Hip
GENERAL
More than one-third of hip problems in adults have their origin during growth.
Development
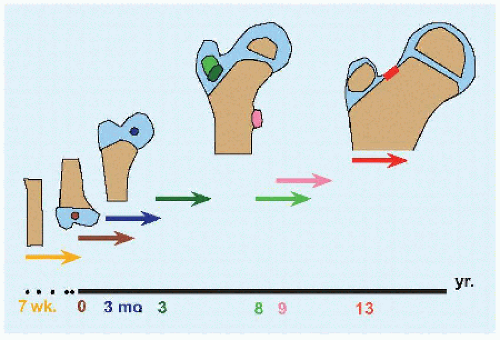
The distal femur is the only epiphysis consistently present at birth. The proximal epiphysis of the femur appears by the 2nd month in girls (2 to 6 months) and the 4th month in boys (4 to 8 months). The apophysis of trochanter major appears by the 3rd year, while that of trochanter minor appears by the 9th year. The proximal femur develops from a cartilage model in continuity from head to trochanter major until separation at the neck by the 13th year [A]. The acetabulum grows in depth and width from the triradiate cartilage and by apposition from the edge [B]. A secondary ossification center at the edge of the acetabulum appears in the early second decade, known as os acetabuli. The trochanter major enlarges by physial growth up to 8 years of age, after which growth is appositional.
Understanding growth of the hip elucidates disease and injury.
Röntgenogramme for hip dysplasia becomes more reliable after appearance of the proximal epiphysis of the femur.
Disease of the proximal femur epiphysis, such as Legg-Calvé-Perthes disease, affects the height and shape of the head, as well as the length of the neck.
Injury to the cartilage between the head and trochanter major, as in antegrade nailing or curettage of lesion, results in growth disturbance of the neck of the femur [B].
Fracture or injury of triradiate cartilage may result in premature closure and acetabular dysplasia.
Antegrade nailing for femur fracture is safe through trochanter major after 8 years of age. A case of a 10-year-old boy was included in Küntscher’s original report on the technique.
Os acetabuli is separated from the remainder of the acetabulum by horizontal or mildly oblique physial cartilage; by contrast, a vertical orientation is seen with femoroacetabular impingement.
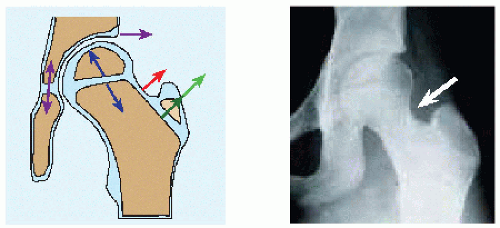
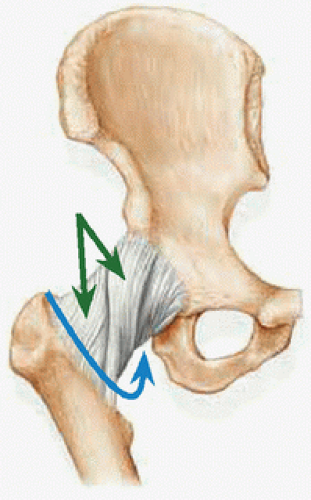
Evolutionarily, the forelimbs rotate laterally and the hindlimbs rotate medially. This results in medial twisting of the hip joint capsular fibers [C]. The universal response of a joint to injury or disease is effusion. The first and most consistently lost motion of a diseased hip is medial rotation: lateral rotation of the hip orients the capsular fibers parallel, thereby increasing volume of the hip joint to reduce pressure and stretch on pain fibers in the capsule.
Vascularity
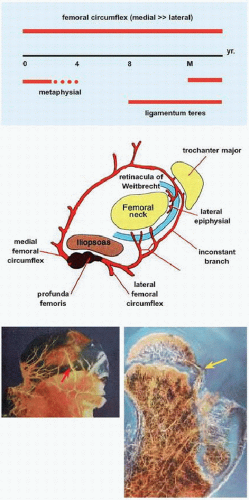
In addition to growth disturbance, the immature proximal femur is susceptible to vascular injury. The head of the femur is perfused from three sources during childhood [D].
In the neonatal period, metaphysial vessels may traverse the physis to supply the head of the femur; after 4 years of age, the physis becomes impervious.
Between 4 and 8 years of age, the head of the femur is dependent upon a single source: the circumflex vessels “travel around” the neck of the femur and are divided into medial and lateral based upon their direction of origin from the profunda femoris artery. The medial circumflex provides >80% of the blood supply to the head of the femur and enters the hip joint posterior to travel in the retinacula of Weitbrecht as the lateral epiphysial vessels. The lateral circumflex travels anterior and supplies the trochanter major in addition to the head of the femur.
After 7 years of age, the artery of ligamentum teres reaches the epiphysis from the obturator artery.
After physial closure, the metaphysial blood supply returns.
Pathoanatomy
Select principles are essential to understanding hip deformity.
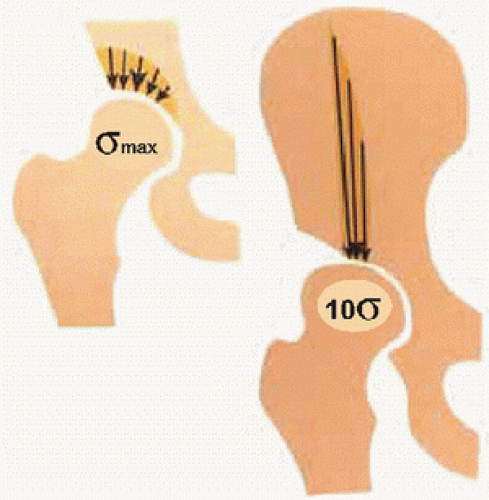
Cartilage Compression is good; shear is bad. Correct bone alignment to move oblique (shear) weight-bearing joint surface to horizontal (compression).
Acetabulum [E,F] The anterior wall overlaps the posterior wall approximately 50%. Margins of both walls meet at the lateral limit. In retroversion of the acetabulum, there is increasing overlap of the anterior wall until its margin overshadows that of the posterior wall to produce a crossover sign. The sourcil (named in French after its resemblance to an “eyebrow”) represents the principal weight-bearing surface: osteotomy of the pelvis aims to place this horizontal. Pressure = Force/Area. The acetabulum should cover enough of the head of the femur to avoid abnormal stress concentration, in particular at the edge. The “teardrop” represents medial wall of acetabulum: widening suggests insufficient medial force from a subluxated head of femur, and displacement beyond the ilioischial line (of Köhler) is defined as coxa profunda: “deep hip.”
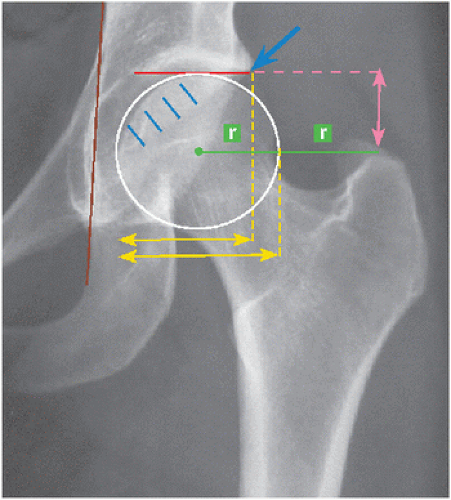
Proximal femur [E,F] The top of the trochanter major is at the level of the center of the head of the femur. If the top is above this level, there is varus deformity; if the top is below this level, there is valgus deformity. The articulotrochanteric distance is measured from the top of the articular surface of the head of the femur to the top of trochanter major: it is increased in valgus, reduced in varus, and negative in severe varus. This assessment of varus and valgus is independent of rotation, which may distort measurement of neck-shaft angle. Tip of trochanter major is 2 radii lateral (offset) to the center of the head of the femur. “Protrusion” of the head of the femur beyond the ilioischial line is defined as protrusio acetabuli.
Femoral anteversion and neck-shaft angle vary in utero, are maximum at 2 years of age, and then decline until maturity [G]. The head is offset from the neck in coronal and sagittal planes [H]. The head-neck
junction subtends an angle (designated α) with the longitudinal axis of the neck in both planes. Lateral offset is reduced and α angle is increased in femoroacetabular impingement and slipped capital femoral epiphysis. The latter also is characterized by reduction in coronal plane offset, simulating varus deformity in the anteroposterior projection.
junction subtends an angle (designated α) with the longitudinal axis of the neck in both planes. Lateral offset is reduced and α angle is increased in femoroacetabular impingement and slipped capital femoral epiphysis. The latter also is characterized by reduction in coronal plane offset, simulating varus deformity in the anteroposterior projection.
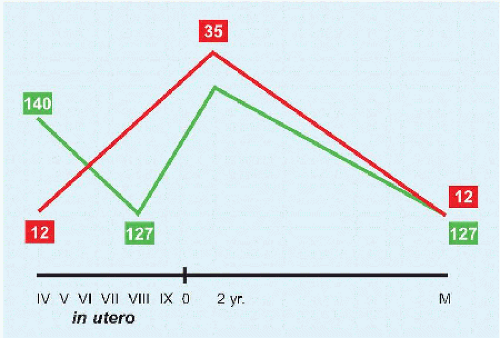 G Angulation of the proximal femur Mean values of neck-shaft angle (green) and neck anteversion (red) in degrees. Fœtal age in Roman numerals. M: maturity. |
The head of the femur is spherical, which allows motion in all dimensions. More important than sphericity is congruity: while the latter may concede limitation in motion, matching articular surfaces prevent stress concentration. Incongruity despite cosphericity occurs in subluxation, leading to edge loading.
Distinguishing Features
The hip is a bone-dependent joint, in contrast with the knee (ligament dependent) and the shoulder (muscle dependent). It is enarthrodial, consisting of a “ball in socket” that allows motion in all directions, like the shoulder and in contrast with the knee, which is ginglymoid (“hinge-like”), and the symphysis pubica or sacroiliac joints, which as syndesmoses absorb motion more than they allow it. The hip, like the shoulder, may be distinguished by its axial location, which under cover of multiple layers of thick muscle makes it obscure to direct observation and palpation. It also may be distinguished by the precariousness of its blood supply, raising the specter of osteonecrosis in several of its disorders and management. Outside of trauma, the hip in a
child demands more attention of the surgeon than any other joint. Like the glenoid cavity of the shoulder, the acetabulum is rimmed by a labrum. Like the cruciate ligaments of the knee, the hip joint is traversed by the ligamentum teres (also known as ligamentum capitis femoris), connecting the fovea centralis of the head of the femur with the fossa of the acetabulum.
child demands more attention of the surgeon than any other joint. Like the glenoid cavity of the shoulder, the acetabulum is rimmed by a labrum. Like the cruciate ligaments of the knee, the hip joint is traversed by the ligamentum teres (also known as ligamentum capitis femoris), connecting the fovea centralis of the head of the femur with the fossa of the acetabulum.
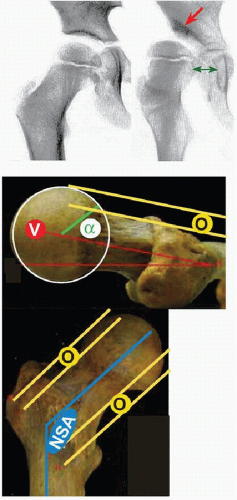 H Architecture of the proximal femur. V: version of the neck (degrees) α: angle of head-neck junction O: offset of the head and neck (mm) NSA: neck-shaft angle |
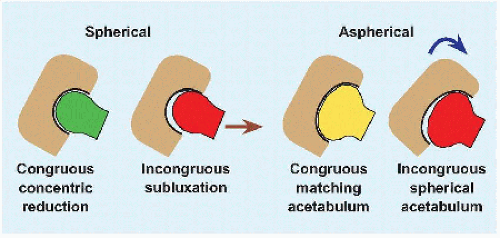 I Congruity versus sphericity Incongruity (red) leads to stress concentration, which may result from subluxation in hip dysplasia (brown) or rotational osteotomy (blue). |
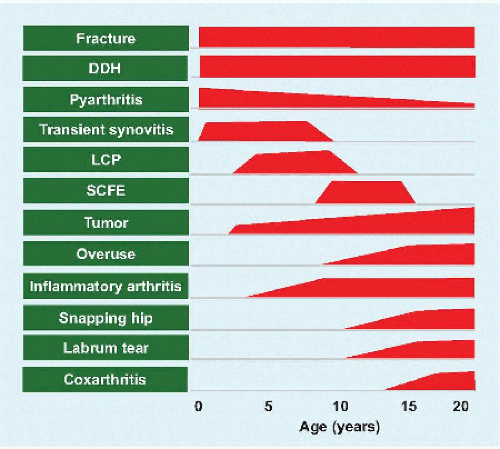 A Conditions affecting the hip by age DDH: developmental dysplasia of the hip. LCP: Legg-Calvé-Perthes. SCFE: slipped capital femoral epiphysis. |
EVALUATION
History
Is there a family history? Developmental dysplasia of the hip can be familial. Has there been an alteration of gait? The waddle of a dislocated hip may seem attractive in a young girl. Does the hip make noise or catch? Crepitus may be a sign of labrum tear.
Age Age is a universal discriminator of disease [A].
Onset In the acute presentation, it is imperative to rule out fracture, which occurs after an antecedent event, pyarthritis, and slipped capital femoral epiphysis, which carries urgency due to the fragile vascularity of the hip. Other conditions, such as Legg-Calvé-Perthes disease, tend to have a more insidious onset and chronic course.
Physical Examination
Observation Does the child appear ill? Distress and fear are signs of infection or trauma. Are there constitutional or other system symptoms or signs? Hyperactivity and small for age have been associated with Legg-Calvé-Perthes disease. Overweight is typical of slipped capital femoral epiphysis. Rash is associated with inflammatory and autoimmune conditions that may affect the joints.
Pain Is there pain, and where? The law of Hilton (John Hilton, surgeon at Guy’s Hospital London, 1860) states that “a nerve which innervates a muscle that acts on a joint will innervate that joint and the skin overlying the muscle’s insertion.” While groin pain may have an intrapelvic origin, such as inguinal hernia, the groin also is the locus of hip pain. In addition, femoral and obturator nerves supply muscles inserting about the anteromedial knee, where hip pain manifests in isolation in up to 15% of cases. Buttock pain may be from the back or from hip abductor muscle fatigue. The latter also may manifest as lateral pain, which in turn may be produced by contracture of the iliotibial tract.
Pain that awakens from sleep is concerning, in particular for osteoid osteoma. Tenderness may be seen in apophysitis or apophysial injury. Be careful of a “groin pull” in the peripubescent or associated with lateral rotation of the lower limb.
Gait Is there a limp, and if so what type? Reduced stance phase is seen in painful conditions such as trauma. Pain without an alteration in gait is less concerning. Abductor lurch (of Trendelenburg) results from weakness of pericoxal muscles [B]. Out-toeing gait is pathognomonic of slipped capital femoral epiphysis in a peripubescent child.
Palpation The hip joint is deep, and as such, points of tenderness are less revealing than more exposed joints such as the knee. Apophysis are accessible, including at iliac spines, tuberosity of ischium, and trochanter major in traumatic separation or irritation (overuse). Crepitus may be elicited from the hip joint, for example, labrum, or from pericoxal tissues, for example, a snapping psoa muscle in the groin or an iliotibial tract grating or “jumping” (coxa saltans) across trochanter major.
Motion
PSEUDOPARALYSIS Severity of disease or early age of onset may cause the child to quit the limb, out of pain and fear.
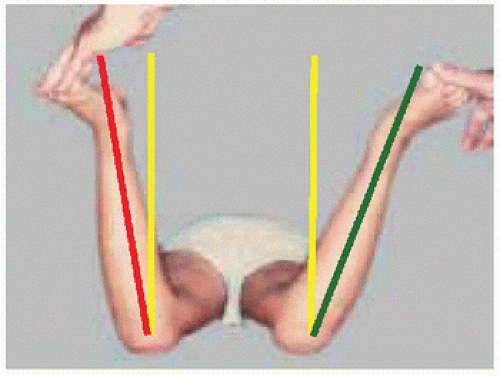
HIP ROTATION Medial rotation is the first and most characteristic motion lost in hip disease; this is followed by flexed posture or contracture. The prone position has three principal advantages [C]. It stresses a hip held in flexion. Comparison may be made as both hips may be moved simultaneously. The knee may be decoupled from the hip: the former may be moved without obligate motion of the latter, as occurs supine. Supine position allows assessment of rotation in the flexed position, which may be altered as the neck of the femur impacts acetabulum, as in slipped capital femoral epiphysis deformity.
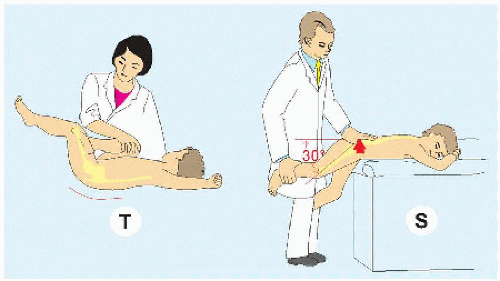
FLEXION In addition to losing medial rotation, the painful or diseased hip is held in flexion. This is exposed automatically when evaluating motion in the prone position. In the supine position, a contracture may be detected by the Thomas or the prone extension test [D]. Pain with flexion beyond 90 degrees, exacerbated by adduction and medial rotation, suggests impingement. By contrast, the same pain with the same manœuvre but with normal or increased motion is seen in hip dysplasia, due to damage of a deficient anterior wall of acetabulum.
EXTENSION Perform supine with pelvis at edge of table. The patient flexes contralateral hip while the examiner extends the hip and limb beyond table. Anterior deficiency of acetabulum, as in hip dysplasia, produces apprehension. Painful extension also may be seen in psoa abscess.
ABDUCTION-ADDUCTION Assess with fingers on anterior superior iliac spines as reference points, so that tilting of the pelvis does not mask contracture. Varus deformity of the hip, or growth disturbance of the head and neck of the femur, will lead to abutment of trochanter major against the ilium, thereby limiting abduction. Reduced adduction due to iliotibial tract contracture is assessed by Ober test: patient lateral; the examiner hand stabilizes the pelvis to keep it vertical; contralateral hip held by the patient in flexed position; and examined hip flexed, then abducted, and then extended while the examiner holds foot only. Contracture prevents the examined limb from adducting: the knee will remain suspended in abduction beyond midline.
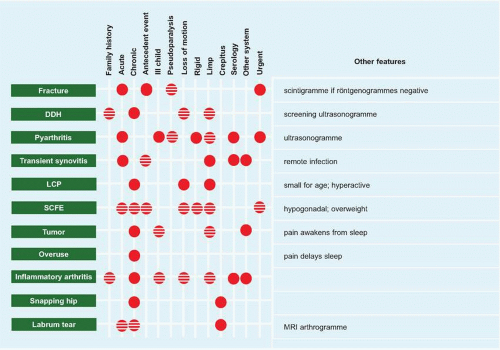 E Diagnosis of hip disease Characteristic (solid) and possible features (striped). DDH: developmental dysplasia of the hip. LCP: Legg-Calvé-Perthes. SCFE: slipped capital femoral epiphysis. |
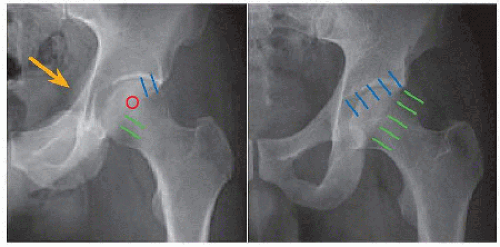
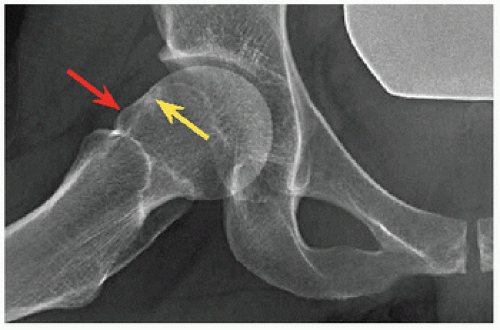 B Lateral of proximal femur Note bump (red) on the neck with adjacent cyst (yellow), due to femoroacetabular impingement. |
Imaging
Röntgenogrammes These are the foundation of imaging for the hip.
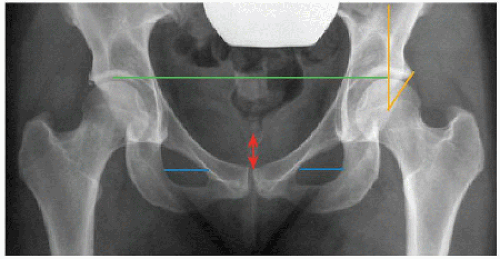
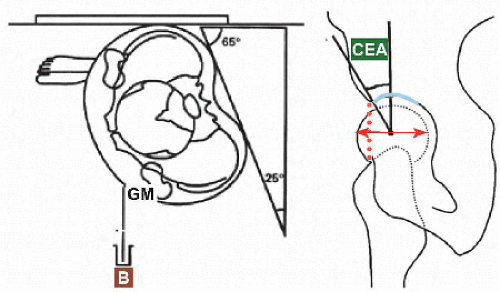
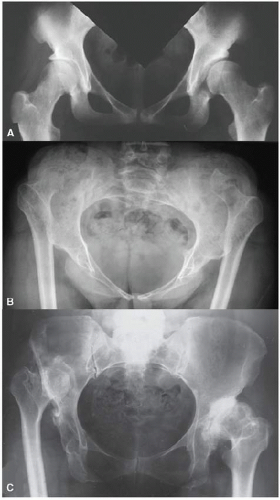
In the anteroposterior projection of the pelvis, symmetry of the transverse diameters of the obturated foramina ensures neutral [A]. In the standing position, tip of coccyx to symphysis pubica distance 1 to 3 cm ensures correct pelvic tilt. The top of the femoral heads may be used to determine limb lengths, assuming a standing position with knees straight. Medial rotation of the lower limbs neutralizes anteversion of the femora for true coronal relationship with acetabula. The angle between a vertical through the center of the head of the femur and a line drawn from the center to the edge of the articular margin of acetabulum is a measure of coverage. The normal range is 25 degrees to 45 degrees: less represents insufficient coverage, as in developmental dysplasia of the hip, while more represents overcoverage, as in pincer impingement or protrusio acetabuli.
Lateral projection of the proximal femora may be obtained by supine abduction with external rotation (“frog-leg”), placing the feet together with the knees flexed to 90 degrees [B]. In the painful or unstable hip, an easier and safer view is taken supine with the contralateral hip flexed 90 degrees and the x-ray beam directed “cross-table” at 45 degrees to the symptomatic limb. Soft tissue may obscure details. In the operating room, a lateral projection of the proximal femur may be obtained by flexing the hip to 45 degrees while preserving neutral rotation, and rotating the image intensifier 45 degrees away (modified Dunn).
Supine abduction with medial rotation of the femora (von Rosen) assesses center of rotation of the head of the femur compared with acetabulum and simulates redirectional osteotomy of the acetabulum.
The faux profil (“false profile”) provides a true lateral of the acetabulum, based upon its version [C]. The patient stands with affected hip against the film, pelvis rotated 65 degrees toward affected side, and affected foot parallel to film. The angle between a vertical through the center of the head of the femur and a line drawn from the center to the edge of the articular margin of acetabulum is a measure of anterior coverage. Less than 20 degrees is abnormal.
Version of acetabulum [D]. Normal version presents a symmetric opening of the cup to the front of the hip, seen on anteroposterior projection as an anterior wall that covers half of the posterior wall, which it meets at the lateral margin of acetabulum. In retroversion of the acetabulum, the anterior wall advances on the posterior wall, progressively crossing it from lateral to medial. Retroversion rotates the ischial spine anteriorward and medialward into profile. Note that projection of the walls of the acetabulum is influenced by pelvic tilt, which must be correct to correctly assess version of acetabulum and crossover.
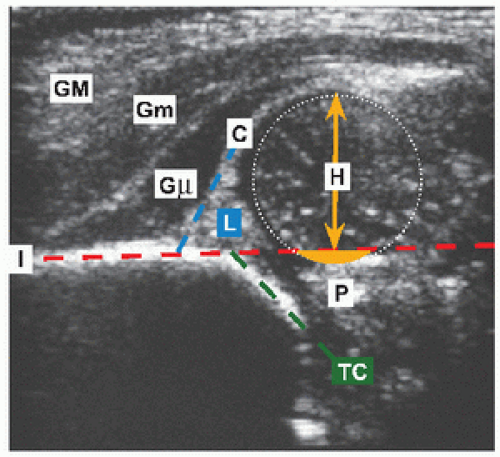
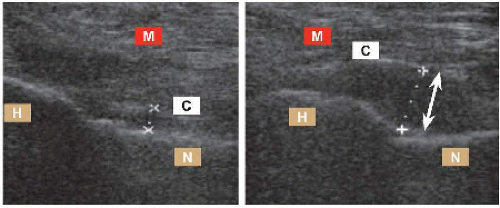 E Ultrasonography for hip effusion The joint capsule is elevated (white) off the femur by fluid. H: head of the femur. N: neck of the femur. C: capsule. M: muscle. |
Ultrasonography This is the standard for screening and evaluation of hip dysplasia from neonatal period to 4 to 6 months. Ultrasonography is useful for evaluating the hip for effusion [E]. It is quantitative and qualitative, demonstrating volume of fluid and type (e.g., clear vs. turbid). It is harmless, is practical, and may be performed with the child awake, by contrast with MRI, which provides more detail at the expense of complexity and sedation. Other applications include assessment of severity of slipped capital femoral epiphysis, of head size and containment in Legg-Calvé-Perthes disease, and of neck continuity in coxa vara. This imaging technique is underutilized, despite the fact that it has the distinct advantage of being practicable by an orthopædic surgeon in office.
Scintigraphy This is a physiologic imaging modality, providing a measure of bone turnover and perfusion. After excluding pyarthritis by an ultrasonogramme showing no effusion of the hip, a scintigramme evaluates the lower limb for osteomyelitis as a cause of limp. Inflammatory conditions may be localized, such as osteoid osteoma of the proximal femur. Hypoperfusion may be detected, such as of a slipped capital femoral epiphysis with an acute or unstable or severe presentation, or of the proximal epiphysis of the femur during the initial ischæmic stage of Legg-Calvé-Perthes disease [F]. Hyperperfusion of the proximal physis of the femur may be an alert to a preslip state.
Arthrography Arthrogramme confirms articular penetration, as in arthrocentesis in infection or for diagnostic injection when a locus of pain is obscure. The technique aids operative evaluation of dislocation and reduction in developmental dysplasia of the hip. It provides further static definition of the deformed head of the femur in Legg-Calvé-Perthes disease [G] and permits dynamic assessment of hip motion. Arthrography enhances magnetic resonance imaging.
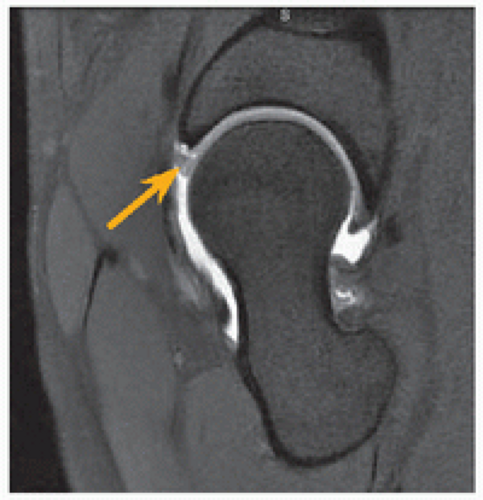
Magnetic resonance imaging This modality provides greatest detail, in particular of intra-articular structures such as labrum in developmental dysplasia of the hip [H], epiphysis with altered perfusion, physis in slipped capital femoral epiphysis, a mobile body after trauma, or effusion as a first or only sign of disease. Rapid sequence protocol assesses location of the head of the femur after reduction of a dislocated hip, without X-radiation. Balance this with less availability, less agency for the surgeon, increased cost, and the fact that in the first decade sedation may be necessary to avoid motion artifact. Gadolinium may be injected for arthrography or per venam to measure proteoglycan content of cartilage.
Computerized tomography CT gives the most accurate depiction of osseous architecture, in particular as part of preparation for osteotomy of the pelvis or femur in the setting of complex deformity. It is less distorted than MRI by metal, as in postoperative evaluation of implant placement or healing of osteotomy [I]. Rapid sequence protocol assesses location of the head of the femur after reduction of a dislocated hip, but with radiation exposure in contrast with MRI.
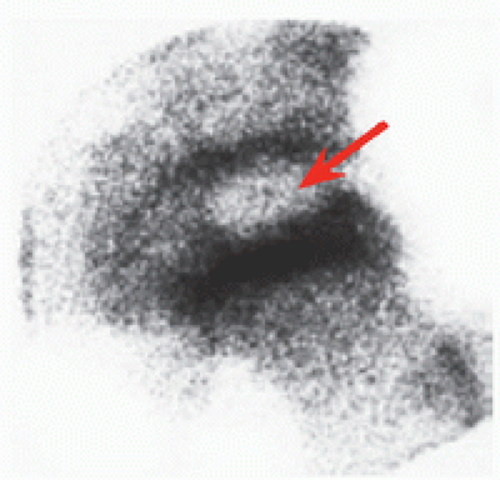 F Scintigraphy of the hip Focal lateral and anterior reduced uptake in the epiphysis (red) indicates ischæmic stage at presentation of Legg-Calvé-Perthes disease. |
 G Arthrography of the hip The articular surface is outlined showing flattening of the epiphysis (green) by the lateral acetabulum (blue) in Legg-Calvé-Perthes disease. |
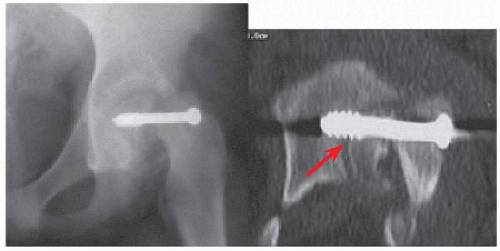 I CT to evaluate implant placement In this severe slipped capital femoral epiphysis, uncertainty about location of screw was resolved by CT, showing transarticular fixation (red). |
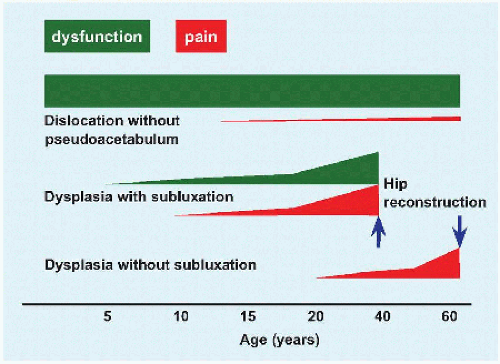
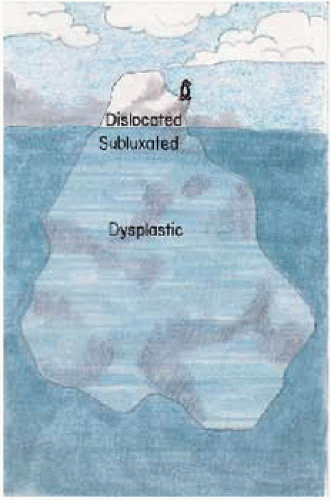 A Spectrum of hip dysplasia Dislocated hips are usually diagnosed during infancy, but hip dysplasia may not become evident until adult life, when it presents as degenerative coxarthritis. |
| ||||||||||||
DEVELOPMENTAL DYSPLASIA OF THE HIP
Dysplasia refers to “bad” (Greek δvζ) “formation” (Greek πλασσω) of the hip. The term developmental encompasses cases that are congenital, present “at birth,” and those developing after birth, in which the neonatal evaluation is normal.
Incidence
Hip laxity affects up to 1% of neonates, whereas clinically detectable DDH affects 0.1% of the Caucasian population. The true incidence remains unclear [A]. Physical examination and even screening ultrasonography will have a certain miss rate for several reasons, including operator error, single evaluation of a developing condition in a developing skeleton, and the use of indirect measures as proxies for final outcomes. As a result, DDH may underlie up to one-third of adult coxarthritis.
Cause
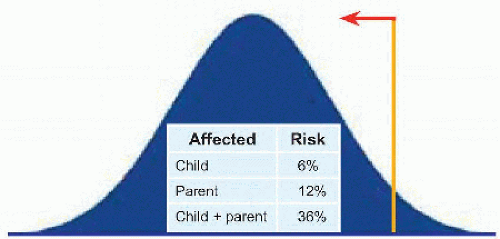
The causes of DDH may be divided into intrinsic or extrinsic. The former represents polygenic inheritance (‘problems of production’), in which a characteristic is controlled quantitatively by more than one gene (the quintessential example is height) [B]. The latter refers to ‘problems of packaging’, of which the most significant factor is breech, with oligohydramnios and primigravida uterus being relative factors [C]. Girls and the left hip are affected more. Incidence in Caucasians is 1%: it is five times more in Lappland and five times less in Africans.
Pathoanatomy
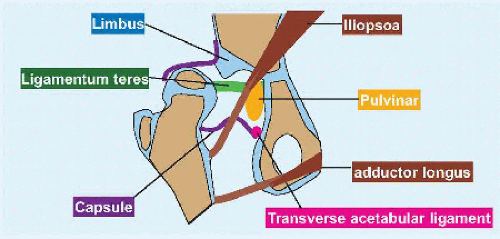
The acetabulum is shallow and maldirected. The proximal femur shows antetorsion and coxa valga. When either or both are sufficiently severe, the head of the femur will dislocate. Extra-articular obstacles to reduction include iliopsoa, which constricts capsule such that it will display an hourglass configuration with arthrography, and adductor longus [D]. Articular obstacles include labrum, which may be inverted and hypertrophied as the limbus, ligamentum teres, a thickened and tortuous ribbon, pulvinar, which expands (nature abhors a vacuum), and medial inferior capsule.
Evaluation
Physical examination This first is performed as part of neonatal screening, during subsequent routine evaluations, and as part of an orthopædic consultation. Take what the child will give: relax if there is resistance, and resume with no force when the child relaxes. Test for instability in the entire range of hip motion.
HIP CLICK This is normal. It refers to a fine short-duration feeling or sound that is a manifestation of laxity stressing the limits of motion. Differentiate from a “clunk,” which represents the deep perception of a shift as the head of the femur dislocates and relocates. The sensation of the hip being displaced over the acetabular margin.
CUTANEOUS CREASES Asymmetry may be seen in long-standing dislocation in older children, where significant contracture has had time to develop. Asymmetric and extra creases affect approximately 50% of normal infants.
HIP ABDUCTION Abduction of the hip <60 degrees is concerning for DDH [E].
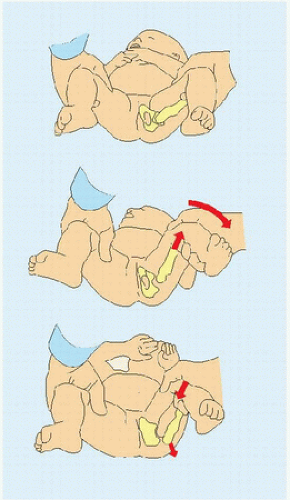
BARLOW SIGN Dislocation of a reduced hip [F]. With adduction of the hip, the head of the femur moves out over the rim of acetabulum. There is no need for posteriorward force: gravity will suffice. ORTOLANI SIGN Reduction of a dislocated hip [G]. With abduction and anterior translation applied to the trochanter major, the head of the femur moves into the acetabulum. Prolonged dislocation may result in sufficient contracture to resist this manœuvre, producing an “Ortolani negative” hip. The only sign may be limited abduction. The symmetry of bilateral presentation may obscure detection.
LOWER LIMB LENGTH DISCREPANCY The head of the femur, taking with it the rest of the limb, rests behind a dislocated hip, producing a lower limb length discrepancy [H].
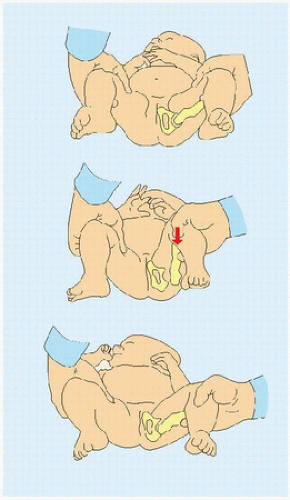 G Ortolani sign A dislocated hip is reduced by abduction with anterior translation applied to trochanter major, perceived as a “clunk.” |
LUMBAR LORDOSIS Dislocation in which the hips are displaced significantly craniad, and posteriorward is accompanied by anterior pelvic tilt and flexion contracture of the hips. The child compensates by hyperlordosis of the lumbar spine to maintain sagittal balance [I].
GAIT The dysplastic acetabulum, without or with subluxation, is silent in the first decade. Hip dislocation produces a Trendelenburg gait due to craniad displacement of trochanter major with shortening and thereby weakening of hip abductor muscles.
PACKAGING SIGNS As part of the extrinsic causation of DDH, other parts of the musculoskeletal system may manifest deformation, including plagiocephaly, torticollis, and metatarsus adductus. The natural history of these is benign, with spontaneous resolution without active treatment. A corollary is DDH as a packaging sign in association with congenital dislocation of the knee.
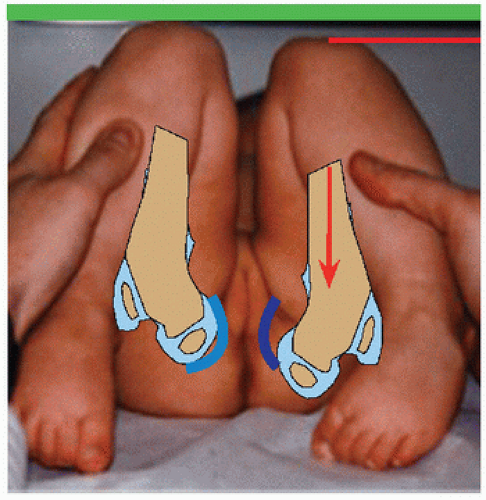 H Galeazzi or allis sign Posterior displacement of the head and rest of the femur produces a limb length discrepancy that is exposed as differential knee heights. |
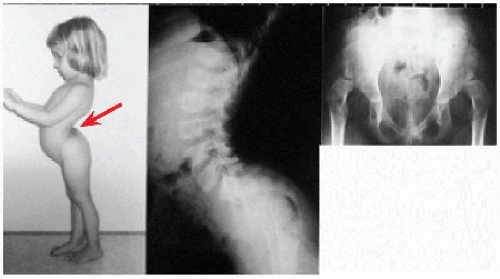 I Bilateral DDH Lumbar hyperlordosis (red) with protuberant abdomen in an older child with bilateral hip dislocation. |
 C Röntgenography of DDH Left proximal ossific nucleus (red) is dislocated into lower lateral quadrant. |
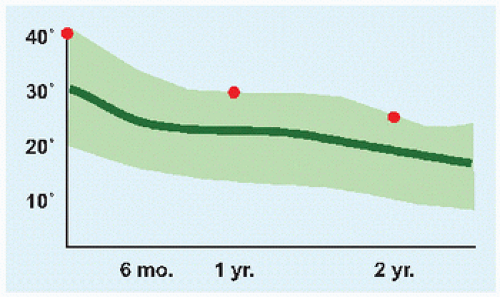 D Acetabular index by age This is measured in degrees. Light green bounds two standard deviations from the mean (dark green). |
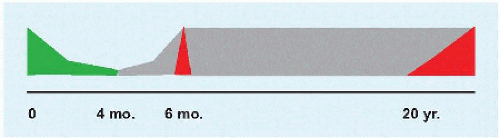
Imaging This varies according to age [A]. It is performed as part of neonatal screening, during subsequent routine evaluations, and as part of an orthopædic consultation. Take what the child will give: relax if there is resistance, and resume with no force when the child relaxes. Test for instability in the entire range of hip motion.
ULTRASONOGRAPHY Indications include the following:
Screening tool. This is a practice in continental Europe.
Infant at risk. This is the practice in the United States, in order to limit the false-positive rate. The definition of at risk varies: it may be restricted to breech girl, or it may include family history.
Unclear physical examination, for example, if a fixed dislocation is suspected (Ortolani negative hip), where a clunk would be absent.
To evaluate the success of brace treatment of the dysplastic hip.
Ultrasonography is not indicated when the physical examination detects a dysplastic hip, because imaging will not change management. There are two forms.
Static [B]. This defines architecture. α (for “acetabulum”) angle measures depth of acetabulum. This is mirrored by the β (next letter in the alphabet) angle, which measures deflection of the labrum by the head of the femur. d:D ratio measures coverage of the head of the femur by acetabulum.
Dynamic. This evaluates stability and is an aid to the physical examination.
Normal α angle is >60 degrees. Most hips in range 43 degrees to 60 degrees “heal up” (Graf) without treatment. Normal d:D ratio is >0.5. Ratio <0.2 suggests failure of Pavlik harness. The static method describes architecture of the hip. The dynamic method may be considered the imaging extension of the physical examination: this, along with the fact that it is most operator dependent and is best assessed live (missed unless the surgeon is operator), makes it less useful.
RÖNTGENOGRAPHY This is the standard after 3 months of age, when the proximal femoral ossific nucleus is visible [C].
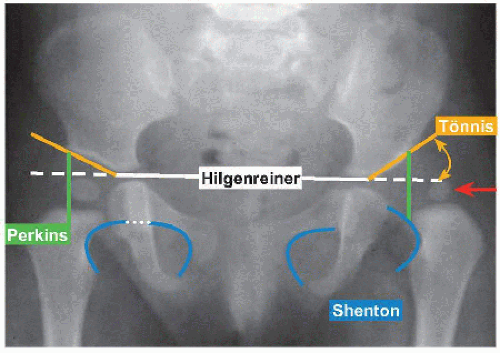
Hilgenreiner line is the horizontal reference for the pelvis.
Perkins line is a vertical mark of the lateral edge of acetabulum. In dislocation, the proximal femoral ossific nucleus lies lateral to this, with migration above Hilgenreiner line with increasing severity. If the nucleus has not ossified, medial corner of proximal metaphysis is medial to Perkins line in the normal hip.
Shenton line is drawn along proximal metaphysis of the femur and margin of obturated foramen. Projected discontinuity between these two lines can highlight subluxation when dislocation is not apparent (e.g., when nucleus has not ossified).
Acetabular index (of Tönnis) measures inclination of sourcil, a theme that arches over DDH regardless of age.
Normative data for acetabular index aid assessment of the dysplastic acetabulum without subluxation or dislocation [D]. The following are guidelines for abnormal (precision is evasive because measurement error is up to 10 degrees, due to observer, patient position, and projection):
Index above 40 degrees in the first year of life.
Index above 30 degrees in the second year of life.
Index above 24 degrees by 24 months of age.
COMPUTERIZED AXIAL TOMOGRAPHY This is reserved for complex deformity, and when metal is present that would distort MRI. Be judicious in requesting this modality, due to radiation exposure early in life that is cumulative.
MAGNETIC RESONANCE IMAGING This has a bimodal application. It evaluates location of the head of the femur after closed or open reduction and immobilization of the infant hip, utilizing motion insensitive sequences that show sufficient detail despite sacrifice in resolution, avoiding need for anæsthesia. MRI has illuminated hip dysplasia in the teenager and young adult.
Labrum. This is invisible to röntgenography or CT. Arthrography with gadolinium may highlight degenerative changes, such as tear or cyst.
Impingement. This may be represented more accurately than by röntgenography, such as measurement of the α angle between the axis of the neck and a line drawn from center of the head to its junction with the neck in cam deformity of the proximal femur.
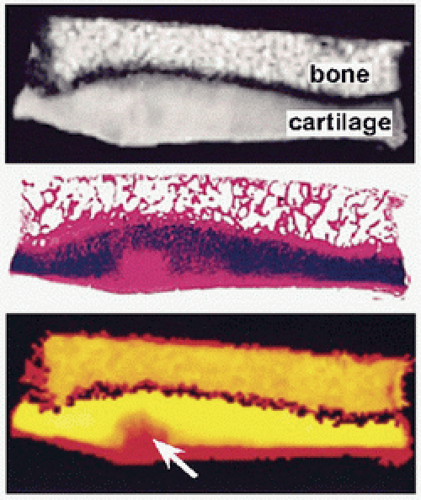
Cartilage. Delayed gadolinium enhancement MRI of cartilage [E] is a measure of the biochemical composition of cartilage and as such of its health and mechanical properties. This contrasts with other structural or morphologic imaging modalities. An exogenous agent that may be nephrotoxic, the need for an exercise protocol to aid delivery to cartilage, and delay have stimulated development of other modalities. In sodium scanning, MRI may be used to measure relaxation times of the cation, which mirrors glycosaminoglycan concentration. Chemical exchange saturation transfer, T1r, T2 mapping, and diffusion-weighted MRI measure signal arising from protons as a biomarker, in particular hydroxyl and amide protons of glycosaminglycans. Ultrasonography shows healthy cartilage as homogeneously hypoechogenic with a well-defined chondrosynovial boundary, characteristics that are lost in degenerative arthritis.
Natural History
Untreated DDH may have the following outcomes [F, G].
Acetabular dysplasia without subluxation. This presents in adulthood: cartilage degeneration results from stress concentration, according to the formula Pressure = Force/Area.
Acetabular dysplasia with subluxation. This presents in childhood. Lack of concentric reduction significantly reduces surface area of contact, concentrating contact pressure. This is exacerbated by micromotion that shears cartilage.
Acetabular dysplasia with dislocation. This in turn may be divided into without or with pseudoacetabulum. The former leads to functional disability produced by shortening and weakening of hip abductors, including Trendelenburg gait, fatigue pain, and restricted hip motion. The latter is associated with disabling pain due to osseous erosion between the head of the femur and ilium.
In one-third of patients treated for DDH (from bracing to operation), initial success will be followed by residual disease requiring secondary treatment. This is the rationale for long-term follow-up, through maturity. Treatment is mechanical and not more fundamental for a disease that has multiple causes, including genetic. Treatment aims to bring a dysplastic hip into the normative range and relies on it sua sponte to continue to grow appropriately once acetabulum and femur are correctly aligned. Such follow-up is akin to evaluation of height and weight at well checks by the pædiatrician: a child in the 50th percentile may fall off the charts with growth.
Management
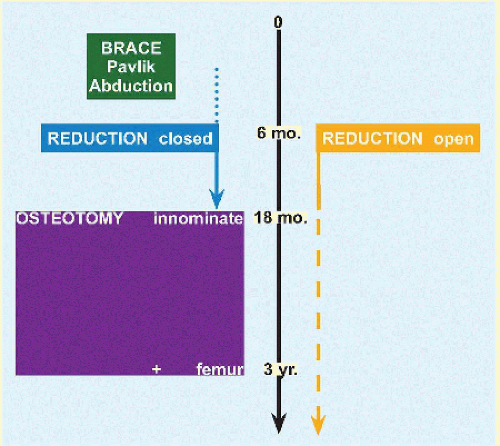
Management is based upon age [A].
Birth to 6 Months
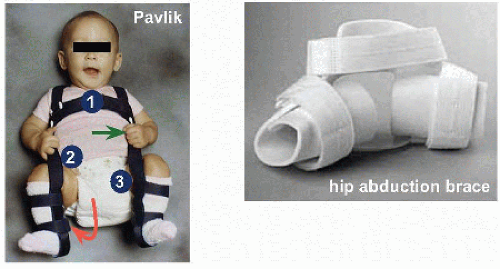
Pavlik harness This follows the principle of dynamic reduction: the child may move the limbs, which return to the favorable position for reduction and for stimulation of triradiate cartilage by the head of the femur when the child is still (including sleep). It is “simple, nondisturbing, and cheap” (Pavlik), hence its broad acceptance [B]. The straps, which are adjusted to maintain moderate force and to account for growth, are applied so that the hips are flexed to 90 degrees and abducted to 45 degrees while remaining readily adductable to neutral [B].
For the hip that rests located (Barlow or subluxatable), the harness is worn full time for 6 to 12 weeks. Treatment concludes once ultrasonographic or röntgenographic metrics have normalized, or if they have not done so by 12 weeks, at which point an alternative treatment is indicated.
For the Ortolani hip, the harness is applied and adjusted as necessary to convert to a Barlow hip over 3 weeks. Persistence of an Ortolani hip is a failure and an indication for alternative treatment. Restriction of the hip in a dislocated position may lead to deformation of the head of the femur and rim of acetabulum, worsening deformity. It also increases development of contracture of the hip. Both outcomes undermine subsequent treatment: the hip is more unstable, and contracture reduces likelihood of success with closed management.
There are other pitfalls of Pavlik harness. Do not overtighten the stirrups (e.g., to improve reduction of a very unstable hip): the posterior straps will abduct too much and risk the blood supply and osteonecrosis of the hip, while the anterior ones will hyperflex the hips and can cause a compressive femoral neurapraxia. While to the surgeon this is “simple” treatment, it may be confusing to parents: if you allow parents to remove the harness (e.g., to wash the child), spend time educating and follow-up with them to make sure they have reapplied the harness correctly.
The success rate of Pavlik harness is 80% to 90%. The Ortolani hip, bilateral disease, and increasing age reduce effectiveness. It is not indicated for teratic (e.g., arthrogryposis) or neuromuscular hip dysplasia.
Rigid immobilization This is indicated when Pavlik harness fails. For the persistent Ortolani hip, apply a hip abduction brace and follow Pavlik harness principles. For persistent abnormal imaging after 12 weeks of Pavlik harness treatment, apply a hip abduction brace full time until normalization of metrics. For a fixed dislocation (Ortolani negative hip), move to closed or open reduction.
6 to 18 Months
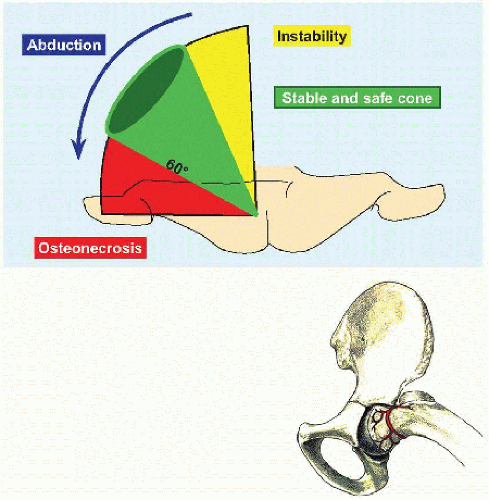
Closed reduction This is performed with general anæsthesia, in order to allow for arthrography and tenotomy of adductor longus. If there is contracture of the adductor longus origin, as determined by palpation with hip abduction, or if this necessitates excessive abduction to stabilize the hip, section the tendon to reduce the force of reduction. This may be performed through a stab incision after digital percutaneous isolation distal to the inguinal crease. Insert the blade over the lateral edge of the tendon and advance medialward away from the femoral vessels. A small incision and dissection avoids injury to the external pudendal artery (ramus of femoral artery), which accounts for at times considerable bleeding after percutaneous section. Excessive abduction risks compression of medial circumflex artery against the rim of acetabulum [C]. Excessive force of reduction adds direct compression of the head of the femur. If the hip reduces with a sufficiently stable and safe cone, apply a hip spica cast. If reduction is insecure, convert to an open reduction. If there is uncertainty, an arthrogramme may add clarity.
ARTHROGRAPHY Insert needle with trocar medial distal to inguinal crease raising the hand 30 degrees above the horizon directed at a point between anterior superior iliac spine and ipsilateral shoulder [A]. Alternatively, eliminate rotation of the hip and approach it laterally over trochanter major. Contact the neck of the femur (not the head and not the joint), relax force of insertion, and inject. Start with saline to confirm entry (so as not to obscure the joint by contrast reagent infiltrating the juxta-articular soft tissues), then just enough dilute contrast reagent to outline articular surfaces. Image intensifier assists. If there are significant obstacles to reduction, as evidenced by medial pooling of contrast due to lateral displacement of the head of the femur, open the hip. An inverted limbus may be a harbinger of persistent acetabular dysplasia despite successful reduction.
Open reduction The indication for this is articular obstacles to safe and stable closed reduction [B]. The hip may be approached anterior (Smith-Petersen) or medial [C]. The former is performed through an oblique incision in the “bikini line” (Salter). The latter, performed through a transverse incision centered on adductor longus origin one finger breadth distal to inguinal crease, may be divided according to relationship to the medial muscles of the hip (the adductor longus is sectioned). Ludloff described the “bloodless” approach between pectineus and adductor brevis. A more posterior medial approach travels between adductor brevis and adductor magnus. A more anterior medial approach follows the interval between pectineus and femoral vessels.
The anterior approach is familiar and utilitarian, including for osteotomy at an older age. Release of medial and posterior obstacles to reduction is blind to the medial femoral circumflex vessels, from which this approach is remote. A capsulorrhaphy is possible, which reduces redundancy of the dislocated hip capsule and adds a soft tissue restraint to redislocation. The medial is a more geographically direct approach to the obstacles to reduction. The medial femoral circumflex vessels are directly in its path, which lowers the risk of injury as these may be knowingly isolated and protected.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree