Acute
Surface
Extension
Treatment
Type I
Damaged
<1 cm2
Debridement
Type II
Damaged
>1 cm2
Fixation
Chronic
Surface
Extension
Treatment
Type 0
Intact
Any
Retrograde Drilling
Type I
Damaged
<1.5 cm2
Microfractures
Type II
Damaged
>1.5 cm2
Cartilage Replacement
Type IIA
Damaged
>1.5 cm2 >5 mm
CR+Bone Graft
Type III
Damaged
Anatomy disruption
Massive Graft
Routine X-ray is the first-line diagnostic tool also in order to rule out a fracture in acute cases [13]. Nevertheless, apart large lesions, OCL can easily be undiagnosed [14].
CT is valuable for the detection of subchondral bone injuries: it may clearly detect the size, shape, and extent of the localization (Fig. 52.1) [15].


Fig. 52.1
Coronal view of a CT scan performed for OCL preoperative evaluation. CT scan is very useful to improve subchondral bone visualization
MRI is the gold standard for OCL diagnosis, providing information about bone bruise, cartilage status, and soft tissues [15]. The sensitivity of MRI is high when correlated to arthroscopic findings (81–83 % or even higher) [16]. The most frequent features compatible with OCL are decreased signal intensity on T1-weighted images and increased intensity on T2-weighted images. In case of incomplete separation of the fragment, T2-weighted images may be confusing due to a high signal, with lower percentage of correlation with arthroscopic findings (55.6 %). In this case, the cartilage break discriminates (Fig. 52.2) [16].
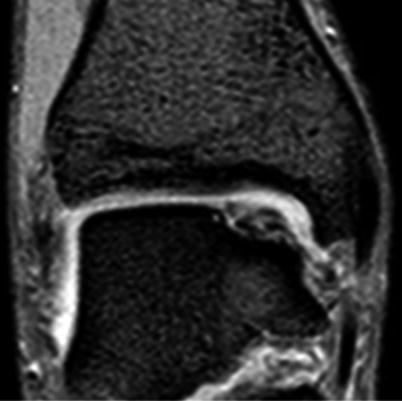
Fig. 52.2
Coronal view of MRI scan performed for chronic medial OCL. MRI is the best diagnostic tool, as it can visualize the cartilage and the subchondral bone as well as other soft tissue as ligaments
52.3 Treatment Strategy
No widely shared guidelines exist for OCL treatment [14, 17, 18]. A valid classification, focused on arthroscopic/MRI findings and corresponding treatments, considering the area and the depth of the lesions as well, was made by Giannini [19].
52.3.1 Acute Lesions
Conservative treatment is not successful in acute lesions, requiring arthroscopic procedures. Debridement and fragment excision are advised in case of acute lesions with fragment’s dimensions inferior to 1 cm [19, 20]. Fragment fixation is performed in case of larger OCL using bioresorbable screws: good long-term results are achieved thanks to an effective vascular restoration [21]. Excision for larger fragment can dramatically raise osteoarthritis rates at long-term follow-up [20]. Recently osteochondral autografts have been adopted, with good results even in acute lesions [21].
52.3.2 Chronic Lesions
52.3.2.1 Conservative Treatment
The aim of conservative treatment is unloading the osteochondral layer, preventing the necrosis, and resolving the bone edema. To date, it should be reserved to small lesions with no fragment isolation in almost-asymptomatic patients [14, 17, 22]. In these cases, 45 % of the patients may benefit from a conservative approach. A possible beneficial approach in athletes may consist in rest, with sport activity restriction, and even a limited period of non-weight-bearing, lasting only a few weeks, according to the gravity of the lesion. In a work by Mei-Dan, hyaluronate and platelet-rich plasma (PRP) were injected intra-articularly in OCL, improving the clinical outcomes, with long-lasting results for PRP (at least 6 months) [23]. Intra-articular injections may be functional in athletes to delay the surgical treatment even in symptomatic lesions with no fragment isolation.
52.3.2.2 Retrograde Drilling
Retrograde drilling is mostly effective in lesions 0 according to Giannini’s classification, with modest subchondral bone involvement and chondral layer continuity and viability [19]. The rationale consists in a stimulation of the repair depending on subchondral bone marrow cells [19, 24, 25]. The approach is made through sinus tarsi, drilling the subchondral bone without damaging the articular surfaces. An autologous calcaneal bone graft is then performed. Retrograde drilling may avoid the necrotic effect of the anterograde approach, preserving the chondral tissue [25]. Good results were reached in case of viable cartilage; nevertheless, it has been applied even in revision surgery [25].
52.3.2.3 Microfractures
Widely diffused microfractures are effective in OCL inferior to 1.5 cm2 [6, 7, 19, 26]. The technique can be easily performed arthroscopically, penetrating the subchondral bone every 3–4 mm, using an awl [26]. Thanks to bone marrow stimulation, this procedure allows a good and rapid restoration of the osteochondral layer, but it generates fibrocartilage, with lower biomechanical properties and durability [14, 24]. Good clinical outcomes were reported by many authors, but medial lesions and larger and deep OCL tended to worsen over the time [26, 27].
52.3.2.4 Mosaicplasty
Osteochondral plugs, obtained from non-weight-bearing areas of the knee and, possibly, ankle, are implanted to restore the proper osteochondral layer [22, 24, 28]. This procedure often requires a malleolar osteotomy to improve the exposure. In the report by Hangody [22], the best OCL to treat is defined as approximately 10 mm large, positioned on the medial or lateral dome (not the central part of the talus), in a non-arthritic ankle. Clinical and bioptic results were promising, achieving remarkable outcomes even in athletes (63 % of the patients came back to sport activity at the same level, only 9 % gave up sport), with a slight deterioration over time, at around 10 years from the surgical procedure [28]. Nevertheless, mosaicplasty faces some drawbacks. First, it is a technical demanding technique, which includes a donor-site morbidity. Between osteochondral plugs, fibrocartilage is frequently found; moreover, not all lesions are successfully treated due to challenging locations (Fig. 52.3) [22, 24, 28].
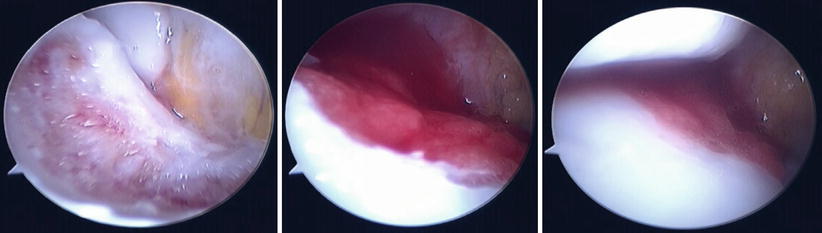
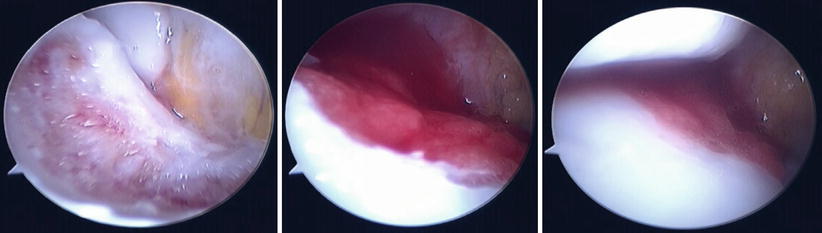
Fig. 52.3
Intraoperative arthroscopic images during BMDCT. This procedure can be performed using an arthroscopic one-step technique. First, the lesion is debrided, reaching a healthy subchondral bone. Then the biomaterial, a collagen membrane loaded with autologous mesenchymal stem cells, is implanted. Then a layer of PRF is sprayed on the biomaterial, to improve the stability of the implant and the cell differentiation and growth
52.3.2.5 Autologous Chondrocyte Implantation
Autologous chondrocyte implantation (ACI) has been intensively applied for OCL of the ankle, with successful clinical outcomes (90 %) [18]. Although no clear superiority has been established, ACI is considered the gold standard in regenerative procedures [18, 19]. The first-generation procedure was technically demanding, requiring an open-field approach, a malleolar osteotomy, and a periosteal flap suture [18, 29]. The second-generation procedure was performed arthroscopically, thanks to the development of specific instrumentation and scaffold [29]. Arthroscopic technique is performed with a two-step approach, with a first arthroscopy to debride the lesion and harvest the autologous chondrocytes doomed to expansion. A source of viable chondrocytes is the osteochondral fragment, the area around the OCL, or even a non-weight-bearing area of the knee [29, 30]. After the first arthroscopy, the chondrocytes are expanded in culture and seeded on a hyaluronate membrane. After 3 weeks, the second step takes place, and the biomaterial is arthroscopically implanted onto the lesion. The hyaline regeneration was confirmed by histological and radiological outcomes [29, 30].
52.3.2.6 Bone Marrow-Derived Cell Transplantation
Bone marrow-derived cell transplantation (BMDCT) is a regenerative technique for bony and chondral layer, based on mesenchymal stem cells [19, 24, 31]. This technique may be performed in one step, in a same surgical session, or with more steps, with cells culture and enrichment: good results were achieved also in degenerated joints [19, 24, 31]. In the one-step technique, the cells are harvested from the iliac crest using a bone marrow needle. During the concentration, a standard arthroscopy of the ankle is performed; the joint and the defect is debrided. The cell concentrate is loaded on a collagen (or hyaluronate) membrane and then implanted in the joint using a specific instrumentation [31]. Then, a layer of platelet-rich fibrin (PRF) is sprayed on the biomaterial, to improve growth and differentiation and stability of the implant. Clinical results at medium-term follow-up are encouraging, with excellent outcomes even in athletes. Hyaline cartilage regeneration has been appreciated in bioptic samples and MRI qualitative scans [19, 31].
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree






