12
High Tibial Osteotomy: Distraction Osteogenesis
Surgical management of the malaligned arthritic knee in an active individual presents a challenge to the orthopaedic surgeon. Procedures aimed at regenerating articular cartilage in the arthritic knee are doomed to fail in the face of malalignment. Furthermore, unicompart mental or total knee replacement may not be appropriate in a patient who wishes to maintain a high level of athletic activity.
Since its description by Jackson in 19581 and Wardle in 1962,2 high tibial osteotomy (HTO) has become a widely accepted treatment for patients with moderately severe, primarily unicompartmental, varus degenerative arthritis of the knee.3 The strategy of the HTO is to unload the diseased medial compartment and realign the extremity so that the more normal lateral compartment bears a greater share of the load. Osteotomies can be performed using an opening or closing wedge technique. Additionally, medial opening wedge osteotomies can realign the leg acutely using a plate and bone graft or gradually using distraction osteogenesis. The closing wedge and acute opening wedge techniques are described elsewhere in this text. This chapter reviews the indications and technique for proximal tibial realignment using distraction osteogenesis.
Surgical Indications and Other Options
The treatment algorithm for the active patient with medial compartment arthritis and varus malalignment (Fig. 12-1) should include lower extremity strengthening, well-cushioned insoles, orthotics to promote a more valgus limb alignment, nutritional supplements such as glucosamine and chondroitin sulfate, nonsteroidal antiinflammatory drugs, and unloader bracing.
Operative options include arthroplasty, knee fusion, and osteotomy. We feel that a knee replacement is not a good option in young, active patients because it will significantly limit athletic activities as well as relegate the patients to a series of revision arthroplasties over their lifetime. A fusion is also a poor option in this patient population because of its dramatic effect on activity level and gait. Consequently, we recommend HTO to young, active patients with medial compartment osteoarthritis. The HTO is often accompanied by a concomitant microfracture chondroplasty of the medial compartment.
Of the techniques available, we prefer a medial opening wedge osteotomy. Traditional lateral closing wedge osteotomies are rarely used in our clinic due to concerns about shortening of an already shortened leg, potential problems with the proximal tibia-fibula joint and operating around the peroneal nerve, and the “one-shot” accuracy a closing wedge requires.4 In our clinic, we utilize an opening wedge osteotomy on the medial side of the proximal tibia in conjunction with a chondral resurfacing procedure in the degenerative varus knee. This technique allows more accurate realignment, applies tension to the “pseudo-lax” medial collateral ligament, involves small incisions that do not complicate future total knee arthroplasty, restores the native height to the tibia, and avoids complications involving the tibia-fibula joint and the peroneal nerve. The distraction osteogenesis technique is employed in patients who, for occupational or social reasons, are unable to tolerate an extended period of non-weight bearing, or in patients who require an angular correction that exceeds the capacity of plate fixation.

Figure 12-1 Preoperative radiograph.
Surgical Technique
The patient is positioned supine on a radiolucent operating table, which allows for fluoroscopic visualization of the hip to the ankle. Diagnostic arthroscopy is initially performed. Although grade IV chondral changes are often seen in the patellofemoral joint, we do not consider this to be a contraindication to an osteotomy. If extensive grade IV changes are visualized in the lateral compartment, we will not proceed with the osteotomy. The extent of grade IV changes in the medial compartment is then evaluated. Any concomitant pathology such as meniscal tears or loose bodies are then addressed arthroscopically.
The microfracture technique is then applied to the appropriate degenerative areas of the medial compartment. A repeat prep with Betadine paint sticks is performed, and a new extremity drape is applied. Following exsanguination of the leg, the thigh tourniquet is inflated to 250 mm Hg. The external fixator pins (EBI, Parsippany, NJ) are then placed 1 cm below the level of the articular surface, parallel to the joint line, typically bicortically if possible. Using the fixator as a guide, the distal pins are placed in a bicortical fashion through the mid-tibia. The pins are left in place, and the fixator is removed to facilitate access for the osteotomy.
Although a large incision with posterior retractors has often been utilized, we feel very safe and comfortable performing this osteotomy percutaneously. This gives us the advantage of maintaining the soft tissue envelope for callus formation.
A 2 cm longitudinal incision is made, 2 cm distal from the proximal pins and 3 cm medial to the tibial tubercle. To preserve the periosteal blood supply, no attempt is made to strip the soft tissues off the anterior or posterior cortex of the tibia. Utilizing a 4.8 mm drill bit, a bore hole is made in the medial tibia. A 3.2 mm drill bit is then utilized from within the medullary canal where multiple holes are made anterior and posterior from the starting hole. To prevent inadvertent posterior neurovascular compromise, we place the 3.2 mm drill bit on oscillation mode. The lateral cortex should not be violated. Next, a 3/4-inch stiletto osteotome is used to “connect the dots” of the multiple 3.2 mm drill holes. A closed osteoclasis is then performed to open the osteotomy site, attempting to preserve the integrity of the lateral cortex. Fig. 12-2 is a schematic illustration of the osteotomy site preparation.
The fixator is then applied, and the desired amount of correction is obtained intraoperatively (Fig. 12-3). This is done to ensure that the fixator can be opened enough to effect the desired correction, as well as to measure the ratio of millimeters opened at the osteotomy site versus the millimeters opened on the fixator. This allows calculation of the amount of fixator opening required per day to achieve the desired 1 mm of opening per day at the osteotomy. The fixator and osteotomy site are then closed down at the end of the procedure.
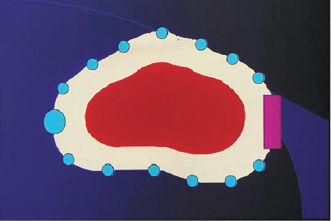
Figure 12-2 Osteotomy preparation. The purple rectangle represents the intact area of the lateral cortex that will serve as hinge for distraction.
On postoperative day 5, we begin distracting 1 mm a day at the osteotomy site. Radiographs are taken 1 week later to ensure that the osteotomy is opening appropriately. Opening is continued until the desired amount of correction is achieved (Fig. 12-4). We typically aim for 4 degrees of mechanical axis valgus, which places the weight-bearing line at the base of the lateral tibial spine. Radiographs are repeated 4 weeks following the completion of distraction to visualize the amount of consolidation (Fig. 12-5). The fixator is removed once adequate consolidation is achieved. The fixator is removed in the operating room; pin sites are overdrilled, and previous skin incisions are excised and closed after thorough irrigation with antibiotic solution. A second-look arthroscopy is often performed at this time to evaluate the regenerate cartilages.

Figure 12-3 Intraoperative distraction.
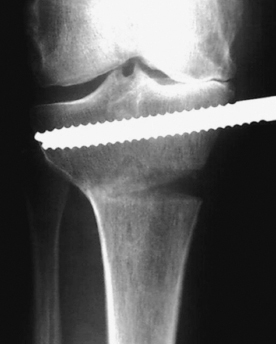
Figure 12-4 Three weeks after surgery.
Following the removal of the fixator, we allow weight bearing as tolerated as long as stable consolidation has been achieved. Fig. 12-6 illustrates the appearance of the osteotomy site 2 years after surgery.
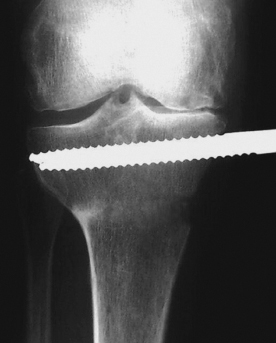
Figure 12-5 Early consolidation.

Figure 12-6 Two years after surgery.
Tips, Tricks, and Avoiding Pitfalls
- Attempt to limit the size of the pin site holes to prevent long-term drainage, and encourage pin care in a shower with a soft toothbrush.
- Perform the osteotomy percutaneously and use serial drill holes in an oscillating fashion from the intramedullary canal to weaken the bone prior to osteoclasis.
- Measure the amount of opening at the medial portion of the osteotomy and compare this to the amount of opening at the fixator. This will provide the ratio of fixator opening to osteotomy opening. The goal should be for 1 mm of osteotomy opening per day while distracting.
- Overdrill the pin sites following removal to sterilize this environment, in the event a total knee replacement may eventually be required.
Conclusion
In young, active patients with primarily medial compartment arthritis, high tibial osteotomy improves pain and allows a continued high level of activity. In a study of our patients undergoing chondral resurfacing and concomitant HTO at a minimum of 2-year follow-up, we found an average increase of 37.5 points in the Lysholm score, and 16.2 in the Western Ontario MacMaster (WOMAC) score. The average postoperative Tegner activity score was 5.0.5
A proximal tibial osteotomy, medial opening, or lateral closing will unload the medial joint,6 decrease the medial tibial sclerosis,7 and improve the adduction moment about the knee during gait.8, 9 Medial opening wedge osteotomy using distraction osteogenesis has several advantages over other techniques; specifically, it is more controllable than the “one-shot” accuracy of a closing wedge or an acute opening wedge. Utilizing a distraction technique allows fine-tuning of the alignment postoperatively and restoration of normal leg length. Regardless of the amount of correction required, we have not found it necessary to release the proximal tibia-fibula joint and have not developed any peroneal nerve complications. The incision should not complicate future knee replacement.
References
1 Aglietti P, Rinonapoli E, Stringa G, Taviani A. Tibial osteotomy for the varus osteoarthritic knee. Clin Orthop Relat Res 1983;176:239–245
2 Appel H, Freiberg S. The effect of high tibial osteotomy on pain in osteoarthritis of the knee. Acta Orthop Scand 1972;43:558–564
3 Matthews LS, Goldstein SA, Malvitz TA, Katz BP, Kaufer H. Proximal tibial osteotomy: factors that influence the duration of satisfactory function. Clin Orthop Relat Res 1988;229:193–200
4 Soejima O. Anatomic considerations of the peroneal nerve for division of the fibula during high tibial osteotomy. Orthop Rev 1994;23:244–247
5 Sterett WI, Steadman JR. Chondral resurfacing and high tibial osteotomy in the varus knee. Am J Sports Med 2004;32:1243–1249
6 McKellop HA. The effect of simulated fracture-angulations of the tibia on cartilage pressures in the knee joint. J Bone Joint Surg Am 1991;73:1382–1391
7 Akamatsu Y. Changes in osteosclerosis of the osteoarthritic knee after high tibial osteotomy. Clin Orthop Relat Res 1997;334:207–214
8 Goh JC, Bose K, Khoo BC. Gait analysis study on patients with varus osteoarthrosis of the knee. Clin Orthop Relat Res 1993;294:223–231
9 Wada M. Relationship between gait and clinical results after high tibial osteotomy. Clin Orthop Relat Res 1998;354:180–188
< div class='tao-gold-member'>









