Hip Dysplasia Overview
Michael Leunig
Reinhold Ganz
Hip dysplasia is a multifaceted orthopedic problem, which has been elaborated in the past periodically in several monographs, each time reflecting the contemporary evolution in understanding and treatment concepts. This chapter concentrates on current scientific knowledge and therapeutic practice.
Definitions
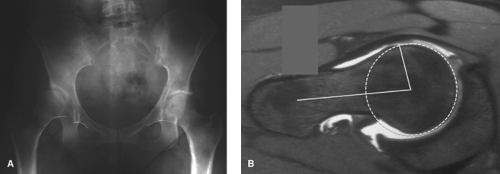
The hypernym “hip dysplasia” comprises the pathomorphologic spectrum of developmental dysplasia subsequent to global or local growth retardation, mainly the acetabulum. Retardation can be severe enough that a prenatal or true congenital dislocation of the femoral head can occur; dislocation can take place after birth when the immaturity of the acetabular development is not immediately recognized and properly treated. Complete dislocation can be high or low in the later process with or without articulating contact against the iliac bone (Fig. 18.1); a low dislocation may become difficult to distinguish from subluxation out of a shallow primary acetabulum (Fig. 18.2). Teratologic dysplasia is rare and frequently combined with other deformities such as sacral agenesis (Fig. 18.3). Growth retardation may persist over time with slight extent or treatment may
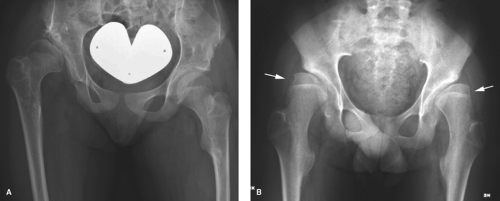
not resolve all adverse forces with the result that at the end of acetabular growth the femoral head remains within the acetabulum but coverage of the head is insufficient. In current practice this morphologic situation is labeled residual acetabular dysplasia (Fig. 18.4A) although the proximal femur frequently shows some minor deformity (Fig. 18.4B). Acetabular dysplasia is called secondary as consequence of a growth disturbance of the femoral head after some diseases during infancy, such as Perthes disease (Fig. 18.5) or from other vascular breakdown, after bacterial infection and occasionally after trauma (Fig. 18.6). Secondary dysplasia is also seen in neurologic disorders, where muscle imbalance, mainly between gluteus medius and iliopsoas muscles, is the primary force; the resulting deformity may vary from insufficient coverage of the femoral head to full dislocation (Fig. 18.7).
not resolve all adverse forces with the result that at the end of acetabular growth the femoral head remains within the acetabulum but coverage of the head is insufficient. In current practice this morphologic situation is labeled residual acetabular dysplasia (Fig. 18.4A) although the proximal femur frequently shows some minor deformity (Fig. 18.4B). Acetabular dysplasia is called secondary as consequence of a growth disturbance of the femoral head after some diseases during infancy, such as Perthes disease (Fig. 18.5) or from other vascular breakdown, after bacterial infection and occasionally after trauma (Fig. 18.6). Secondary dysplasia is also seen in neurologic disorders, where muscle imbalance, mainly between gluteus medius and iliopsoas muscles, is the primary force; the resulting deformity may vary from insufficient coverage of the femoral head to full dislocation (Fig. 18.7).
 Figure 18.1. Unilateral high dislocation in an 18-year-old female. Substantial hypoplasty of the entire femur. |
 Figure 18.2. Complete but low dislocation of the left hip and high subluxation from a shallow acetabulum on the right side in a 23-year-old female. |
 Figure 18.3. Teratologic dislocation of the left hip combined with ipsilateral sacroiliac instability due to agenesis of the sacral ala in a 7-year-old girl. |
 Figure 18.5. Bilateral Perthes deformity in a 15-year-old female. Adaptation during further growth resulted in a rather mild acetabular dysplasia with frequently seen retroversion. |
The term subluxation is used when the femoral has left the center of rotation of the socket (Fig. 18.7), the extreme position being when it is riding on the acetabular rim; usually it cannot be reduced fully into the acetabular socket. However, when it is possible to fully reduce the head, for example, with abduction of the leg, the condition is better called instability. Instability can be observed in the very young hip; diagnosis of instability in the newborn is the basis of harness treatment early after birth; instability can be seen in the adult hip but is less frequent and may be detected only with MRI (Fig. 18.8). As stated earlier, extreme subluxation, especially after some deformation of the rim, is difficult to distinguish from complete dislocation, where by definition, the femoral head is supposed to stay cephalad to the labrum (1). More recently the term structural instability is used for describing the potential or already demonstrable instability of the femoral head because of the small osseous socket of the residual
acetabular dysplasia (2) (Fig. 18.7); the aim is to distinguish soft tissue instability and laxity of the hip, an ill-defined diagnosis frequently made in sports medicine.
acetabular dysplasia (2) (Fig. 18.7); the aim is to distinguish soft tissue instability and laxity of the hip, an ill-defined diagnosis frequently made in sports medicine.
Prevalence and Etiology of Developmental Hip Dysplasia
Information regarding the incidence of developmental dysplasia of the hip varies greatly and depends on whether instability at birth is included; sonographic data or even radiographies are used for elicitation. This condition is most prevalent among Caucasians and very rare in native Africans. In Asia the incidence is rather low in China, especially in Hong Kong (3), but rather common in Japan (4). It is about four times more prevalent in females than in males (range: 2.4:1 to 9.2:1) (1,5). Inheritance with direct familial transmission is not frequent. However, the risk doubles to 12% when one parent is affected and increases to 36% when one parent and one child are affected (6). The higher incidence of dislocation with the intrauterine breech position points toward an etiologic role of mechanical factors (6). With increasing practice of ultrasound screening and early onset of harness stabilization, the incidence of complete dislocation has dropped substantially (7). Meanwhile, however, we regularly see adult hips with residual acetabular dysplasia which had normal sonographic findings at birth, indicating that reduced molding of the acetabulum can take place during adolescence with pathologic forces against the ossification centers in the acetabular margin, in other words even after the triradiate cartilage is closed (1).
Pathophysiology of Hip Dysplasia
To understand the pathophysiology of hip dysplasia it is helpful to have a look into the basic aspects of acetabular and femoral development as outlined in Chapter 5. In short, the anlage of the hip is formed very early in the embryonic development with scleroblastema arranged in two layers. The inner component is a spherical cluster of primitive chondroblasts forming the femoral head whereas the outer component consists of three disc-shaped masses: origin of ilium, ischium, and pubis (8,9,10). In the later course of growth the triradiate cartilage appears between the ossification centers of these three bones; it is a complex growth plate that builds the acetabulum during the fetal growth. Molding mechanical stimulus of the femoral head is essential for the basic shape and depth of the acetabulum whereas secondary ossification centers along the rim are responsible for the fine tuning of the definitive acetabular shape. The latter maturation process is finished only after the triradiate growth plate is
closed (1,11); this underlines the importance of the ossification centers along the rim (12). An interesting observation is that posttraumatic dysplasia after pediatric acetabular fracture was only observed with injury of the triradiate cartilage before the age of 5 years although majority of such fractures occur later in childhood. Above all, there is individual growth retardation as well as influence of adverse mechanical forces that are responsible for the development of hip dysplasia, taking place in fetal life and/or after birth. It can be successfully treated by re-establishing and maintaining centralized pressure of the femoral head; on the other hand, complete absence of the femoral stimulus will lead to a primitive, shallow, and often triangular-shaped acetabulum. With delayed reinsertion of the femoral head incomplete molding has to be expected, eventually leading to residual acetabular dysplasia but also to some minor deformity of the femoral head at the end of growth. Similarly, an incomplete centralized head leading to eccentric and excessive pressure will be followed by a retardation of growth of the involved acetabular edge; the amount of resulting deformity will largely depend on the onset and timeframe of adverse stimulation during the growth period.
closed (1,11); this underlines the importance of the ossification centers along the rim (12). An interesting observation is that posttraumatic dysplasia after pediatric acetabular fracture was only observed with injury of the triradiate cartilage before the age of 5 years although majority of such fractures occur later in childhood. Above all, there is individual growth retardation as well as influence of adverse mechanical forces that are responsible for the development of hip dysplasia, taking place in fetal life and/or after birth. It can be successfully treated by re-establishing and maintaining centralized pressure of the femoral head; on the other hand, complete absence of the femoral stimulus will lead to a primitive, shallow, and often triangular-shaped acetabulum. With delayed reinsertion of the femoral head incomplete molding has to be expected, eventually leading to residual acetabular dysplasia but also to some minor deformity of the femoral head at the end of growth. Similarly, an incomplete centralized head leading to eccentric and excessive pressure will be followed by a retardation of growth of the involved acetabular edge; the amount of resulting deformity will largely depend on the onset and timeframe of adverse stimulation during the growth period.
The pathomorphology of residual acetabular dysplasia in adults is commonly understood as excessive anteversion from the sagittal plane, and the insufficiency of coverage is anterolateral (13). However, more recent studies (14,15) have shown that 17% to 34% of classic acetabular dysplasias are retroverted (Fig. 18.9); in the main group approximately 10% show a pure anterior and less than 5% an exclusively lateral deficiency (13). In secondary acetabular dysplasia, such as after Perthes disease, retroversion is with up to 42% even more frequent (16,17) and in posttraumatic dysplasia as well as in the context of proximal femoral focal deficiency retroversion is present in 100% of the cases (Fig. 18.10) (12,18). Recognition of such variants of version is important to understand that such hips may suffer from impingement rather than from dysplasia (19) and should be considered during corrective surgery (20).
Association of Hip Dysplasia with Osteoarthritis
It is common understanding that residual acetabular dysplasia is a mechanical abnormality frequently leading to osteoarthritis (OA) of the hip (21,22,23). As a consequence of pathologic loading of a reduced area of force transmission (Fig. 18.11) (24), it is reported that by the age of 50 years 25% to 50% of the patients may suffer from secondary joint degeneration (25). Murphy et al. (26) found that with a load transmission area smaller than represented by a Wiberg lateral center edge (LCE) angle of 16 degrees, all hips would undergo end-stage OA. When combined with subluxation of the head, an “inevitability of disabling coxarthrosis” is to be expected (27); another study (28) specifies that dysplasia with additional subluxation would lead to total hip arthroplasty (THA) by the age of 45.
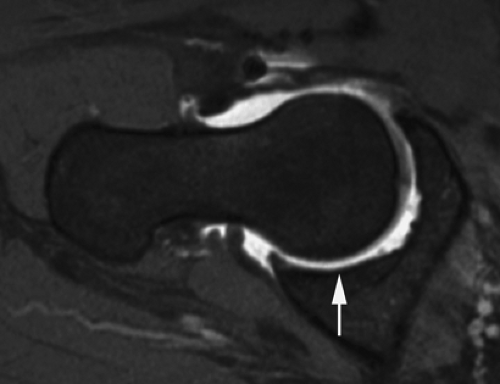
With better imaging techniques, such as MRI, it became evident that the process of joint degeneration in the dysplastic hip is not only eccentric in the osseous acetabular cavity but involves first the hypertrophic labrum that fatigues over time and/or undergoes avulsion with or without a bony fragment (Fig. 18.12). Degeneration and rupture of the labrum may not only decrease the stability of the femoral head but also reduce the sealing function and therefore the lubrication and load distribution within the joint-sufficient joint lubrication (29), both aspects explain why attempts to arthroscopically treat labral lesions in the presence of dysplasia have a very high and early failure rate (30). Klaue et al. (31) have called the labral rupture in the dysplastic hip a precursor of OA, an interpretation which was confirmed by long-term results after acetabular reorientation showing better outcome of hips with intact labrum (32).
Classification of OA of the dysplastic hip is routinely followed by the radiographic subdivision in three severity
grades as proposed by Tönnis (33). MRI studies, however, have shown that substantial cartilage damage can be present even before Grade 0, definition used for a normal hip; Beck et al. (34) have therefore proposed to additionally use an intraoperative visual classification system for cartilage damage with four severity steps; this may help to make surgical indications more precise and treatment results more meaningful. To quantify the deformity, a multitude of different radiologic parameters are proposed (35); there are classifications for joint congruity (36) as well as grading systems for the efficacy of treatment concepts (37



grades as proposed by Tönnis (33). MRI studies, however, have shown that substantial cartilage damage can be present even before Grade 0, definition used for a normal hip; Beck et al. (34) have therefore proposed to additionally use an intraoperative visual classification system for cartilage damage with four severity steps; this may help to make surgical indications more precise and treatment results more meaningful. To quantify the deformity, a multitude of different radiologic parameters are proposed (35); there are classifications for joint congruity (36) as well as grading systems for the efficacy of treatment concepts (37
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree