Sports practice
Incidence
Most common mechanism of injury
Rugby [5]
28 % of all knee injuries
38 % tackle
3.1 per 1,000 h of play
25 % ruck and maul
American football [6]
36.1 % of all knee injuries
Mostly traumatic
2.42 per 1,000 h of play
0.13 per 1,000 h of training
77 % collision with another player
1.47 per 1,000 h of match
Alpine skiing [9]
18 % of all injuries
Noncontact (valgus-external rotation)
60 % of knee injuries
Football [10]
Mean 0.33 per 1,000 h
70 % contact with an opponent
1.31 per 1,000 h of match
40.1.3 Clinical and Diagnostic Examination
First of all, it is mandatory to ask the patient or somebody who was present at the moment of the injury about its mechanism: an isolated MCL injury generally occurs with a valgus force applied to a flexed knee; if any rotational mechanism is present, one must suspect a multiple ligament injury, such as the frequent association of an ACL lesion. A careful inspection of the knee must be done looking for bruising, hemarthrosis, and localized swelling which are frequent in isolated MCL injuries. On the contrary, an early onset hemarthrosis must bring the suspect on an intra-articular pathology such as tibial plateau fracture or ACL/PCL lesion. Patients presenting an MCL injury normally refer pain to a well-defined area corresponding to the site of lesion, which should be identified through careful palpation. Assessing the medial joint line opening will help to grade the MCL lesion [11]: the valgus stress test must be applied at 0 and 30° of flexion and compared to the healthy knee. An opening between 0 and 5 mm defines a grade I lesion, between 5 and 10 mm a grade 2 lesion, and if the joint line opening is more than 10 mm, the lesion is graded 3. A positive valgus stress in extension is indicative of a posterior oblique ligament (POL) or posteromedial corner (PMC) lesion, and it’s most commonly found in multiligamentous injuries, especially with involvement of the ACL [12]. Assessment of the combined rotational and central pivot instability can be very difficult in an acute setting and can possibly require examination under anesthesia to address diagnosis and give indications for successive treatments. Presence of an eventual ACL- and PCL-associated lesions has to be investigated carefully as they are very frequent. Assessment of the associated rotational component of the lesion can be obtained through different tests:
1.
Anterior drawer in external rotation: the anterior drawer test is performed in a standard fashion at 90° of flexion and with the medial tibia held in external rotation [13].
2.
Swain test: with the knee at 90° lying out of the bed, the tibia is forced in external rotation causing pain along the medial side of the joint [14].
3.
Combined valgus stress test: the valgus test is performed at 30° of flexion with the foot held in external rotation.
In acute settings, a standard radiographic exam must be performed looking for potential fractures or epiphyseal cartilage damage and must include anterior-posterior, lateral, and patellar axial views. In chronic lesions, the exam must be completed with a full set of weight-bearing x-rays, including long-leg and Rosenberg-Schuss views in order to evaluate frequent concomitant osteoarthritic degeneration of the medial compartment and the presence of a calcification near to the femoral insertion, known as Pellegrini-Stieda lesion [15]. In the case of chronic laxity, many authors advocate the use of dynamic valgus stress x-rays in order to evaluate and measure differential laxity and plan the most appropriate treatment [16].
MRI is fundamental in the diagnosis of medial side injuries as it allows to evaluate not only ligament but also articular cartilage and meniscal lesions. In acute settings, a bone bruise of the medial compartment subchondral bone following a valgus-directed force can be frequently found. MRI grading of the lesion has a very good concordance with clinical grading and can be used as a complementary tool for addressing diagnosis and therapeutic indications [17].
40.1.4 Treatment Strategy
40.1.4.1 Conservative Treatment
The wide area of the lesion’s surface and the relatively high blood supply of the MCL explain the very high rate of spontaneous healing without need of surgical reparation or reconstruction. In the case of a stage I to II lesion of the MCL, primary treatment must be conservative according to the principles shown in Table 40.2. The insulted knee must be immobilized in a brace to protect it from iterative injuries and decrease pain. Early passive motion and partial weight bearing should be allowed as soon as possible. Strengthening of the quadriceps and flexor muscles with isometric exercises must start as soon as possible in order to be able to proceed to a fast rehabilitation program.
Table 40.2
Conservative treatment of isolated MCL injuries
Grade | Immobilization | Weight bearing | Restriction of ROM | Return to training |
|---|---|---|---|---|
I | Only for pain prevention | Partial | Full-active ROM as soon as possible | 10–15 days |
II | Hinged short-arm knee brace | Partial | Full-active ROM as soon as possible | 4 weeks |
IIIa | Hinged long-arm then short-arm knee brace | Partial as soon as possible | Immobilization 30° for 3 weeks (with passive ROM recovery) then recovery of full ROM after 3 weeks | 8 weeks |
Return to play will be possible only at the resolution of pain and after having achieved a sufficient stability at the clinical exam. As shown by Indelicato [18] and Jones et al. [19], results of a well-conducted conservative treatment are positive in 90–95 % in a population of competitive athletes, also in the presence of a grade III lesion. There is no consensus about the effectiveness of using a protective brace during activity after a minor lesion of the medial compartment, the prescription must therefore be done only if clinically necessary and in selected cases such as contact sports or persistent subjective instability feeling [20]. A minor group of conservatively treated proximal s-MCL lesions can develop a localized pain at the femoral insertion scar which can require a delayed surgical treatment (debridement, scarring of the ligament, and microperforation of the insertion) with satisfactory results.
40.1.4.2 Surgical Treatment
Surgical reparation in athletes can find an indication in the presence of a bony avulsion, in multiligamentous injuries, and in the presence of an isolated complete tear involving both midsubstance and tibial insertion. A diagnostic arthroscopy should be routinely performed in order to check for eventual associated lesions of menisci, cruciate ligaments, and articular cartilage. A bony avulsion, more frequent at the femoral site of insertion (Stieda fracture), is normally reinserted using a metallic lag screw. In the presence of distal or proximal avulsion, reparation should be completed with use of suture anchors (Fig. 40.1) in order to obtain a stable and anatomic reinsertion. The distally avulsed MCL can lie on the medial side with the pes anserinus tendons interposed, defining a “Stener-like” lesion of the knee [14]. This specific lesion cannot repair without surgical intervention and has to be immediately recognized and addressed. A midsubstance lesion can be treated with a standard side-to-side reparation technique, but as the quality of the remnant tissue is frequently poor, often the association with an augmentation technique as the ones published by Kim et al. [21] and Stannard [22] is needed also in acute settings. In conclusion, a stepwise approach must be employed in the presence of an acute complete lesion of the MCL/PMC:
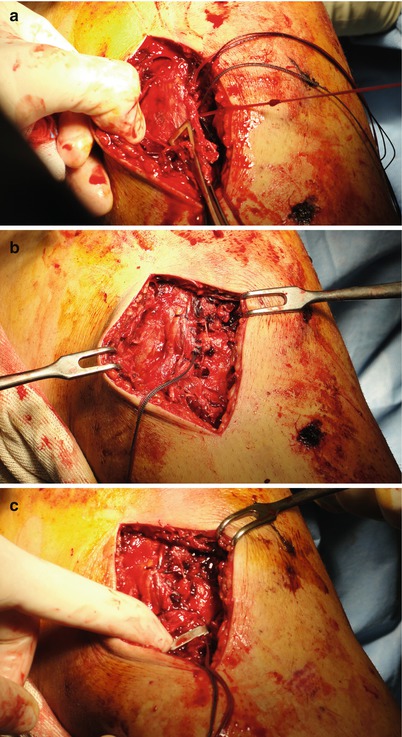
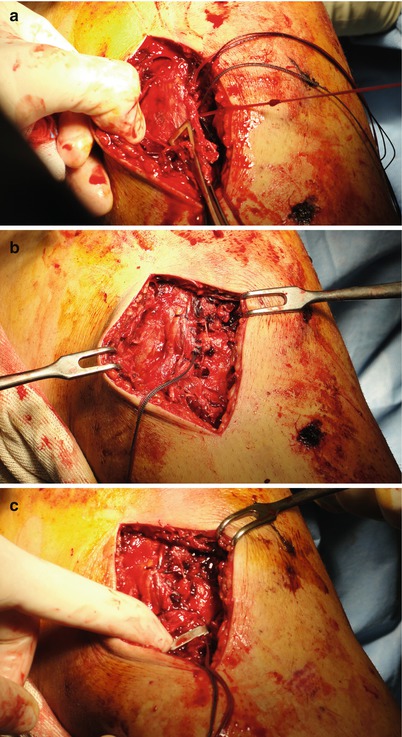
Fig. 40.1
Complete midsubstance and distal insertion lesion of the s-MCL: anatomic reinsertion is obtained using suture anchors (a), side-to-side Orthocord ® sutures (b) and completed positioning of a metallic staple on the proximal tibia (c)
Begin with the deep layer and reconstruct meniscotibial and meniscofemoral bundles of the deep MCL, stabilizing the medial meniscus.
Progress and repair the eventually affected POL and the portion of the superficial MCL (s-MCL) interested by the lesion, taking care of providing a strong but anatomically correct reinsertion using suture anchors. In the presence of a midsubstance lesion, proceed to side-to-side reparation if the remnants are strong enough or switch to repair-augmentation or reconstruction if a correct stability all throughout the range of motion cannot be achieved.
In the presence of a nonreparable midsubstance lesion, we prefer not to use autologous semitendinosus as a graft, as it weakens medial side residual stability, and we rely on an allogenic tubular graft or, in selected cases, biosynthetic graft.
Tibial/femoral avulsions recognize a better prognosis if compared to midsubstance lesions, and best results are achieved if the reparation is performed within 3 weeks from the moment of injury [14]. There is a lack of evidence about clinical outcomes of surgically treated acute isolated MCL lesions. Most of our knowledge is based on multiligamentous injuries series including medial compartment reparation. Ibrahim et al. [23] reported about 18 patients undergoing a reparation of a complete acute MCL rupture: 89 % of patients were stable at a minimum follow-up of 39 months with a mean Lysholm score of 79.2, but mean Tegner score decreased to 4.7 from a pre-injury score of 7.6. Owens et al. [24] also reported good results on 11 complete MCL rupture at 48 months but with a relatively high ratio (27 %) of postoperative stiffness requiring secondary surgery (arthroscopic lysis).
40.1.4.3 Treatment of Chronic Lesions
Medial instability in the presence of an isolated chronic medial collateral ligament injury in competitive athletes is a very rare condition, but its association to ACL or ACL/PCL chronic lesions is far more common. In the case of a clinically relevant chronic medial instability, the surgical indication is mandatory. The results of reparative techniques are very poor, due to the chronicity of the lesion and the absence of healthy ligament tissue, necessary for achieving a good quality reparation, and this should not be performed in a chronic setting. Reconstructive surgery is commonly performed in these cases using different techniques and different grafts (autologous, heterologous, or synthetic). Most of the employable surgical interventions originate from the technique described by Bosworth in 1952 [25]. The semitendinosus tendon is stripped with an open stripper and left attached to its tibial insertion. The free end of the tendon is then whipstitched, and isometry is checked looping it on a K-wire positioned in the site of insertion of MCL on medial epicondyle. If isometry is confirmed, a half tunnel is performed, and the free part of the tendon is secured to the femur with a screw, having care of applying a varus moment to the tibia during fixation. If the semitendinosus tendon is not available as a graft (for instance associated ACL reconstruction), one can consider to use, with the same principles, a heterologous tubular graft (semitendinosus, peroneus longus, tibialis anterior or posterior). This technique has been heavily modified in the past few years, but it is still very useful in reconstruction of isolated chronic s-MCL lesion or as an augmentation in acute settings.
In the presence of a concomitant POL-PMC lesion/insufficiency, an anteromedial rotatory instability is defined, and the technique employed must include a stabilization of the PMC as an isolated reconstruction of the MCL could not be sufficient [21, 22, 26]. A fan-shaped graft as a heterologous fascia lata can be used in order to address also posteromedial component of the instability (Fig. 40.2): maintaining a single insertion on the femoral side (half tunnel and interference screw), the anterior part of the graft is inserted on the anteromedial side of the tibia using suture anchors and fixed a 30° of flexion. The rotational stability is then achieved fixing the posterior border of the graft on the posteromedial side of the tibia in full extension. In alternative, a number of techniques defined as “anatomic” have been described as the one described by Coobs et al. in 2010 [27]: two separate soft tissue grafts are used to reconstruct separately s-MCL and POL. All the grafts are secured on both sides with interference screws: first, the femoral insertions are fixed, then the distal part of the s-MCL is fixed at 30° of flexion and neutral rotation. The procedure ends with fixation of POL bundle in extension reproducing the “normal anatomy” of the medial side of the knee. This type of technique, although very promising on a biomechanical point of view, can be very complicated on the daily basis, as the increased number of tunnels and fixation devices can represent an issue, moreover, in the case of a surgically treated multiligamentous injury. Given this considerations, LaPrade and Wijdicks [28] have published very good results with this technique on 28 patients at a mean follow-up of 1.5 years: mean IKDC score improved from 43.5 to 76.2, and all patients noted a subjective improvement in terms of stability.








