Hip Dislocation and Femoral Head Fractures
Kenneth J. Koval and Philip J. Kregor
Key Points
Introduction
Hip dislocations and femoral head fractures are usually the result of high-energy trauma.1–3 Associated injuries are common and include chest, abdominal, craniofacial, and other musculoskeletal trauma.1–7 Hip dislocations can be divided into anterior and posterior types, and femoral head fractures are classified according to the fracture location in the femoral head, as well as the presence of an associated fracture (e.g., femoral neck or acetabular fracture).
Treatment principles for patients with either injury include (1) careful clinical evaluation to detect associated injuries; (2) emergent gentle closed or, if necessary, open reduction, followed by assessment of hip stability; (3) radiographic evaluation (including computed tomography [CT] scan) for congruency of reduction and any associated fractures; and (4) treatment of residual joint incongruity, removal of clinically significant intra-articular fragments, and establishment of hip stability.
Epidemiology and Risk Factors
Posterior hip dislocations are much more common than anterior dislocations; anterior dislocations constitute 10% to 15% of traumatic dislocations of the hip,1-3,7 and posterior dislocations account for the remainder. True shear-type fractures in the frontal plane of the femoral head occur in 10% of posterior dislocations.7 Indentation lesions of the femoral head occur in 25% to 75% of anterior dislocations.7
Hip dislocations and femoral head fractures are usually associated with other injuries, either systemic or musculoskeletal. Suraci reported that 95% of patients who sustained a hip dislocation after a motor vehicle accident had an associated injury requiring inpatient management.5 Ipsilateral knee injuries are particularly common. In a series of 187 patients who sustained a dislocation or a fracture dislocation of the hip, Tabuenca and Truan reported that 25% sustained a major knee injury.8 In another series, 89% of patients who sustained a hip dislocation had visible evidence of soft tissue injury about the ipsilateral knee9; magnetic resonance imaging (MRI) revealed acute meniscal tear in 22% of patients, bone bruise in 33%, effusion in 37%, cruciate ligament injury in 25%, collateral ligament injury in 21%, and periarticular knee fracture in 15%.
Sciatic nerve injury occurs in 10% to 15% of hip dislocations.10–12 The peroneal division is affected more frequently than the tibial branch because it is tethered at the pelvis and at the fibular neck. Additionally, the fascicles of the peroneal division are fewer in number, larger, and less protected by connective tissue. Partial return of function in sciatic nerve palsy can be expected in more than 50% of affected patients.
Anatomy and Pathophysiology
The hip joint is inherently stable; more than 400 N of force is required to distract the hip.13 Hip stability is conferred by both osseous and ligamentous restraints, as well as by femoral head congruity with the acetabulum. The labrum deepens the acetabulum and enhances joint stability.14 The hip joint capsule is formed by thick longitudinal fibers supplemented by much stronger ligamentous condensations (iliofemoral, pubofemoral, and ischiofemoral ligaments) that run in a spiral fashion, preventing excessive hip extension. Seventy percent of the femoral head articular surface is involved in load transfer; therefore damage to this surface may lead to the development of post-traumatic arthritis.7
The main vascular supply to the femoral head originates from the medial and lateral femoral circumflex arteries—branches of the profunda femoral artery.1-3,7 An extracapsular vascular ring is formed at the base of the femoral neck with ascending cervical branches that pierce the hip joint at the level of the capsular insertion. These branches ascend along the femoral neck and enter the bone just inferior to the cartilage of the femoral head. The artery of the ligamentum teres, a branch of the obturator artery, may contribute blood supply to the epiphyseal region of the femoral head.
The sciatic nerve exits the pelvis at the greater sciatic notch. A certain degree of variability exists in the relationship of the nerve to the piriformis muscle and short external rotators of the hip. Most frequently, the sciatic nerve exits the pelvis deep to the muscle belly of the piriformis.
Force transmission resulting in hip dislocation or femoral head fracture arises from one of three common sources7,15-20: (1) the anterior surface of the flexed knee striking an object (e.g., dashboard injury); (2) the sole of the foot, with the ipsilateral knee extended (e.g., foot on brake pedal); or (3) the greater trochanter (e.g., lateral impact). Less frequently, the force resulting in hip dislocation may be applied to the posterior pelvis with the ipsilateral foot or knee acting as the counterforce. The direction of dislocation (anterior or posterior) is ultimately determined by the position of the lower extremity at injury and the direction of the pathologic force.
Anterior dislocations result from hip abduction and external rotation.7,21 The amount of hip flexion determines whether one sustains a superior or inferior (obturator) type of anterior hip dislocation. Inferior dislocations are the result of simultaneous abduction, external rotation, and hip flexion; superior (iliac or pubic) dislocations are the result of abduction, external rotation, and hip extension. In anterior dislocations, one may also sustain a femoral head impaction fracture secondary to the femoral head impacting the acetabular margin.
Posterior dislocations usually result from direct impact to the flexed knee with the hip in varying degrees of flexion.7,22 If the position of the hip is neutral or slightly adducted at the time of impact, a simple dislocation (no acetabular fracture) will likely occur. However, a femoral head fracture may occur as a result of avulsion by the ligamentum teres or impaction by the posterior acetabular rim. If the hip is in abduction, a posterior-superior rim of the acetabulum fracture usually results.
For the hip to dislocate, the ligamentum teres and a portion of the hip capsule must be disrupted.3 Tears of the acetabular labrum and associated muscle commonly occur.23 The capsule of the hip may be stripped off of the acetabulum or femur as a cuff secondary to rotational forces or may be split by direct pressure.21 In anterior dislocations, the hip capsule is usually disrupted anteriorly and inferiorly. In posterior dislocations, the capsule may be disrupted inferoposteriorly or directly posteriorly, depending on the position of the hip at impact.
Clinical Features and Diagnosis
Clinical Examination
A full trauma survey is essential because of the high-energy mechanism of injury and the likelihood of associated injuries. The patient may be obtunded or unconscious at the time of hospital presentation and unable to give a clear history of the accident or to complain of other areas of potential injury. Patients presenting with hip dislocations typically are unable to move the injured lower extremity and report severe hip pain.
Patients who have sustained a posterior hip dislocation usually present with the hip in a position of flexion, internal rotation, and adduction; those with an anterior dislocation present with the hip in marked external rotation with mild flexion and abduction. The appearance and alignment of the extremity, however, are dependent on the presence or absence of associated ipsilateral extremity injuries.
One must perform a careful neurovascular examination because injury to the sciatic nerve or to femoral neurovascular structures may have occurred at dislocation. Sciatic nerve injury may result from stretching of the nerve over the posteriorly dislocated femoral head. Posterior wall fragments from the acetabulum may have pierced or partially lacerated the nerve. Usually the peroneal portion of the sciatic nerve is affected, with little if any dysfunction of the tibial nerve. Injury to the femoral artery, vein, or nerve is rare but may occur as a result of an anterior dislocation.
Radiographic Evaluation
A dislocated hip is usually apparent on an anteroposterior (AP) radiograph of the pelvis (Fig. 48-1); femoral head fracture may be subtler and more difficult to diagnose. On the AP view of the pelvis, the two femoral heads should appear similar in size, and the hip joints symmetrical. In posterior dislocations, the affected femoral head should appear smaller than the contralateral side because of the closer distance of the femoral head to the radiographic cassette; in anterior dislocation, the femoral head should appear slightly larger than the normal hip.7 The position of the femoral shaft should be noted (adducted or abducted), as well as the relative appearance of the greater and lesser trochanters, because they may indicate pathologic internal or external hip rotation. One must carefully evaluate the femoral neck to rule out the presence of a femoral neck fracture before any manipulative reduction is performed. Although it is usually not necessary for diagnosis of hip dislocation or fracture dislocation, a cross-table lateral view of the injured hip may help to distinguish a posterior from an anterior dislocation.

Figure 48-1 A dislocated hip is usually apparent on the anteroposterior (AP) pelvis radiograph. A, An anterior dislocation. B, A posterior dislocation.
Full radiographic evaluation of a dislocated hip can usually wait until after an attempt is made at hip reduction and should include a repeat AP pelvis, cross-table lateral of the hip, and 45 degree oblique (Judet) views of the pelvis. The repeat AP pelvis is necessary to assess hip congruency after reduction; the cross-table lateral is used to evaluate the integrity of the femoral neck. Forty-five degree oblique (Judet) views of the hip are helpful in ascertaining the presence of associated femoral head fracture, osteochondral fragments, the integrity of the acetabulum, and joint congruence. The obturator oblique Judet view is particularly helpful in diagnosing femoral head and neck fractures, posterior wall fractures, and joint incongruity.
In general, CT scan is not needed before hip reduction unless a high level of suspicion for a nondisplaced femoral neck fracture is present. A 2 mm cut CT scan is usually obtained after closed hip reduction to assess the adequacy of reduction and to rule out associated acetabular and femoral head fractures3 (Fig. 48-2). Frontal plane CT reconstructions are helpful in characterizing associated femoral head fractures. If hip reduction cannot be attained through closed means, a CT scan should be obtained before open reduction to help identify offending structures, such as incarcerated bone fragments from the femoral head or a posterior wall fracture, or soft tissue interposition.
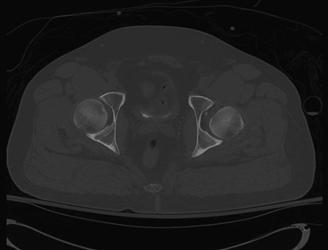
Figure 48-2 Computed tomography (CT) scan after closed reduction of the hip showing asymmetrical joint spaces with widening of the left hip joint.
The role of MRI in the evaluation of hip dislocation is controversial.7,23 MRI may prove useful in the evaluation of hip labrum integrity and femoral head vascularity; however, the usefulness of MRI in predicting femoral head osteonecrosis after dislocation has not been established.
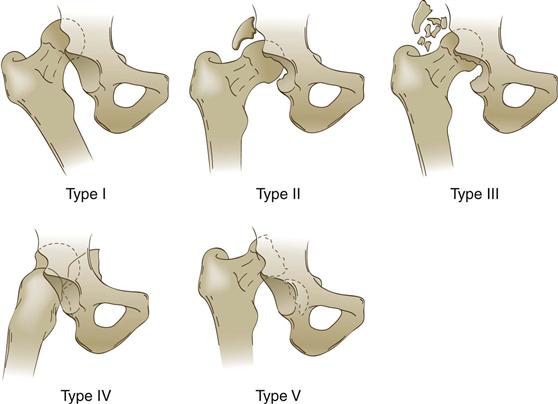
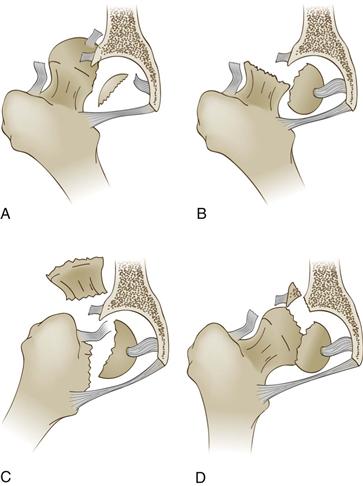
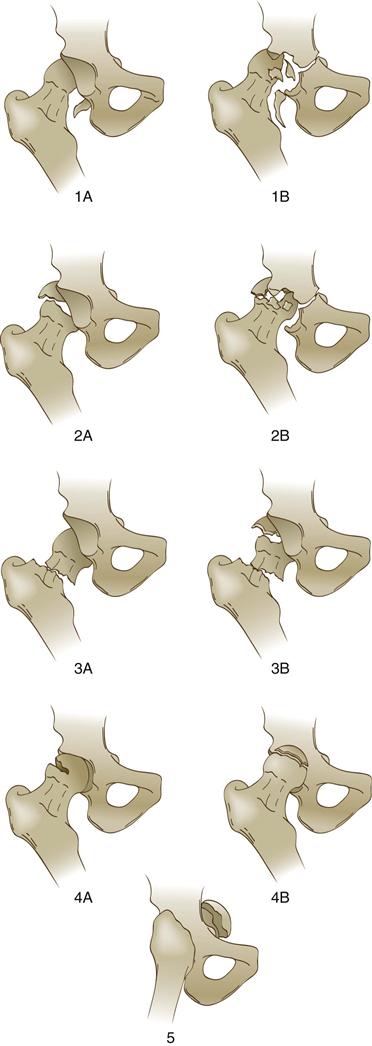
Classification
Several classifications have been described for hip dislocations and femoral head fractures (Boxes 48-1 through 48-5). In general, hip dislocations are classified on the basis of (1) the relationship of the femoral head to the acetabulum, and (2) the presence or absence of associated fractures. The Stewart and Milford classification for posterior hip dislocations also addresses the question of hip stability after reduction.24 The Brumback classification of femoral head fractures takes into account the size of the femoral head fragment, the direction of hip dislocation, and hip stability.25 The Orthopaedic Trauma Association (OTA) classification of hip dislocations and femoral head fractures is part of a universal classification system and is used primarily for research purposes.26