). In previous series, a dislocation rate of 2% to 3% was reported.66,235 In one series, changes in design of the cam and post mechanism eliminated subsequent dislocations over a 2-year period.235 Because of the uncertainties in achieving optimal tension in the PCL, we believe that PS prostheses produce more reliable long-term anterior-posterior stability.
Polyethylene Wear
Polyethylene wear in current PS designs that have moderately conforming articular surfaces has not been a major clinical problem in older, less active patients.58,235 In contrast, the higher contact stress encountered in the unconstrained flat-on-flat articulations, in conjunction with the heat-pressed, thin polyethylene inserts used in CR prostheses during the 1980s, led to documented rapid wear.31,76,157,291 Failure to balance the PCL may also result in severe posteromedial polyethylene wear. Based on these results, the more conforming surfaces of PS implants seem better suited to optimizing long-term wear (Fig. 97-30).
Loosening
The increased constraint imposed by the moderately conforming articular surfaces of PS prostheses was initially considered to be detrimental to long-term fixation at the cement-bone-prosthesis interface because of increased stress transmission versus the relatively less conforming CR prostheses. However, with proper design, this shear stress can be altered to forces that are compressive (Fig. 97-31).
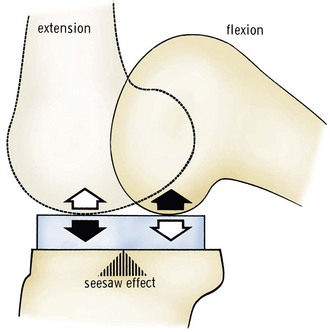
A theoretical seesaw motion may occur in CR prostheses (Fig. 97-32). The rolling motion of the femur changes the metal-plastic contact point from anterior in extension to posterior in flexion. Thus, in extension, the anterior portion of the tibia is compressed and in flexion the situation is reversed. This alternating compression-distraction may theoretically affect long-term fixation.
Long-term follow-up studies have failed to identify a significant clinical problem caused by these theoretical concerns, with only rare cases of aseptic loosening with both types of prosthesis. In the senior author’s (JI) experience with posterior-stabilized prostheses, no cases of aseptic loosening of the tibial component and only two cases of femoral component loosening have occurred in 165 primary TKRs at a mean of 10-year follow-up.58 These results are similar to those obtained with CR designs. Malkani and associates194 from the Mayo Clinic have reported a 96% survival rate at 10-year follow-up. In summary, at 10- to 15-year follow-up, there is little evidence to suggest that PS prostheses have an increased risk of aseptic loosening.
Current Prosthesis Design
Fixed-Bearing, Surface Replacement Prostheses
Traditional Cruciate-Retaining and Posterior-Stabilized Prostheses
The prostheses described in the preceding sections have given rise to derivatives (Fig. 97-33). The TCP led to a series of PS prostheses initially developed by Insall and Burstein, including the IB PS prosthesis, and modular IB II (IB II PS) prosthesis.*
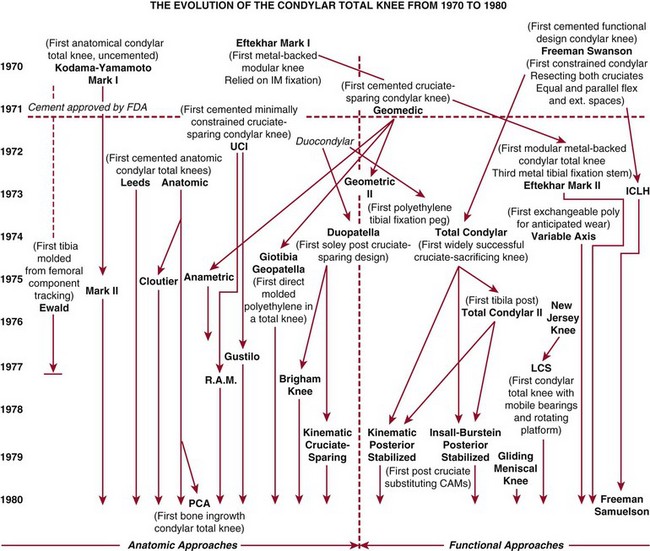
Figure 97-33 The evolution of the condylar total knee from 1970 to 1980.
(Adapted from Robinson RP: The early innovators of today’s resurfacing condylar knees. J Arthroplasty 20[Suppl 1]:2, 2005.)
These devices then evolved into the Zimmer NexGen LPS prosthesis. Subsequently, although the basic elements of the LPS prosthesis have endured, line extensions have occurred to attempt to address specific issues noted with the initial device. A high-flexion variant, the Zimmer NexGen LPS Flex-Fixed prosthesis, was introduced almost 10 years ago, with augmented posterior condyles to help decrease polyethylene contact pressures in higher flexion and a cam mechanism that was optimized for the high-flexion environment (Figs. 97-34 to 97-36; see Figs. 97-25, 97-26, and 97-28). More recently, a gender-optimized variant was added to the system (Zimmer Gender Solutions Nex Gen LPS High Flex knee), which has a narrower medial to lateral width, thinner anterior flange, and higher Q angle to the trochlear groove for a better match to the native female anatomy. In addition to the Nex Gen LPS prosthesis, the Press-Fit Condylar (PFC) PS and its successor, the PFC Sigma PS prosthesis (Fig. 97-37), were developed from the same TCP foundation, as were the Optetrak PS and Advance PS prostheses; the PCL-preserving Duopatellar prosthesis evolved into the Kinematic I and II and PFC CR prostheses (Fig. 97-38).245,321

Figure 97-35 The modular Insall-Burstein II Posterior-Stabilized prosthesis. A, Front view. B, Side view.
During the consolidation of the PFC CR and PS variants under the PFC Sigma brand more than a decade ago, the coronal plane geometry of the CR and PS implants was made identical.252 This highlights the trend that has occurred over the past 15 years where, to some degree, prosthesis design has converged with several seemingly important elements becoming common, not only to CR and PS variants in the same implant system from one manufacturer, but also across manufacturers. These desirable features of fixed-bearing, surface replacement prostheses include the following: multiple sizing options to match a broader range of native anatomy better; side-specific femoral components with anatomically oriented trochlear grooves designed to accommodate native and resurfaced patellae; front-loading, modular, metal-backed tibial components for ease of potential revision and optimization of soft tissue balancing; moderately conforming round-on-round femorotibial geometry in the coronal plane to minimize edge loading and polyethylene wear; and a femoral component with the so-called J curve, multiradius sagittal plane geometry that is moderately to highly conforming during the early arc of flexion to optimize contact areas, but where the radius of curvature decreases toward the posterior condyles, which facilitates rollback and range of motion.231 Examples of CR and PS knee prostheses that currently incorporate most or all of these concepts include the Zimmer Nex Gen, DePuy PFC Sigma, Smith & Nephew Genesis II, and Biomet Vanguard systems. Other systems, such as the Stryker Triathlon, Smith & Nephew Journey Bi-Cruciate Stabilized, and Wright Advance Medical Medial Pivot Knee, incorporate alternative unique elements that theoretically change the function of the devices. The features of this later group of devices that are considered guided motion prostheses are described here.
Guided Motion Prostheses
Although traditional PS knees may be considered guided motion prostheses to some degree, the kinematics of traditional surface replacement prostheses is less rigidly dictated by the design than in the prostheses introduced during the past 10 years which are usually considered to be guided motion devices. Each of these devices has similar elements that attempt to compel the components to move in a specific way. Two common features include a femoral component with a single sagittal axis of rotation to at least 90 to 100 degrees of flexion, rather than the J curve noted earlier, and articular surfaces that are molded and shaped to encourage rotation and rollback of the lateral condyle on the tibia while the medial femoral condyle remains relatively static. As noted in the previous section, most current traditional fixed-bearing surface replacement prostheses have a femoral component with posterior condylar geometry that incorporates a number of different axes of rotation. This effectively creates a decreasing sagittal radius of curvature of the posterior condyles, which facilitates rollback in flexion. However, although the J curve theoretically facilitates rollback and improves flexion, the decreasing radius of curvature reduces the contact area of the articulating surfaces as the knee flexes, which may lead to increased polyethylene stresses.231 In most surface replacement designs, the effects of this J curve do not occur during the initial 30 to 40 degrees of flexion; therefore, the increased joint forces generated during the weight-bearing portion of the gait cycle are accommodated by articular surfaces with moderate to high combined coronal and sagittal plane conformity, which helps reduce potential wear. In addition to this problem with potential wear, the decreasing radius of curvature results in decreasing tension on the collateral ligaments as the knee flexes. This reduction in soft tissue tension has been implicated in the phenomenon described as midflexion instability, in which some patients experience pain and instability with activities performed with the knee in moderate flexion, such as stair climbing or rising from a chair.304 This is a controversial subject; however, in a minority of modern fixed-bearing surface replacement prostheses, it has led to the incorporation of a fixed single sagittal radius of curvature through an extended arc of motion exceeding 90 to 100 degrees. The Stryker Triathlon prosthesis (Fig. 97-39), and the Scorpio knee that preceded it, along with the Wright Medical Technologies Advance Medial Pivot Knee, are designs that incorporate this concept of a single sagittal axis of rotation. However, at higher degrees of flexion, these devices actually incorporate a gradual reduction of the sagittal radius of curvature to allow better rollback. Other theoretical advantages of a prosthesis with a constant sagittal radius of curvature and a more posterior flexion-extension axis that lengthens the extensor moment arm are improved quadriceps function and reduced anterior knee pain.192
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree