Fig. 1
Normal hip anatomy. Fat-suppressed T1-weighted coronal (a, b), sagittal (c, d), and axial oblique (e) images with intra-articular gadolinium. (a, b) The normal triangular-shaped labrum is shown by the small thin arrow. The joint capsule inserts several millimeters above the acetabular rim (medium-sized arrow) forming a normal recess. The ligamentum teres arises (short thick arrow) from the fovea capitis and extends to the transverse ligament. The long thin arrows depict the junction of the ligamentum teres and the transverse ligament. The circular fibers of the zona orbicularis (open arrow). (c) The triangular cross-section of the anterior and posterior labra (arrows). (d) The transverse ligament spans the acetabular notch (arrow). (e) The anterior triangular-shaped labrum (small arrow), the posterior joint capsule attachment at the base of the posterior labrum (large thick arrow), and the small posterior inferior sulcus at the junction of the transverse ligament and labrum (long thin arrow) (http://www.springerimages.com/Images/MedicineAndPublicHealth/1-10.1007_s00256-006-0105-5-0)
Fig. 2
Hip joint anatomy. (1) Ilium, (2) capsula articularis, (3) perilabral recess, (4) acetabular labrum, (5) head of femur, (6) articular cartilage, (7) acetabulum , (8) fovea, (9) ligamentum teres, (10) transverse ligament (http://www.springerimages.com/Images/MedicineAndPublicHealth/1-10.1007_s13244-010-0023-x-1)
Bony Anatomy and Alignment
Significant variability exists in the morphology of the proximal femur and acetabulum. Specific aspects of femoral and acetabular alignments have significant clinical relevance and impact joint biomechanics. Both the angle of inclination and the amount of femoral torsion are characteristics of femoral anatomy that affect the function of the hip joint. The angle of inclination, or neck-shaft angle, is formed by the axis of the head and neck of the femur with respect to the axis of the shaft of the femur. The normal angle is approximately 125 degrees [3]. The neck-shaft angle determines the size of the femoral offset, the distance from the center of rotation of the femoral head to a line bisecting the long axis of the femur. The neck-shaft angle of the femur and resultant femoral offset affect the mechanical advantage of the hip abductors. Decreased neck-shaft angles (coxa vara) increase the moment arm of the abductors and increase joint stability due to increased coverage of the femoral head in the acetabulum. A shorter, more valgus femoral neck reduces the offset and decreases the moment arm of the hip abductors requiring larger abductor forces and potentially increased contact forces at the hip joint. Femoral version (torsion) is defined as the angular difference between the axis of the femoral neck and transcondylar axis of the knee and, in adulthood, is normally about 15 degrees [3]. Anteversion is an increase in the angle of femoral torsion. While a decrease in the angle of femoral torsion is known as retroversion. Excessive anteversion and retroversion require compensatory rotation (medial and lateral, respectively) at the hip joint to maintain joint congruency. Excessive anteversion may also change the moment arm of the gluteus medius and thus decrease its efficiency. Specifically, increased femoral anteversion displaces the greater trochanter posteriorly thus decreasing the lever arm of the gluteus medius and subsequently its strength [4]. Hip contact forces have been shown to increase with increased femoral anteversion [5]. The angle formed by the line connecting the center of the femoral head and the lateral rim of the acetabulum forms an angle with vertical known as the central edge angle, with angles greater than 25 degrees being considered normal [3]. Examination of proximal femoral and acetabular alignment using computed tomography has demonstrated relationships between these measures [6]. Mean femoral neck version was found to be positively correlated with acetabular version [6]. A negative correlation was found between femoral version and acetabular inclination [6]. Femoral neck-shaft angle was positively correlated with acetabular version and negatively correlated with age [6]. Both acetabular version and central edge angle were observed to be positively correlated with female gender [6].
Capsular and Ligamentous Anatomy
The capsule of the hip joint consists of a cylindrical arrangement of dense fibers connecting the acetabulum and proximal femur through firm proximal attachments to the acetabular periosteum and distal attachments to the intertrochanteric line on the femur anteriorly [7]. The anterior attachments extend from the intertrochanteric line to the greater trochanter superiorly and to the lesser trochanter inferiorly [7]. Posteriorly it has been observed that the fibers of the capsule lack a direct distal attachment on the femur but the zona orbicularis forms “an arched free border” around the femoral neck medial to the intertrochanteric crest [7]. Where the acetabulum is incomplete inferiorly, the capsule is attached to the transverse acetabular ligament [7]. Thickness of the capsule has been observed to vary, but it is reinforced consistently by the capsular ligaments.
Anteriorly, the strongest of the capsular ligaments, the iliofemoral ligament, reinforces the capsule with longitudinally oriented fibers spanning between the intertrochanteric line and the ilial portion of acetabular rim and anterior inferior iliac spine (Fig. 3). It is suggested that this ligament is reinforced by the tendinous origin of the rectus femoris muscle [7].


Fig. 3
Anterior view of the right hip capsule. Observe the presence of the iliofemoral ligament with its two components: superior (white arrows) and inferior fascicles (black arrows) (http://www.springerimages.com/Images/MedicineAndPublicHealth/1-10.1007_978-1-4419-7925-4_7-8)
The iliofemoral ligament possesses two distinct thickened bands, superiorly and inferiorly along its course, with a thinner central region [7] (Fig. 4). Its fibers appear maximally taut in extension and lax in flexion of the hip [7]. It has been suggested that due to the position of this ligament anterior to the hip joint, it has a special role in the maintenance of erect posture, balancing the force of the body’s weight on the femur during standing.
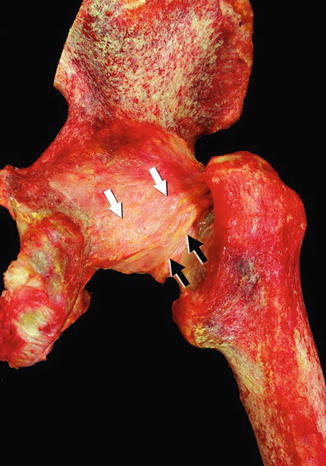
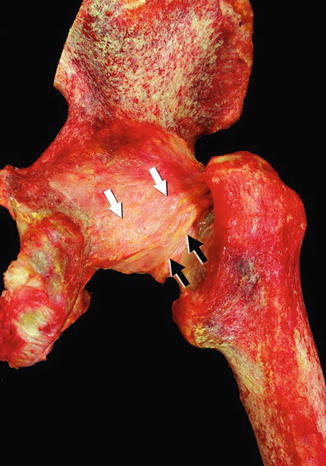
Fig. 4
Posterior view of the right hip joint. Observe the presence of the ischiofemoral ligament (white arrows) and femoral arcuate ligament (black arrows) that passes below the first one (http://www.springerimages.com/Images/MedicineAndPublicHealth/1-10.1007_978-1-4419-7925-4_7-9)
The pubofemoral ligament spans from its proximal attachment at the obturator crest and superior pubic ramus to the intertrochanteric fossa. An extracapsular portion of this ligament has been observed inferior to the acetabulum [7]. The intracapsular portion courses perpendicular to the zona orbicularis. Distally at the femoral attachment, the pubofemoral ligament blends with the inferior band of fibers of the iliofemoral ligament at the attachment site on the lesser trochanter [7]. This ligament has been observed to exhibit maximal tautness in abduction and laxity when the hip is in an adducted position [7].
The ischiofemoral ligament is attached to the acetabular rim and labrum and the inner surface of the greater trochanter. Posteriorly the ischiofemoral ligament reinforces the joint capsule and can be subdivided into two bands (superior and inferior) which both run in an oblique direction between the acetabular rim and labrum and the inner surface of the greater trochanter [7]. The thickness of the capsule is decreased posteriorly with thinner and looser fibers except at the distal attachment on the femur where the transversely oriented fibers of the zona orbicularis provide reinforcement [7]. This ligament has been suggested to restrict internal rotation due to the length and tautness of its fibers with this motion at the hip joint [7].
The zona orbicularis is a circumferential band of fibers which forms an annular ligament at the hip joint. It attaches superiorly on the femur at the greater trochanter, blending with the fibers of the ischiofemoral ligament [7]. It reinforces the hip joint capsule posteriorly, where its fibers create a sling around the femoral neck and comprise the distal free border of the joint capsule [7, 8].
The labrum and capsule with its associated ligaments and zona orbicularis provide stability to the hip joint during distraction [8]. The proximal to middle portions of the capsule and the zona orbicularis seem to have a particularly important role in resisting distractive forces [8]. Thickness of the joint capsule has also been linked to joint stability. The role of the joint capsule as a stabilizer is an especially important consideration in total hip arthroplasty (THA), as research has suggested that compromise of the capsule may be an important, if not the primary, cause of dislocation after arthroplasty surgery [9]. Because all of the ligaments are taught in hip extension, hip extension is a very stable, “closed packed” position of the joint.
The ligamentum teres was once considered a vestigial structure with no role in the stabilization or biomechanics of the hip joint; however, it is now suggested that this ligament is more than an embryonic remnant and may contribute to hip joint mechanics and pathology [10, 11]. The ligament teres arises from the transverse acetabular ligament as well as the ischial and pubic aspects of the acetabulum [11]. Its insertion site is into the fovea capitis of the femur which is a round area on the head of the femur devoid of articular cartilage. Histologically, the ligamentum teres is composed of well-organized bundles of type I, III, and IV collagen fibers [11]. It is invested by its own synovial membrane [10, 11]. An anterior branch of the posterior division of the obturator artery courses through the ligamentum teres, vascularizing it, and variable branches of this vessel extend into the femoral head. In some individuals these branches may contribute some, but not all, of the vascular support to the femoral head itself [10, 11]. It has been suggested that this ligament may function as an intrinsic stabilizer of the hip joint and may resist subluxation of the hip joint, but this remains to be definitively proven [10, 11].
The acetabular labrum , also called the cotyloid ligament, is a fibrocartilagenous structure attached both along the perimeter of the bony acetabulum and to its articular surface via connections to the articular cartilage lining the acetabulum (Fig. 5). The labrum also has attachments to the transverse acetabular ligament anteriorly and posteriorly, and together these structures complete the socket of the hip joint [12, 13]. The labrum is primarily composed of type I collagen [12]; however, the attachment of these fibers to the acetabulum differs anteriorly and posteriorly in the joint. The anterior fibers are reported to attach parallel to the bony edge of the acetabulum making them susceptible to shear forces, while the posterior fibers attach perpendicular to the bony edge increasing their ability to resist shear stresses [13]. The labrum is separated from the joint capsule by the capsular recess [13]. The labrum appears horseshoe-shaped when viewed en face; however, in cross section, the labrum appears triangular in shape [12] .
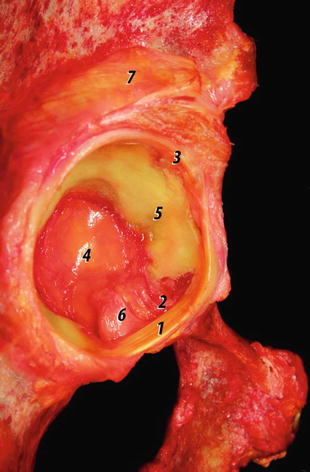
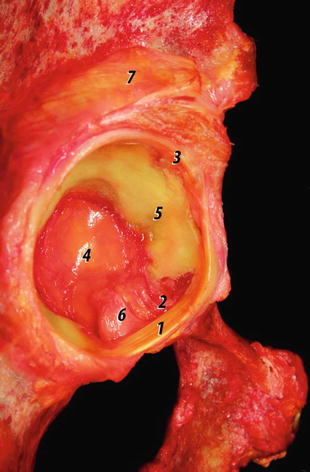
Fig. 5
Posterolateral view of a right acetabulum. Note the origin and attachment of the transverse acetabular ligament. (1) Transverse acetabular ligament. (2) Acetabular notch. (3) Acetabular labrum. (4) Acetabular fossa. (5) Anterior lunate cartilage. (6) Ligamentum teres (resected). (7) Reflected tendon of the rectus femoris muscle (http://www.springerimages.com/Images/MedicineAndPublicHealth/1-10.1007_978-1-4419-7925-4_7-7)
Muscular Anatomy
Muscles acting on the hip joint include muscles of the gluteal region (Fig. 6) as well as the muscles of the anterior, medial, and posterior compartments of the thigh. This section will review the attachment sites and actions of these regional groups of muscles with particular attention to those with the greatest clinical significance.


Fig. 6
Cadaveric dissection of the musculature of the gluteal region with the gluteus maximus reflected. The gluteus medius, piriformis, superior gemellus, tendon of the obturator internus, inferior gemellus, and quadratus femoris are visible in the dissection field. The sciatic nerve is visualized coursing inferior to the piriformis muscle (Photo reproduced with permission from Daniel Wasserman)
In the gluteal region muscles are classically divided into superficial and deep groups. The superficial group includes the gluteus maximus, gluteus medius, gluteus minimus, and the tensor fascia lata. Of this group, the gluteus maximus is the most superficial muscle with origins from the fascia of the gluteus medius, the ilium, the thoracolumbar fascia between the lower border of the posterior superior iliac spine and a point just lateral to the spinous process of the third sacral vertebrae, the aponeurosis of the erector spinae muscles, the sacrum, the coccyx, and the sacrotuberous ligament [14]. The insertion site for the majority of this muscle is on the iliotibial band at its aponeurotic origin on the greater trochanter of the femur; however, the inferior third of the muscular fascicles insert onto the gluteal tuberosity of the femur [14]. This muscle receives innervation from the inferior gluteal nerve, which arises from the ventral rami of the fifth lumbar as well as the first and second sacral spinal nerves. The inferior gluteal nerve emerges from the pelvis via the greater sciatic foramen inferior to the piriformis muscle. Attachments of the gluteus maximus to the thoracolumbar fascia and the aponeurosis of the erector spinae are not uniformly recognized in all anatomy texts. Recent literature suggests that these attachments and the large area of the gluteus maximus which crosses posterior to the sacroiliac joint support a role for this muscle as a stabilizer of the sacroiliac joint via generation of compressive forces on this joint and may also assist in load transfer between the lower limbs and trunk [14]. These functions are in addition to this muscle’s more classically described function of hip joint extension when the thigh is in a flexed position, such as in rising from a seated position. The gluteus maximus is also activated with forceful lateral rotation and abduction of the thigh. There is uniform agreement that the gluteus medius originates from the ilium between the anterior and posterior gluteal lines, while the iliac crest and the gluteal aponeurosis are also cited by some as proximal sites of attachment by some [15]. The gluteal minimus is classically described as arising from the external surface of the ilium between the anterior and inferior gluteal lines [15]. The gluteus minimus was extensively described in a cadaveric dissection study as proximally arising from the external ilium just anterior to the anterior superior iliac spine and then running parallel to the iliac crest up to the iliac tubercle [16]. Along the anterior gluteal line, the gluteus minimus is reported to extend to the greater sciatic notch and to have a proximal attachment to cover the posterior superior acetabulum extending to the anterior inferior iliac spine [15]. It is agreed upon that the gluteus medius and minimus insert onto the greater trochanter of the femur, with the medius being most often reported as inserting onto the lateral aspect of the greater trochanter and the minimus onto its anterior surface [15]. It has been suggested that the gluteus minimus has an insertion into the hip joint capsule [16]. The final muscle of the superficial gluteal group, the tensor fascia lata, is commonly described as originating from the anterior lateral portion of the iliac crest and the lateral aspect of the anterior superior iliac spine. It is distally described as attaching into the fascia lata. There are differing descriptions as to how this distal attachment occurs, specifically if the tendon of the tensor muscle inserts immediately into the iliotibial band just beneath its muscular belly or if these fibers themselves continue inferiorly to insert into the Gerdy’s tubercle at the lateral aspect of the tibia and the patellar retinaculum [15]. Innervation to the gluteus medius and minimus and tensor fascia lata is via the superior gluteal nerve, arising from ventral rami of the fourth and fifth lumbar and first sacral spinal nerves. The superior gluteal nerve emerges from the pelvis via the greater sciatic foramen in a position superior to the piriformis muscle. Together, the gluteus medius and minimus and the tensor fascia lata serve a primary function as abductors of the thigh. Of most clinical relevance is their function in closed chain during gait to stabilize the pelvis and prevent pelvic drop away from the stance limb as the contralateral limb swings through for limb advancement. In a position of hip flexion, the gluteus medius and minimus also function as medial rotators of the thigh. While classically less emphasized than the other gluteal muscles, results of cadaveric dissection suggest a potentially important function of the gluteus minimus, given its attachment to the articular capsule. It is suggested that the gluteus minimus may be to stabilize the head of the femur in the acetabulum by tightening the capsule and applying pressure on the femoral head [16]. Recent detailed study of the gluteal muscles suggests that both the gluteus medius and minimus, but not the tensor fascia lata, can be subdivided into distinct compartments based on fascicular organization within each muscle as well as the patterns of innervations via distinct branches of the superior gluteal nerve to these compartments [17]. Clinical relevance to this compartmental organization has been suggested, as rehabilitation of these gluteal muscles often utilizes exercises which target specifically the anterior or posterior aspects of the muscles [17].
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








