Traumatic/direct injury
Femoral neck/head fracture
Hip dislocation
Slipped capital femoral epiphysis
Nontraumatic
Corticosteroid use
Alcohol abuse
Idiopathic
Sickle cell disease
Caissons disease
Systemic lupus erythematosus
Cushing disease
Organ transplantation
Prior radiation therapy
Smoking
Pregnancy
Chronic pancreatitis
Coagulopathy
Chronic renal failure
Gaucher disease
Arteritis
Disseminated intravascular coagulation
Lipid disorders
Today, AVN is thought of as a multifactorial disease process including the risk factors previously listed and also in some patients a genetic predispositions to the development of disease. In a coagulation study, it was noted that 82 % of patients with AVN had at least one coagulation abnormality [11, 12]. Patients with AVN have also been found to have genetic polymorphisms in the genes for endothelial nitric oxide synthase (eNOS) which is involved in regulating the tone of blood vessels [13–16]. Genetic polymorphisms in the genes involved with collagen production, as well as alcohol and steroid metabolism, have been identified in patients with AVN [17–20]. Investigating for these rare associations is important, as treatment success for AVN can potentially be predicated upon the presence or absence of these risk factors.
Presentation
Patients with AVN typically are less than 40 years of age and present with a complaint of groin pain; however, the intensity of pain varies depending on the stage of AVN. They will typically deny any traumatic injury to the hip, and many will present with a history of a known risk factor. Pain in early stages is secondary to synovitis and an increased pressure in the femoral head as described by Ficat, as a result of venous congestion within the femoral head [1]. Patients without collapse of the femoral head typically complain of an insidious onset of a dull, deep ache; however, once subchondral fracturing and collapse occurs, the pain can become acutely severe [1]. In the early stages of disease, pre-collapse, patients will frequently have a normal range of motion; however, this will become limited secondary to pain with advanced stages of disease, especially with forced internal rotation of the hip. In advanced stages of AVN, after collapse of the femoral head has led to degenerative changes, patients will have findings consistent with end-stage osteoarthritis.
Imaging
Radiographic analysis of the hip should begin with anteroposterior (AP) and frog-lateral radiographs (Fig. 1). Since a majority of patients with AVN will have bilateral involvement, it is important to also evaluate the contralateral side [2]. The frog-leg lateral view is important to identify subtle changes in the subchondral bone of the femoral head which can be missed on AP and cross-table lateral views and is important in staging of the disease [2]. Plain radiographs have also been historically used to determine the proportion of the femoral head involved by measuring the arc of involvement on the AP and lateral radiographs and adding these together [21].
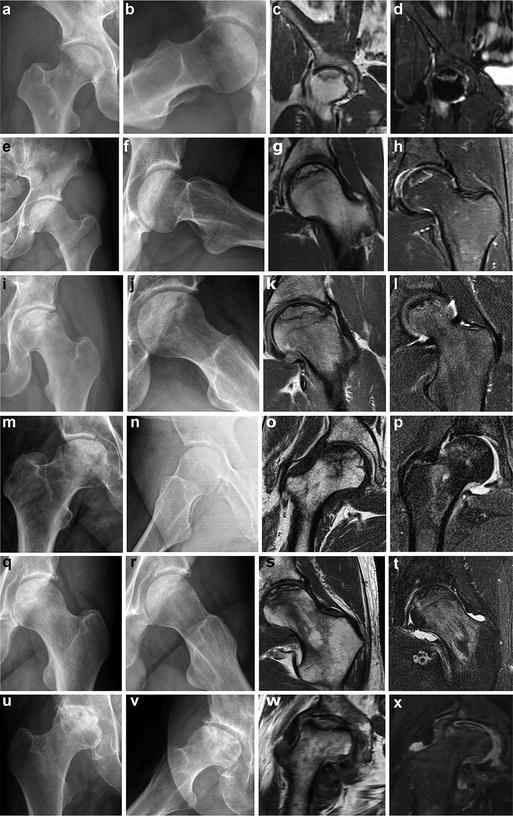
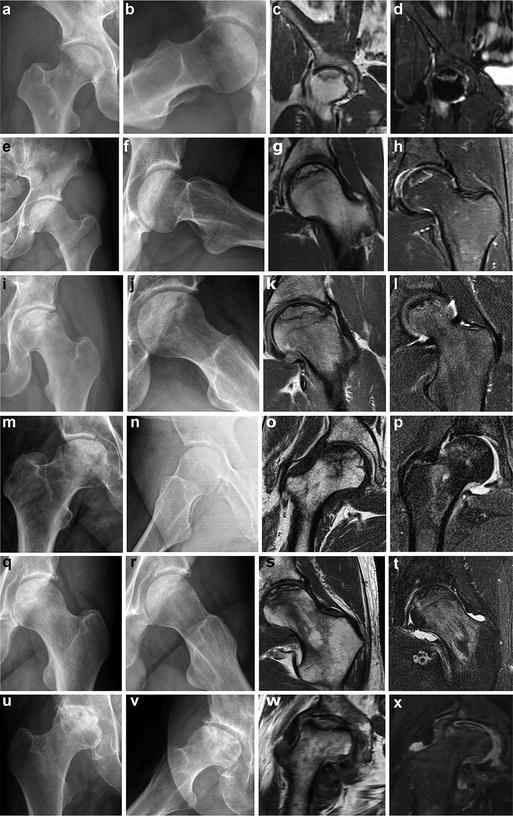
Fig. 1
Corresponding radiographs (AP and frog leg lateral) and MRIs (coronal T1 and T2) for patients with various stages in the Steinberg classification [23]. Stage 1 (a–d) shows no radiographic features of AVN (a and b), however, features readily apparent on MRI (c and d). Stage 2 (e–h) shows subtle increase sclerosis in the femoral head on radiographs (e and f) and features of AVN on MRI (g and h). Stage 3 (i–l) shows collapse of the articular surface with a “crescent sign” on radiographs (i and j), along with corresponding MRI images (k and l). Stage 4 (m–p) radiographs show flattening of the femoral head without joint space narrowing (m and n), along with corresponding MRI images (o and p). Stage 5 (q–t) radiographs show joint space narrowing, with minimal involvement of the femoral head (q and r), along with corresponding MRI images showing AVN (s and t). Stage 6 (u–x) radiographs show advanced degenerative changes (u and v), along with corresponding MRI images showing AVN (w and x)
Currently, there is no modality that is 100 % sensitive and specific to diagnose AVN of the femoral head. If a patient presents with a history and physical exam consistent with a diagnosis of AVN, an MRI can be ordered to diagnose and also evaluate the extent of AVN [2, 22–24]. The use of MRI is very effective in detecting AVN at the earliest stages and is 98 % sensitive and 98 % specific. Initially edema appears in the femoral head as a hypointense signal on T1-imaging and hyperintensity on T2 [22, 23].
Staging
In order to formulate a treatment plan, accurate staging of the disease is imperative. Staging of the disease also allows the physician to be able to counsel the patient on the disease course and treatment options. Historically, the classification system by Ficat (Table 2) is most commonly used [1]. This system uses plain radiographs to evaluate the femoral head and separates early from late-stage AVN by the presence of a “crescent sign,” signifying a fracture in the subchondral bone [1]. Similar to the Ficat classification, the Steinberg classification (Table 2) also uses the “crescent sign” to separate early from late-stage AVN [23].
Table 2
Radiographic stages for AVN of the femoral head
Stage | Ficat classification [1] | Steinberg classification [23] |
|---|---|---|
0 | No symptoms | No symptoms |
Normal X-rays | Normal X-rays | |
MRI nondiagnostic | MRI nondiagnostic | |
1 | Mild pain in the affected hip | Mild pain in the affected hip |
Pain with internal rotation | Pain with internal rotation | |
Normal X-ray | Normal X-ray | |
MRI diagnostic | MRI diagnostic | |
2 | Worsening or persistent pain | Worsening or persistent pain |
Increased sclerosis or cysts in the femoral head | Increased sclerosis or cysts in the femoral head | |
3 | Subchondral collapse producing a crescent sign | Subchondral collapse producing a crescent sign |
Flattening of the femoral head | ||
Normal joint space | ||
4 | Collapse of head | Flattening of the femoral head |
Flattened head | Normal joint space | |
Decreased joint space | ||
5 | Joint space narrowing with/without femoral head involvement | |
6 | Advanced degenerative changes |
With the advancement of MRI, it has become easier to detect the subtle changes of early AVN [22, 23]. Since physicians are able to detect AVN at an earlier stage, MRI is used to determine characteristics which aid in predicting outcomes in certain patients [24–26]. The most important prognostic factor is the percent involvement of the weight-bearing portion of the femoral head.
The Association Internationale de Recherche sur la Circulation Osseuse (ARCO) developed a classification system that is the most complete [27]. The ARCO classification combines plain film radiographs, MRI, and bone scan findings to determine different stages of disease (Table 3); however, due to the multiple stages which a patient can fall into, it is difficult to use and apply in clinical practice.
Stage | Findings | Femoral head involvement |
|---|---|---|
0 | Negative plain radiographs, CT, bone scan and MRI | None |
I | MRI or bone scan positive | I-A: <15 %a |
I-B: 15–30 %a | ||
I-C: >30 %a | ||
II | Plain radiographs show osteosclerosis, cyst formation, and osteopenia | II-A: <15 %a |
No crescent sign | II-B: 15–30 %a | |
I1-C: >30 %a | ||
III | Presence of crescent sign | III-A: <15 % crescent sign or <2 mm depression of femoral headb |
III-B: 15–30 % crescent sign or 2–4 mm depression of femoral headb | ||
III-C: >30 % crescent sign or 4 mm depression of femoral headb | ||
IV | Joint space narrowing with acetabular degenerative changes (sclerosis, cyst formation and osteophytes) |
Treatment Options
Treatment modalities for AVN can be divided into two main categories: pre-collapse and post-collapse. Many of the treatments that are utilized in the pre-collapse phase of AVN are not effective once the femoral head has collapsed. If the disease process is halted in the pre-collapse phase, patients can avoid THA and other salvage-type procedures. This group encompasses stages 0–2 of the Steinberg classification.
Pre-collapse AVN
Nonoperative Modalities
Statins
Hyperlipidemia is commonly seen in patient with AVN. One study noted that 12 out of 19 patients who were receiving corticosteroids and developed AVN had elevated lipid levels, with many patients requiring a lipid lowering agent [28]. Interest has grown for the use of statins both in prevention and treatment of early-stage AVN. Pritchett reviewed a series of 284 patients who received steroids for a variety of reasons [29]. All patients received at least one statin during this time, some patients received two or more. Only 1 % of patients developed AVN in the statin treatment group. It is believed that etiologies such as fat emboli and metabolic abnormalities contribute to the development of AVN in this patient population [29]. The exact mechanism for the effectiveness of statins has yet to be fully understood. Experimentally, statins have been found to lower the intramedullary pressure and increase femoral bone density in femoral head AVN [30, 31].
Stanozolol
A hypercoagulable state has been hypothesized to contribute to the pathogenesis of AVN. One study investigated the relationships between certain hypercoagulable states and the development of AVN. It was found that a Factor V Leiden mutation as well as homocysteinemia was more common in patients with multifocal AVN than in the control groups [13]. Medications that can reverse their hypercoagulable states are currently under investigation for the treatment of early-stage AVN. Stanozolol, a synthetic steroid, which is commonly taken orally for anemia and hereditary angioedema is one of these agents. Glueck studied a group of five patients with AVN; four of these patients had hypofibrinolysis. All patients were treated with Stanozolol. Three of the patients had normalization of hypofibrinolysis and resolution of their hip symptoms, although one progressed radiographically [14].
Bisphosphonates
Bisphosphonates work by inhibiting osteoclasts which prevents bone resorption which leads to net bone formation and are commonly used to treat osteoporosis. These properties are appealing in the setting of AVN, since it is thought that collapse of the femoral head is due to osteoclasts removing necrotic subchondral bone. To this end, alendronate has been studied in the treatment of AVN. The results indicate that patients had significantly less pain, increased their walking time and also hip range of motion. Radiographic progression was typically minimal; however, 10 % of patients required surgery during the study [32, 33]. The use of bisphosphonates for the treatment of AVN has also been shown to be efficacious in randomized clinical control trials. Alendronate or placebo was given to patients with Steinberg stage IIC or IIIC nontraumatic AVN of the femoral head [34]. At 24-months of follow-up, in the patients who received alendronate, only two patients (7 %) went onto collapse, while 19 (76 %) in the placebo group collapsed [34]. However, in a recent study by Chen, similar patients with Steinberg stage IIC or IIIC AVN were again randomized to receive alendronate or placebo to determine the effect of the medication on the progression of AVN and subsequent need for total hip arthroplasty [35]. The results of this study showed no difference between the alendronate and placebo group with 13 % of the alendronate group and 15 % of the placebo group progressing to total hip arthroplasty [35].
Operative Modalities
Core Decompression
Increased femoral head intramedullary pressure is thought to be part of the pathophysiology of AVN. The increase in pressure decreases blood flow through the retinacular vessels within the femoral neck which provide perfusion of the femoral head. With decreased perfusion of the terminal aspect of the femoral head, necrosis subsequently develops. Core decompression has been proposed as a surgical option to reduce the intramedullary pressure within the femoral head [36]. Core decompression is a relatively minor outpatient surgery that is typically only used in early AVN before femoral head collapse has occurred. The procedure is performed supine on a radiolucent table. Fluoroscopic imaging is required to localize the areas of AVN of the femoral head. Through a lateral incision over the greater trochanter, a guide wire can be inserted through the femoral neck and into the femoral head under fluoroscopy. Cores are then removed from the femoral head and neck to decrease the intramedullary pressure. Caution should be utilized when approaching areas of necrosis as this can dislodge the necrotic lesion from the femoral head.
Hungerford and Ficat were among the first to describe the utilization of core decompression for Ficat stages 0, 1, and 2 AVN [37]; however, core decompression was initially described by Graber-Duvernay for osteoarthritis in 1932. Core decompression, in the early setting, has been found to delay progression in approximately 60 % of patients. Postoperatively patients are usually made protected weight bearing for 1–2 weeks depending on the size of core that was taken intraoperatively, with most patients able to wean from crutches within 1 month of surgery. Complications associated with the procedure include surgical site infection, postoperative femoral head collapse, and subtrochanteric fracture. The risk of subtrochanteric fracture can be minimized by ensuring that the lateral cortex of the femur is entered proximal to the level of the lesser trochanter.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








