Hip Arthroscopy for Structural Hip Problems
Marc Philippon, Bruno G. Schroder e Souza and Karen K. Briggs
Key Points
Introduction
Arthroscopy has been used successfully to address intra-articular hip pathology due to functional or morphologic alterations of the hip. Historically, trauma was believed to be the cause of most labral tears in the hip; however, improved understanding of physiopathology has revealed that up to 80% of such lesions are related to subtle structural problems.1 For many years, this led surgeons to classify most hip osteoarthritis cases as primary or idiopathic.2,3 However, both the femur and the acetabulum can present with abnormal shapes that predispose to impingement, instability, or both, which ultimately induce degenerative changes of osteoarthritis.2,4,5 Hip arthroscopy aims to treat intra-articular damage and its causes, preferably in the early stages of the disease. It has been shown to improve symptoms and is expected to improve joint biomechanics to prevent or delay the natural progression of joint degeneration.5
A common structural problem is developmental dysplasia of the hip (DDH), in which the acetabulum is shallow, is inclined laterally, and insufficiently covers the femoral head.6–8 In this situation, the labrum is known to function as a key factor in joint stability and is usually hypertrophic.6 Higher stress loads on the lateral margin of the acetabulum and labrum were found to occur in an inverse relation to acetabular coverage, as shown by the center edge angle.9 The lesser the coverage, the greater the stresses that are found, and the earlier joint degeneration is observed.8,10 Whenever the labrum fails to manage those stresses, it presents with a tear or detachment. Subluxation, joint incongruence, and rapid progression to joint degeneration have been documented.10,11
On the other hand, the acetabulum can present with excessive coverage leading to joint impingement at the extremes of range of motion.12,13 Examples of such morphologic alterations include coxa profunda and protrusio acetabuli, in which the center of rotation of the femoral head lies too medially in an abnormally deep socket.14 Another condition is general acetabular retroversion, in which the whole acetabulum is oriented posteriorly, producing anterior overcoverage, predisposing to impingement against the femoral neck during hip flexion, and relative undercoverage posteriorly. Focal acetabular retroversion is seen more commonly, and the superior hemisphere of the acetabulum is posteriorly oriented, provoking localized impingement on the anterior superior aspect of the acetabular rim, proximal to the psoas valley or U, in between the origins of the heads of the rectus femoris muscle.14
In many instances, the femur is the site of the deformity. A posterior tilt of the femoral head relative to the axis of the femoral neck is often observed after slipped femoral capitis (clinical or subclinical).2,3,5 The decreased femoral head-neck offset is responsible for a cam effect, in which that region is forced into the acetabulum, especially on hip flexion, adduction, and internal rotation.12,15 This effect can also be elicited in maximum abduction, when the bump is more laterally based. In many cases, the center of rotation of the femoral head is in line with the femoral neck axis, but insufficient offset is present. Cam deformities seem to be deleterious to the hip joint because they can predispose to impingement at earlier degrees of range of motion, inducing cartilage and labral damage.9,12,16 Other variations on proximal femur morphology, such as excessive anteversion and coxa valga, can be components of DDH and can worsen joint function.
To restore normal interaction between femur and acetabulum, hip arthroscopy can be used to modify the shape of the femoral head-neck junction and the acetabular rim.17,18 When correctly indicated, the arthroscopic approach provides the great advantages of effective treatment, low morbidity, reproducibility,19,20 and excellent results.21–23
Indications/Contraindications
Hip arthroscopy is indicated to correct intra-articular conditions, specifically, labral tears, chondral lesions, loose bodies, ligament teres pathology, and capsular disease, which often are observed in the presence of trauma or functional or structural alterations in the hip.24–26 Femoroacetabular impingement (FAI) is probably the most common indication. The presence of symptoms, along with radiographic evidence of impingement and chondral and/or labral lesions, is a clear indication for surgical treatment.17,23,24,26-28 No conservative measure has been shown to be effective when intra-articular lesions are already present. Operative treatment focuses on improving clearance of hip motion and alleviating femoral abutment against the acetabular rim to relieve pathologic stresses in the labrum and the articular cartilage.9 This is achieved by acetabular osteoplasty (or rim trimming) and femoral osteochondroplasty (cam resection).17,18 Localized acetabular retroversion and the presence of an anterior-superior bump in the femoral head-neck junction are optimal indications. A completely deepened socket, as in coxa profunda or protrusio acetabuli cases, is treatable arthroscopically; however, the procedure may be technically demanding. Besides correcting morphologic factors leading to impingement, treatment of concurrent intra-articular lesions is paramount.
Mild hip dysplasia can be treated with arthroscopy.29 Great functional and pain improvement was reported when intra-articular loose bodies and ligamentum teres tears were present in the dysplastic joint.29 Although labral repair may reestablish joint physiology in mildly dysplastic joints, no arthroscopic treatment has been developed to date for the treatment of acetabular bone undercoverage. In the presence of hip dysplasia, complete resection of the labrum is contraindicated because the condition worsens joint instability, and this has been related to faster development of joint degenerative disease.5 More severe hip dysplasia is often better treated with open approaches in young patients.30 However, even in these patients, hip arthroscopy can be performed before or after reorientating osteotomies to mend intra-articular pathology.31
Advanced joint degenerative disease, with massive chondral loss and radiographic joint space of less than 2 mm, has been related to worse outcomes23 and is a relative contraindication for hip arthroscopy. In such patients, mechanical causes of symptoms such as loose bodies or an entrapped labrum may be possible indications for surgery. Previous hip surgery32,33 or a history of joint infection34 is not a contraindication. However, effective revision hip arthroscopy is a demanding procedure because scar tissue is often present, as is altered anatomy in some cases. Extra-articular infection without joint extension should be treated completely before any arthroscopic procedure can be considered because of the risk of development of pioarthrosis. Obesity poses extra difficulty for the procedure, in that joint distraction may be challenging and the instruments can become hard to maneuver or may not reach the necessary depth.35 Other conditions that impede adequate join distraction such as severe protrusio acetabuli, dense heterotopic bone formation, and joint ankylosis are also contraindications.35
Preoperative Planning
Preoperative assessment begins with an adequate history and physical examination.36,37 The physician should be able to distinguish between intra-articular and extra-articular sources of pain based on symptoms and signs elicited by the evaluation.6,36,38,39
Radiographic assessment is paramount in defining the cause of the condition.18,36,37 Almost all morphologic causes of hip problems can be evident on a series of radiographs (Tables 54-1 and 54-2). The anteroposterior (AP) pelvis in the supine position, a lateral view of the proximal femur (cross-table, Dunn, or its modifications), and a false profile of the pelvis are often enough to disclose both impingement and dysplasia. An AP pelvis roentgenogram should be obtained in all patients. Pelvic positioning must be considered when radiographic signs associated with pincer impingement are interpreted. With the coccyx and the symphysis pubis aligned, the pelvis should be in neutral flexion-extension.40 Pincer-type impingement can be diagnosed on this view when the patient has acetabular retroversion and coxa profunda.13 Dysplasia and proximal femur deformities can also be seen on this view.40,41 Signs of acetabular dysplasia are presented in Table 54-2. The center edge angle is of special interest for surgical planning. Bone resection for correction of pincer deformity should not decrease that angle to below 25 degrees because of the risk of creating instability.42,43 Intraoperative fluoroscopic methods to quantify the amount of actual resection have been described.44,45 Another study correlated the amount of resection in millimeters with the reduction in the center edge (CE) angle. The formula derived from that study (CE angle reduction = 1.8 + [0.64 × rim reduction in millimeters]) also provides an estimate for maximal resection.46
Table 54-1
Radiographic Signs of FAI
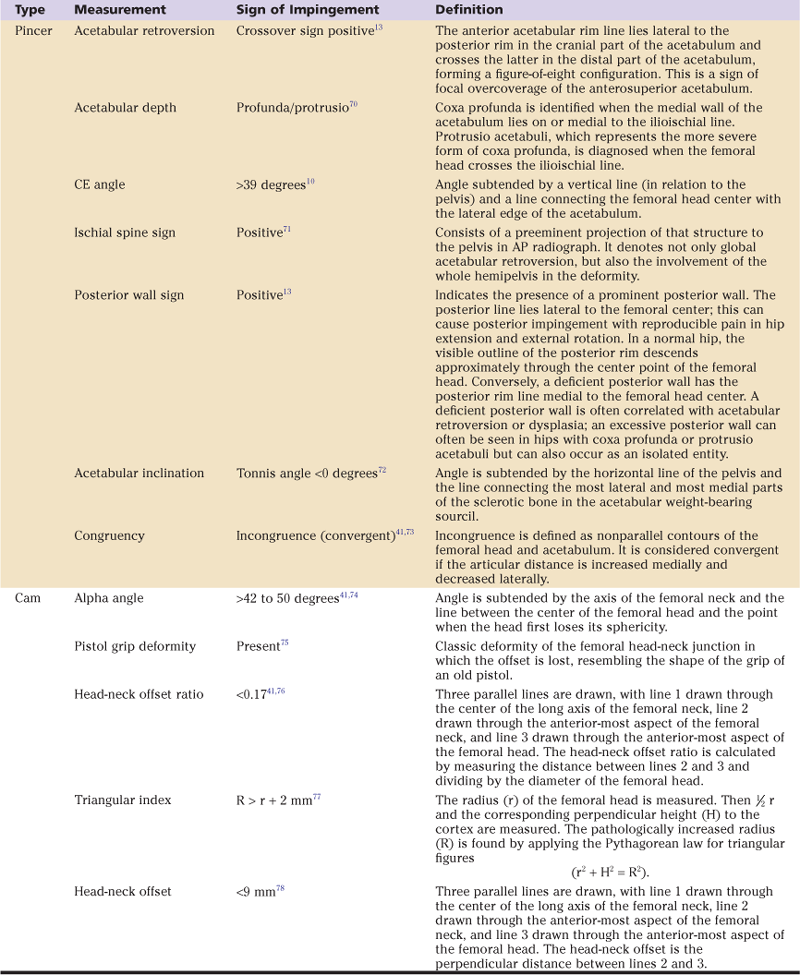
AP, Anteroposterior; CE, center edge; FAI, femoroacetabular impingement.
Table 54-2
Radiographic Signs of Hip Dysplasia
| Measurement | Sign of Dysplasia | Definition |
| Acetabular inclination | Tonnis angle >10 degrees79 | Angle subtended by the horizontal line of the pelvis and the line connecting the most lateral and most medial parts of the sclerotic bone in the acetabular weight-bearing sourcil. |
| CE angle | <25 degrees10 | Angle is subtended by a vertical line (in relation to the pelvis) and a line connecting the femoral head center. |
| Extrusion index79 | >20%80 | The femoral head is measured horizontally. The index is calculated by dividing the size of the uncovered portion of the femoral head by the size of the head. |
| Congruency | Incongruence (convergent)41,73 | Incongruence is defined as nonparallel contours of femoral head and acetabulum. It is considered divergent if the articular distance is increased laterally and decreased medially. |
| Shenton’s line | Superior migration of the femur41 | Line formed by the inferior margin of the femoral neck and the superior border of the obturator foramen. |
| Lateralization of the femoral head | Lateralized (>10 mm)41 | The hip center is considered lateralized if the medial aspect of the femoral head is greater than 10 mm from the ilioischial line. |
| Sharps’ acetabular angle | >42 degrees81 | Angle subtended by the horizontal line of the pelvis connecting both teardrop signs and the line of the teardrop to the most lateral point of the acetabular articular surface. |
| Anterior center edge angle (VCA) | <20 degrees48 | Angle subtended by the line connecting the center of both femoral heads and the one between the center of the femoral head and the anterior-most edge of the acetabulum articular surface. |
CE, Center edge; VCA, vertical-center-anterior.
A lateral view of the proximal femur is essential for the diagnosis of cam impingement. Because the abnormality is typically seen in the anterolateral portion of the head-neck junction, it may not be evident on an AP pelvic radiograph. A cross-table lateral view (with the hip in 10 degrees of internal rotation) is the authors’ preferred view. Correlation between radiographs and surgical findings is paramount in guiding resection of the correct amount of bone in the femoral neck. Remnants of the physeal scar can be used to guide the surgeon as to where to begin the femoral osteoplasty. Although insufficient resection can cause persistent impingement, over-resection can lead to risk of femoral neck fracture47 and may impair an adequate sealing effect in the labrum.44
In some cases, signs of dysplasia can be disclosed only in the false profile view of the pelvis, as described by Lequesne.48 The anterior center edge angle (vertical-center-anterior [VCA]) is calculated in this radiologic view. The patient stands at an angle 65 degrees oblique to the x-ray beam, with the foot on the affected side parallel to the x-ray cassette. The focal distance is 1 meter. The beam is centered by using the tip of the greater trochanter as the horizontal center. The vertical center is located midway between the symphysis pubis and the anterior superior iliac spine.40,41,48 A VCA angle of 25 degrees is regarded as normal, 20 to 25 degrees as borderline, and less than 20 degrees as pathologic. The threshold of abnormality of the VCA angle may be even lower. Some studies suggest that the normal value is equal to or greater than 17 degrees.49 The presence of hip dysplasia should preclude further bone resection and alerts the surgeon to be more conservative with the labrum. Yet on this view, joint space narrowing on the anterior superior or on the posterior inferior aspect of the acetabulum can be evidence of more advanced joint degeneration than might be expected by isolated analysis of the AP radiograph.41
Description of Techniques
Arthroscopic Treatment of Femoroacetabular Impingement
After thorough inspection, a capsulotomy is performed about 1 cm distal and parallel to the labral margin. Leaving a cuff of intact capsule next to the labrum will ease visualization of the peripheral compartment and may help to prevent postoperative adhesions. Although preserving the iliofemoral ligament by avoiding excessive anterior extension of the capsulotomy anteriorly is desired, this should not impede adequate exposition and instrumentation. The ligament can be repaired afterward. At all stages, the capsulotomy should be performed under direct visualization. The lateral retinacular vessels, which are an important source of blood supply to the femoral head, lie on the lateral synovial fold and should be at risk if blind manipulation is performed too laterally.47
Acetabular Rim Trimming With Labral Takedown
When the labrum is detached at its base, it should be separated in the watershed zone, so that the underlying bone deformity (pincer) can be corrected. The labrum is reattached with suture anchors. First, the chondro-labral junction is delineated by controlled application of a monopolar radiofrequency (RF) chisel to better define the tear to prevent sacrificing healthy labral tissue. Chondral flaps are removed after demarcation with the aid of the same RF device. The area between the labrum and the capsule is then dissected with a shaver, and the labrum is completely detached from the acetabular rim. The acetabular bone overhang, responsible for the pincer deformity, is removed, before or after complete labral detachment, with a motorized burr blade. The amount of rim resection should be estimated preoperatively by analysis of the image examinations. The lateral portal is used to perform most of the resection, although switching of portals is essential for assessment of complete work. The current labral repair technique will be detailed in a separate item.
Acetabular Rim Trimming Without Labral Takedown
In cases without labral tear and in which a minimum amount of acetabular bone resection is required, rim trimming can be performed without labral takedown. To obtain adequate space to work between the capsule and the labrum, articular traction is released, the capsulotomy is extended, and the peripheral compartment is usually treated first. With a shaver in the space between the capsule and the labrum, the resection is then performed as planned (Fig. 54-1). Articular traction is introduced again, and inspection of the labrum is performed. The stability of the labrum should be thoroughly inspected to ensure adequate support from the remaining acetabular rim. If inadequate bone remains, failure of the watershed zone is expected (Fig. 54-2). On revision surgery, in cases with no additional fixation of labrum to bone, intraoperative findings showed a labral tear at the transition (watershed) zone and adherence of the labrum to the adjacent capsule, despite no history of new trauma. Anchor placement with suture fixation of the labrum to the acetabulum is recommended despite not taking down the labrum (Fig. 54-3). Besides preventing failure of the watershed zone, this practice allows a more active rehabilitation process, which is believed to help prevent adhesions and to allow early return to most activities.
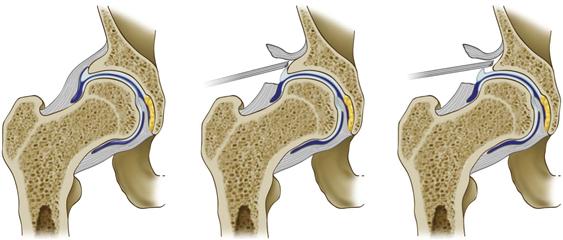
Figure 54-1 Illustration demonstrating rim trimming of the acetabular rim for pincer impingement without takedown of the labrum.
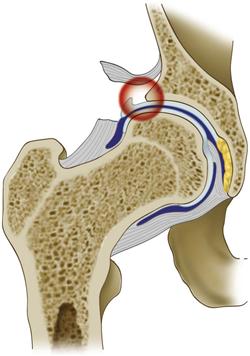
Figure 54-2 If the labrum is not repaired, after rim trimming without labral takedown, the abnormal mobility of the labrum causes the thin chondro-labral junction to fail. Labral tear and capsule-labral adhesions have been documented in this situation.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








