Fig. 33.1
Plain radiograph. (a) AP view of the pelvis with both hips with neutral tilt and obliquity. On the right hip, the FAI is present. (b) The frog-leg lateral radiograph provides accurate visualization of the femoral head-neck offset
Except the false profile view, all the remaining aforementioned projections are performed in lying supine position. In the AP view of the hip and pelvis, the patient’s feet must be internally rotated 15° and the x-ray beam directed exactly in the AP plane [8]. The true AP pelvis view should have a neutral tilt and obliquity with the tip of coccyx 1.5–2 cm from symphysis. The AP pelvis film is centered low over the hips, and this is used rather than just an AP view of the affected hip for two reasons. First, it allows a radiographic examination of closely related areas, including the sacrum, sacroiliac joints, ischium, ilium, and pubis. Second, it allows us to compare subtle variations of the affected and contralateral hip.
The frog-leg lateral view is obtained with the hip abducted and the x-ray beam oriented in the AP direction [8]. The frog-leg lateral view provides a good lateral view of the femoral head and head-neck junction. The 45° and 90° Dunn views are taken with the hip flexed 45° or 90° and 20° abducted and the x-ray beam directed in the AP plane [7].
In recent years, much attention has been devoted to radiographic changes associated with FAI [7, 9]. The FAI syndrome could be divided into three types: pincer type, cam type, and mixed type (a combination of both). In the pincer type FAI, we could find excessive acetabular coverage, a crossover sign (COS) (Fig. 33.2), or posterior wall sign [9]. The crossover sign is associated with cranial acetabular retroversion but could also be often present on well-positioned AP pelvis radiographs in the absence of acetabular retroversion. Zaltz et al. reported that different morphologies and sizes of the anterior inferior iliac spine (AIIS) might contribute to the COS even in the absence of acetabular retroversion [10]. Findings supportive of the cam-type FAI include an aspherical femoral head with an abnormally increased alpha angle, focal prominence at the anterior or lateral femoral head-neck junction (Fig. 33.3), and a typical pistol grip deformity of the proximal femur or cystic lesion [7, 9]. The alpha angle is defined as the angle subtended between the midline of the femoral neck and a line connecting the center of the femoral head to the point along the head-neck junction which first deviates from the sphericity of the femoral head (Fig. 33.3b). Notzli et al. reported significant increases in the alpha angle in FAI patients (72°) when compared with healthy controls (42°) [11].

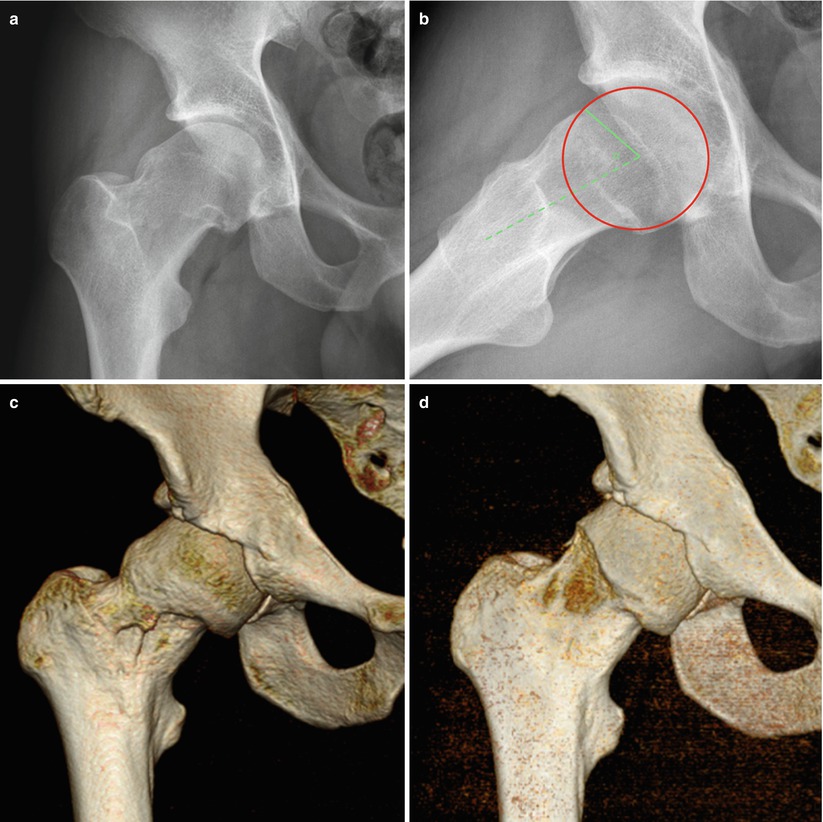

Fig. 33.2
The crossover sign in patient with Pincer type of FAI syndrome. Blue line indicates anterior wall and red line posterior wall of the acetabulum
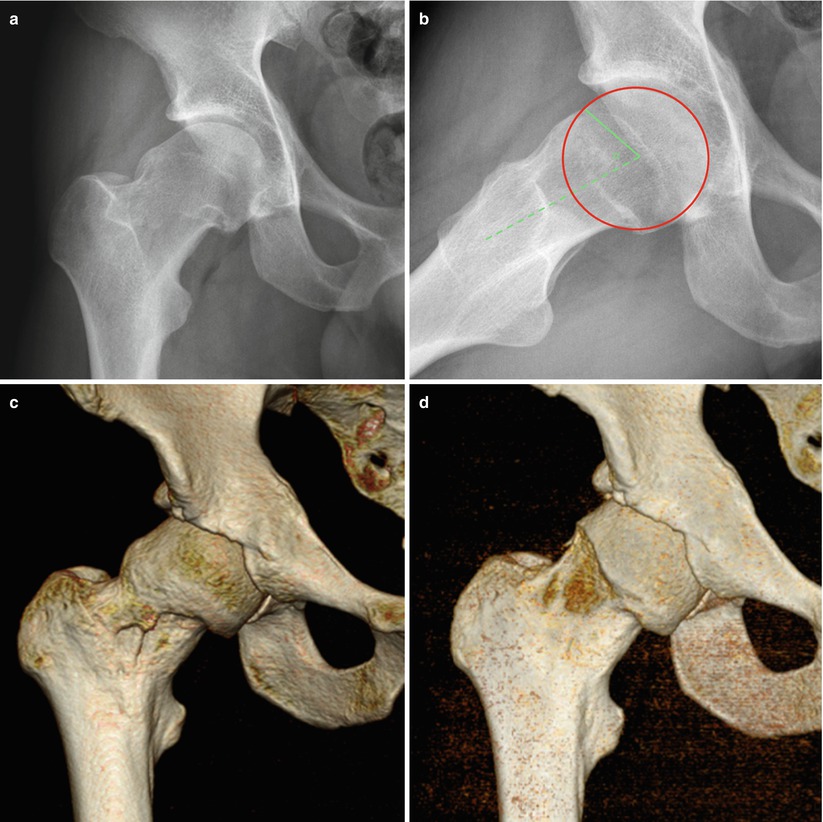
Fig. 33.3
A 28-year-old soccer player with painful right hip (a) AP view with pistol grip deformity on the lateral part of the head-neck junction typical for cam type of FAI syndrome. (b) The frog-leg view reveals anterior part of cam lesion. Measurement of the alpha angle is shown. (c) Anterior view of the right hip on 3D CT before and (d) after arthroscopic cam resection
Considerable variability in measurements could arise depending on pelvic position [7]. Plain radiographic findings in young patients with painful hips suggestive of any type of FAI should always be correlated with clinical evaluation.
33.2 Computed Tomography
CT is used to further characterize a bony detail of the hip not available on plain radiographs by providing cross-sectional information. CT of the hip should be done primarily in the setting of trauma or in suspicion to the neoplasm of the proximal femur or acetabulum. Occasionally, it is used to evaluate developmental hip dysplasia, to detect the small particle disease, and to evaluate for nonunion [12]. Multislice helical CT has markedly improved our ability to rapidly acquire high-resolution images with multiplanar 2D or 3D reconstruction with the benefits of a lower radiation dose than conventional CT, to improve resolution and to help us reduce the exam time. 3D CT reconstruction shows us a three-dimensional view of the acetabulum and femoral head and neck in FAI syndromes. The 3D CT helps us to clarify where exactly the cam or pincer lesion or other different abnormalities are situated, and therefore, it is very helpful in preoperative planning (Figs. 33.3, 33.4, and 33.5). In our institution, 3D CT is performed in every patient before and also after arthroscopic management of the FAI syndrome to clarify whether the resection of the cam or pincer lesion has been sufficient.
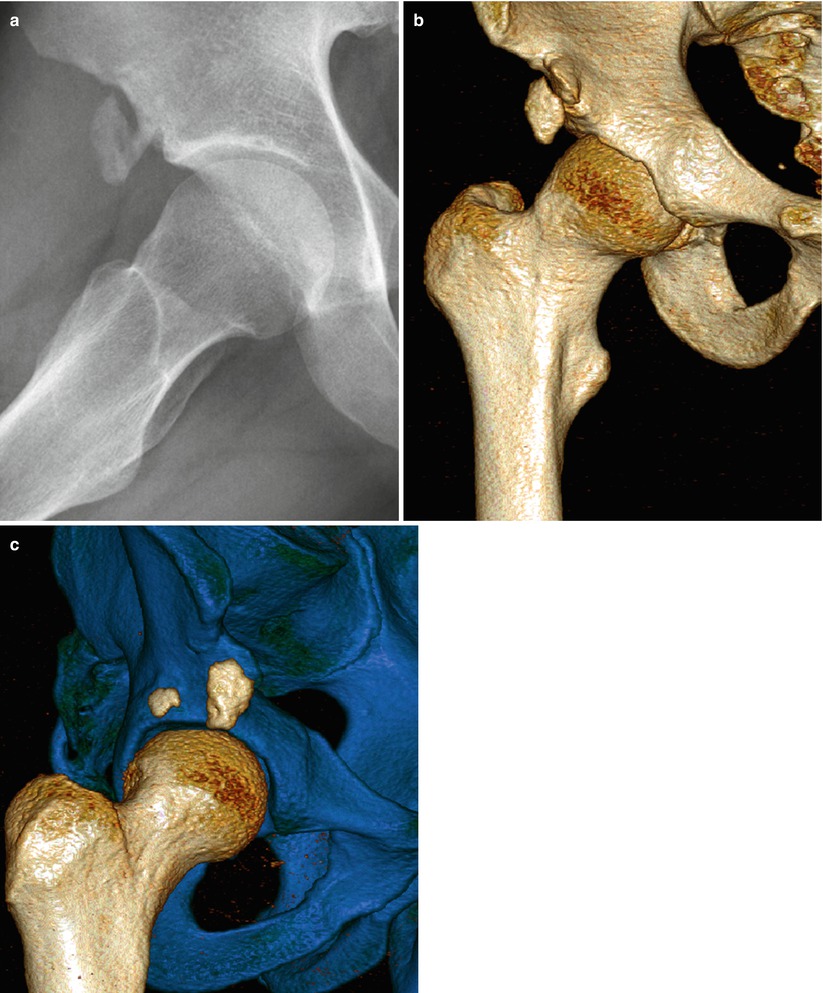
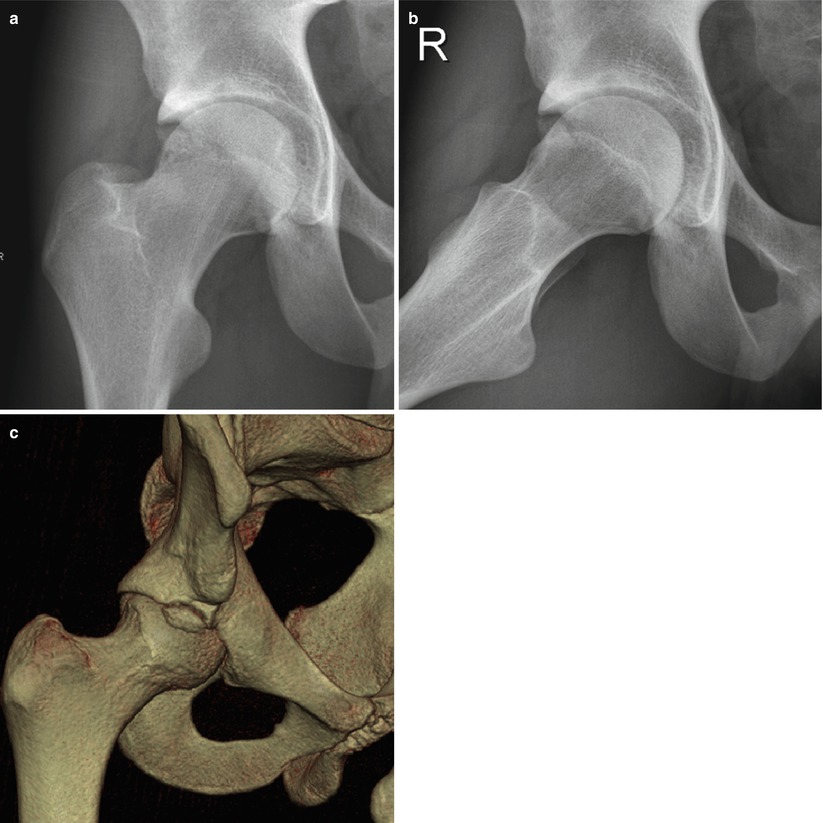
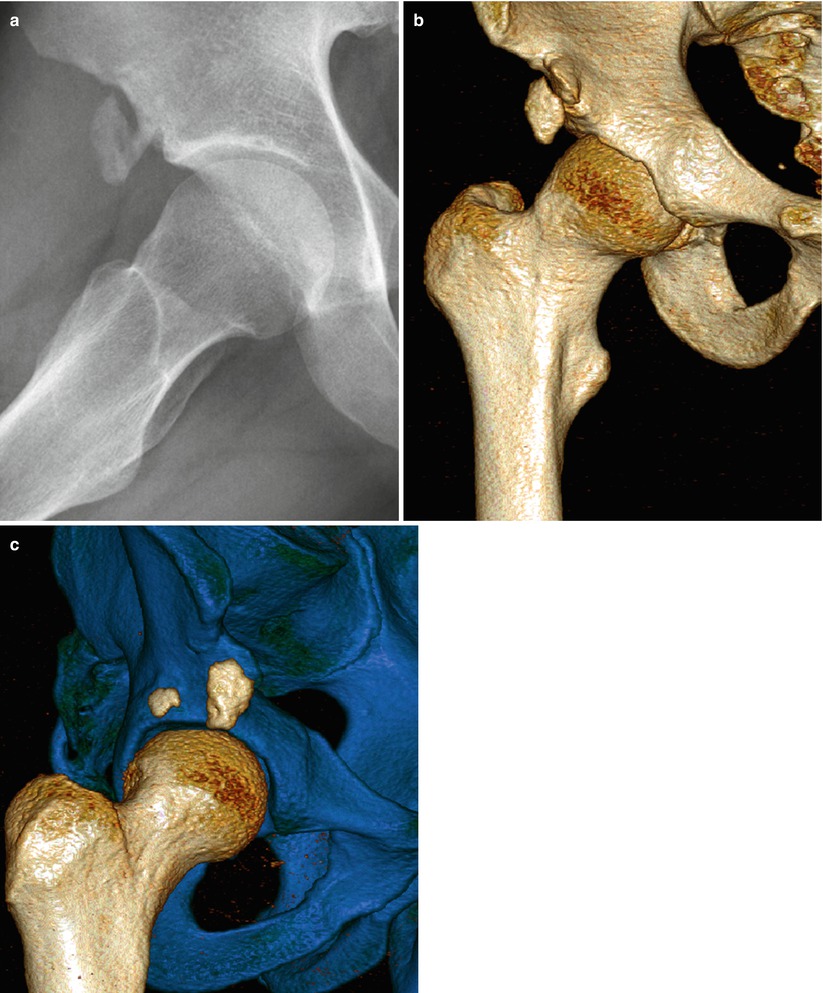
Fig. 33.4
A 24-year-old ice hockey player who suffered an avulsion fracture of the anterior inferior iliac spine 8 years ago. Subspine impingement syndrome is seen on the (a) frog-leg lateral view and (b) anterior and (c) anterolateral view of 3D CT
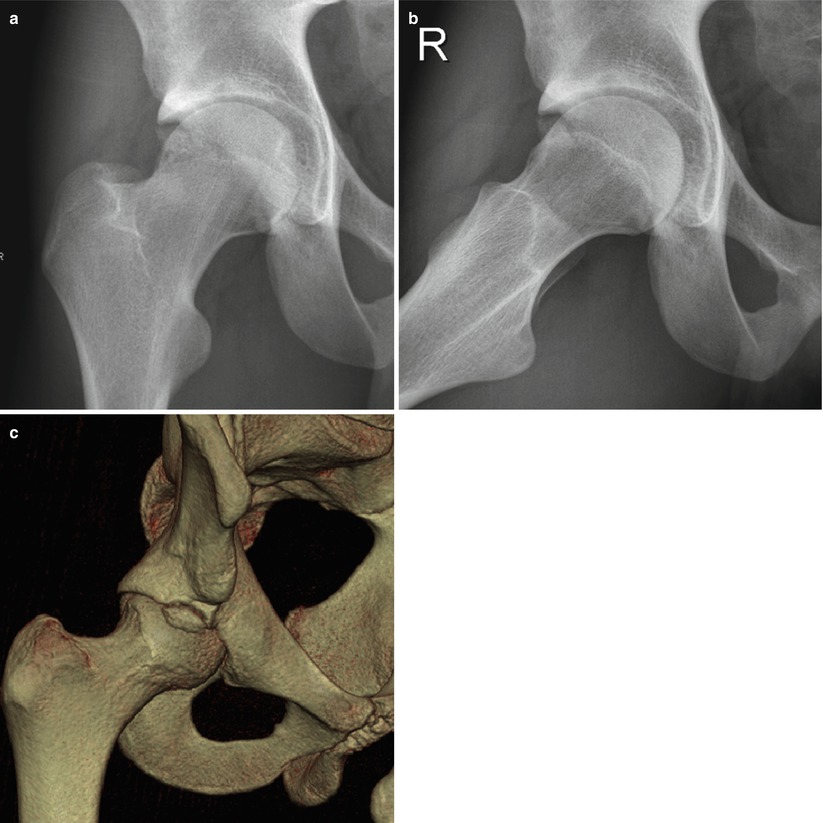
Fig. 33.5
A 34-year-old athlete with painful hip. (a) AP and (b) frog-leg lateral view with presence of os acetabuli and signs of mixed type of FAI syndrome. (c) An anterolateral view of 3D CT highlights os acetabuli and FAI syndrome better
In the setting of trauma, CT of the hip is used primarily to better characterize a fracture or fracture dislocation and to aid in the detection of articular surface fractures and intra-articular loose fragments [1]. CT can also yield information used in predicting hip instability in fractures of the posterior wall of the acetabulum.
CT offers a tool for preoperative measurement and planning for patients undergoing hip arthroplasty and can also be helpful in detecting and determining the extent of osteolysis around the hip prosthesis [13]. But in this case, a high artifact-free protocol is necessary.
CT can be used to help characterize the nature of the tumor matrix and demonstrate cortical thinning or destruction, in cases of neoplasm [14].
33.3 CT Arthrography
CT arthrography of the hip is an excellent alternative to MR arthrography in patients with presence of loose metallic implants, presence of cardiostimulator, or with any other contraindications to MRI. CT arthrography can elucidate intra-articular abnormalities due to leakage of contrast into sites of labral, chondral, or ligamentous injury and can demonstrate loose bodies. Intra-articular injection before CT arthrography is preferably carried out using a combination of iodinated contrast with bupivacaine. In case of pain relief after local anesthetic application, it can help us to distinguish intra-articular from extra-articular sources of the hip pain [14].
33.4 Ultrasound
Ultrasound is a complementary diagnostics method to MRI in the evaluation of hip pain. Ultrasound is suitable especially for the evaluation of snapping hip syndrome and image-guided intervention [15, 16]. This method has many advantages over other imaging methods: It is noninvasive; it lacks ionizing radiation, allows concomitant evaluation of the contralateral hip, allows dynamic examination of the tendons and muscles, and can recognize pathologies of the tendons and soft tissue; and it is an inexpensive and quickly performed method and can be used as a guide for therapeutic injections and aspirations [17]. Ultrasound may provide a useful tool for early diagnosis of the cam-type FAI in daily practice [18].
Ultrasound is an excellent noninvasive tool for the diagnosis of different types of snapping hip syndrome in patients in case the snapping phenomenon may occur during a movement of the hip in the course of the examination [15].
Despite these advantages, ultrasound does not provide anatomic overview and demonstration of the bony structure, articular surfaces, bone marrow, and surrounding soft tissues in comparison with MRI [19].
Ultrasound is well suited for image-guided interventional procedures including injection of the joint, tendon sheaths, or bursa; drainage of para-articular fluid collections; and treatment of calcific tendinosis [17]. Continuous imaging during aspiration or injection helps us to verify a proper positioning of the needle tip. The problem is the impossibility to reevaluate the images of the hip later, and a very experience ultrasonographist must be present.
33.5 Conventional Magnetic Resonance Imaging
MRI is a secondary diagnostic method of choice in the evaluation of adult painful hip which provides excellent information about soft tissue and bone marrow abnormalities which are not seen on plain radiograph, CT, ultrasonography, or nuclear medicine exams. MRI is effective in demonstrating intra-articular and extra-articular pathology. Intra-articular disorders that are well demonstrated with MRI include osteonecrosis, stress fracture, occult fractures, joint effusions, osteoarthritis, and inflammatory arthropathies [20–23]. Different extra-articular pathologies such as pubic osteitis, sacroiliitis, bursitis, myotendinitis, and occult pelvis neoplasm may also be well recognized on MRI. In recent years, poor success has been demonstrated in the detection of labral tears and cartilage lesion on conventional MRI at 1,5 T, but this may improve with 3T MRI and with newer imaging techniques [3, 24]. Future improvements in MRI technology may lead to successful noninvasive evaluation of these structures. Studies in recent years have shown that 3T MR arthrography is much more beneficial in the detection of labral tears in comparison with conventional 3T MRI [6, 25]. Although MR arthrography is an excellent positive predictor in diagnosing acetabular labral tears and cartilage abnormalities, it still has limited sensitivity. A negative imaging study does not exclude the presence of intra-articular pathology that can be identified and treated arthroscopically [26].
Protocols for MRI of the hip vary among institutions and with the type of scanner used. The quality of the examination depends on the field strength of scanner, coil selection, technical parameters used, and whether or not dedicated small-field-of-view images of the hip are acquired. MRI protocols are adapted to the clinical presentation. For instance, at our institution, the typical exam for an adult with unexplained hip pain includes seven sequences and is tailored toward evaluating intra-articular and extra-articular pathology. The coronal T1-weighted images of both hips reveal anatomy and marrow-based pathologies such as occult fractures, tumors, or osteonecrosis. The T2-weighted fat-suppressed images of both hips demonstrate myotendinous injuries, intra-articular or extra-articular fluid collection such as bursitis and joint effusions, depict stress fracture and occult fracture, subchondral cyst, osteonecrosis, and tumor as marrow-based changes. For the detection of cartilaginous and labral lesions, it is essential to create small-field-of-view high-resolution imaging of the affected hip [12]. The oblique sagittal SPGR sequences are used to measure for the cam and pincer FAI and to assess for the characteristic osseous bump present with the cam FAI.
33.6 Magnetic Resonance Arthrography
Magnetic resonance arthrography (MRA) of the hip is a diagnostic method of choice of unexplained adult hip pain in the event that we suspect intra-articular pathologies. Several reports have documented the success of MRA of the hip in detecting cartilage and labral injuries [3, 5, 14, 27, 28]. MRA can also depict abnormalities of ligamentum teres and joint capsule and demonstrate the presence of loose bodies or proliferative changes of synovitis. In comparison with conventional MR, MR arthrography allows better visualization of intra-articular anatomy because the intra-articular application of the fluid displaces the joint capsule from the underlying bone and normal structures. Leakage of contrast into the labrum or cartilage is direct evidence of pathology of these structures [24]. MRA of the hip is thus helpful when conventional MR is noncontributory and when there is clinical suspicion of labral or other intra-articular pathologies.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree






