High Body Mass Index
C. Lowry Barnes
Key Points
Introduction
The most recent data (2005) from the World Health Organization (WHO) estimate that approximately 1.6 billion people age 15 and older are overweight (i.e., body mass index [BMI] ≥25) (Table 84-1), and that at least 400 million people worldwide are obese (i.e., BMI ≥30).1 WHO data predict that by 2015, approximately 2.3 billion adults will be overweight, and more than 700 million will be obese. In 2008, six states had an obesity prevalence of greater than 30%, and Colorado was the only state with an obesity prevalence of less than 20%. Between 1991 and 2000, the number of people in the United States in the obese category grew by 60%.2 In the United States, obesity trails only cancer and coronary heart disease as the third most costly diet- and inactivity-related disease, at $117 billion annually.3 Total hip arthroplasty (THA) in obese patients presents the surgeon with challenges associated with the surgical procedure itself, the increased risk of perioperative complications, and postoperative recovery and performance of the implant. This chapter will focus on those aspects of THA performed in patients with high BMI (Table 84-2).
Table 84-1
International Classification of Adult Underweight, Overweight, and Obesity According to BMI
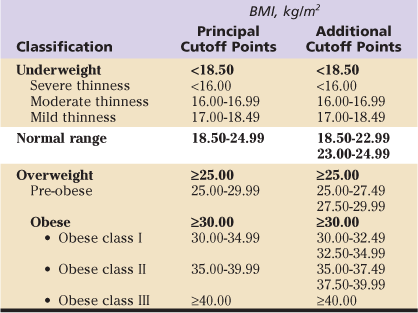
Data from World Health Organization (WHO): Physical status: the use and interpretation of anthropometry, report of a WHO Expert Committee, WHO Technical Report Series 854, Geneva, 1995, WHO; World Health Organization: Obesity: preventing and managing the global epidemic, report of a WHO Consultation, WHO Technical Report Series 894, Geneva, 2000, WHO; and World Health Organization (WHO)/International Association for the Study of Obesity (ASO)/International Obesity Taskforce (IOTF): The Asia-Pacific perspective: redefining obesity and its treatment, Melbourne, Australia, 2000, Health Communications.
Table 84-2
Summary of Representative Studies
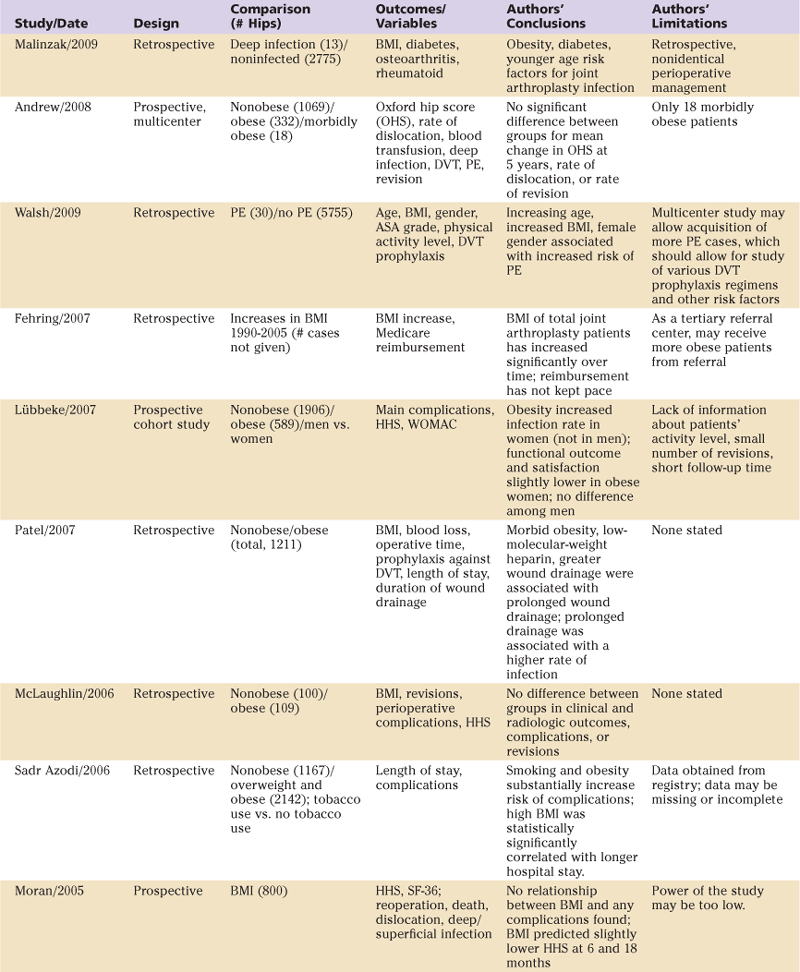
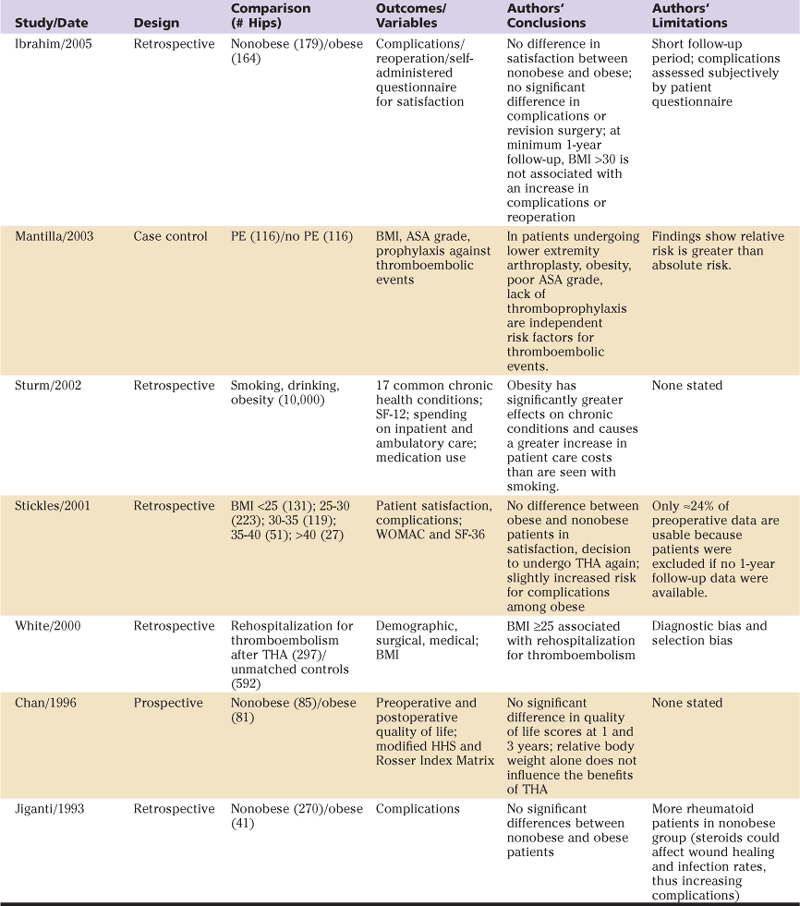
ASA, American Society of Anesthesiologists; BMI, body mass index; DVT, deep vein thrombosis; HHS, Harris hip score; PE, pulmonary embolism; SF, short form; THA, total hip arthroplasty; WOMAC, Western Ontario and McMaster University Osteoarthritis Index.
Indications/Contraindications
The most common indication for THA is osteoarthritis. Several studies have shown that obesity is likely to play a role in the development of osteoarthritis of the hip.4–8 Clinicians have postulated that “obese” (BMI, 30 to 39.9 kg/m2) and “morbidly obese” (i.e., BMI ≥40 kg/m2) patients undergoing THA pose greater technical difficulty for the surgeon, have more postoperative complications, and have poorer short- and long-term outcomes than “ideal weight” (BMI, 20 to 24.9 kg/m2) or “overweight” (BMI, 25 to 29.9 kg/m2) patients. In 1982, Sir John Charnley stated that obesity should be a contraindication to performing THA.9 Some surgeons advise obese patients to lose weight before undergoing THA, believing that THA in an obese patient would be technically demanding and would likely lead to increased postoperative morbidity.10 Possible concerns have included increased risk of infection, thromboembolism, and early implant failure (e.g., fatigue fracture).
Implant manufacturers today include some patient selection caveats in their precautionary statements to surgeons and include warnings in their product inserts, for example, “patients should be able to control their weight”; “excessive weight may adversely affect the implant”; “heavy patients can place high loads on the prosthesis which may lead to failure”; and “complications or failure may be more likely in heavy patients.”
Preoperative Planning
Preoperative planning for obese patients does not differ, in general, from planning for nonobese patients. Standard radiographic imaging should be performed. A radiographic marker may be more important for sizing because of increased distance between the hip and the radiographic plate. To facilitate postoperative evaluation and long-term follow-up, additional preoperative assessments can be valuable (e.g., Harris hip scores, Short Form [SF]-12 or SF-36).
It is advisable to encourage obese patients to attempt to increase upper body strength preoperatively because they must utilize an overhead frame on the hospital bed to assist in achieving early mobilization. As with all THA procedures, early mobilization is important to avoid an overall decline in function, venous thromboembolism, and respiratory complications. In addition, preoperative plans for other accommodative equipment should be made, such as a wide bedside commode and a wide walker. Preoperative planning should also include pharmacologic consultation to ensure careful administration of narcotic pain medications because obese patients often cannot tolerate as much narcotic as simple calculations based on an increased BMI might suggest. Finally, consideration should be given to bariatric surgery before elective primary THA for selected patients.
Description of Surgical Technique: Variations in Obese Patients
Few differences in operative technique have been described for obese patients undergoing THA. In general, a minimally invasive approach should be avoided in obese patients; however, any approach and incision that can achieve easy and adequate exposure while protecting the soft tissues is appropriate (Fig. 84-1). The author prefers a straight lateral position on the operating table, which allows fat/excess skin to “fall away” (Figs. 84-2 through 84-5), combined with an anterolateral approach and a cementless socket and stem. When a modular neck prosthesis is used, it is preferable to use a short straight neck to avoid increasing the risk of fatigue fracture of the femoral neck. For obese patients, low wear with large heads is preferred in the absence of other contraindications.

Figure 84-1 Long femoral elevating retractors are used in obese patients.

Figure 84-2 With appropriate use of retractors, excellent proximal femoral visualization can be attained.

Figure 84-3 A hip slide functions as a shoehorn to allow a clear pathway for hip reduction.

Figure 84-4 Visualization during reaming is increased when a thinner reamer driveshaft is used. Easily removable reamer baskets allow for placement of the reamer basket into the acetabulum and subsequent attachment of the reamer driveshaft.

Figure 84-5 A two-piece inserter for the acetabulum allows easy isolated placement of acetabular components into the reamed acetabulum before engagement with the impactor, which is narrow in diameter to allow for better visualization.
Intraoperative radiographic evaluation allows the surgeon to determine proper cup placement. With obese patients, a tendency to place the cup in a more abducted position in the acetabulum should be avoided, especially with hard-on-hard bearings, because this may result in increased wear. Intraoperative radiographs allow the surgeon to assess the equality of leg length, which can be more difficult to determine in obese patients. At the conclusion of the operation, two drains are placed: one deep to the fascia and the other in the subcutaneous space; then, a waterproof, compliant dressing is applied (Fig. 84-6).

Figure 84-6 A waterproof, compliant dressing helps prevent blistering and allows sealing of the wound dressing.
Postoperative Care
Studies have shown that obesity is associated with a number of operative and postoperative complications, making careful medical and pharmacologic management a priority. Obesity is an independent risk factor for type 2 diabetes mellitus, which is known to be associated with postoperative morbidity.11 Specifically, because of the strong association between diabetes and obesity, as well as the predictive value of diabetic glucose control and the risk of infectious complications, preoperative screening of obese patients for hemoglobin A1c (HgbA1c) levels may be advisable. Obesity is also associated with postoperative deep vein thrombosis (DVT) and pulmonary embolism after joint replacement surgery.12,13 Prolonged wound drainage and higher rates of wound infection are other well-known morbidities in the obese THA population.14,15 Prophylaxis against DVT is a must, and patients must be monitored closely after discharge as well. They are especially at risk for wound problems because of the need for DVT prophylaxis with low-molecular-weight heparin, fondaparinux, or warfarin and associated large “dead space” areas for hematoma development.16 Postoperative mobilization and activity are to be encouraged.
Effects of Obesity on THA: Results/Complications
It has been shown in a European study that orthopedic surgeons and their referring physicians have differing opinions about what patient factors affect long-term outcome after primary THA. Sturmer and associates17 used a standard questionnaire to conduct a multicenter, cross-sectional survey of 304 orthopedic surgeons and 314 referring physicians at 22 centers from 12 European countries. The questionnaire asked about seven patient characteristics and their effects on long-term outcome after THA. Participants were asked, “How would each of the following patient characteristics in your view affect the chances of a favorable long-term outcome of hip replacement (pain and function)?” Participant physicians were asked to make one choice to answer each question: (1) increases the chances of favorable outcome, (2) does not affect outcome, or (3) decreases the chances of favorable outcome. The seven patient characteristics were male gender, old age (>80 years), young age (<50 years), obesity, medical comorbidity, rheumatoid arthritis, and poor bone quality. Responses were analyzed using the Cochran-Mantel-Haenszel statistic.
A majority of participants in both groups of physicians believed that patient gender did not affect the chances of a favorable outcome. For old age patients, 56.2% of referring physicians believed that chances of a favorable outcome would be decreased, as did 40.5% of orthopedic surgeons, yet 23.3% of surgeons thought that old age increased the chance of success. For young age patients, 39.7% of surgeons thought chances of a favorable outcome would be decreased, and 37.1% of them thought young age increased the chances of success. Among referring physicians, a greater percentage (46.6%) thought that young age increased the chances of success. When considering obesity, 80.9% of orthopedic surgeons thought that this factor would decrease the chances of success, as did 89.1% of referring physicians. Statistical analysis of these responses revealed that differences in mean scores between orthopedic surgeons and referring physicians were statistically significant for old age (P < .0001), young age (P < .006), and obesity (P < .006). No major differences in mean response scores between physician groups were noted for significant comorbidities, rheumatoid arthritis, and poor bone quality, although a majority of participants in both groups agreed that these conditions would decrease the chance of a favorable long-term result.17 In many European countries, referral by a physician to an orthopedic surgeon is required for the patient to undergo THA. Results of this study showed that referring physicians believe that patients who are old or overweight, or who have comorbidities, might not benefit from THA; thus, they may not refer patients who would actually benefit from this procedure. Although orthopedic surgeons could not agree on the influence of “old age” on THA outcome, it may be concluded that referring physicians are even less well informed about the results of studies evaluating the success of total joint replacement in patients with variable physical and medical characteristics and conditions.
Studies of factors affecting long-term outcome of THA have reported variable results. For example, although it is generally agreed that patient gender does not independently affect the success or failure of the procedure, studies have shown that men can have better outcomes with regard to activities of daily living.18,19 Using age as a predictor of outcome after THA has also been inconsistent, with some studies associating advanced age with poorer outcomes20–29 and others finding no adverse effect related to advanced age.30,31 Along with age in years as a predictor of long-term outcome after THA, patient functional status and quality of life should be considered.31
With specific regard to obesity, Chan and Villar32 prospectively studied quality of life in obese patients after THA using Harris hip scores and the Rosser Index Matrix. Of 166 patients with adequate follow-up data, 85 were nonobese (BMI <25), 56 were grade I (mildly obese; BMI, 25 to 29.9), 25 were grade II and above (moderately obese; BMI, 30 to 39.9), and 1 patient had a BMI greater than 40 and was included in the grade II and above group. Average weights of patients in the different groups were not statistically significantly different. Quality of life scores for the nonobese group improved significantly at 1 year post THA (P < .001) and remained similar at the 3-year post-THA time point. For the grade I obese group, average scores improved significantly at both 1- and 3-year follow-up (P < .001 for both time periods). The grade II and above obese group showed improvements of similar magnitude in their quality of life scores, but because of the smaller number of patients in this group, improvements were not statistically significant. These results indicate that quality of life improvement for nonobese, mildly obese, and moderately obese showed no differences between groups, leading the authors to conclude that patients should not be excluded from undergoing THA based on obesity alone.32
Sadr Azodi and colleagues33 retrospectively studied the impact of obesity on postoperative complications and length of hospital stay after THA. They categorized patients as “highly obese” if BMI was greater than 35. Of the 3309 male patients studied, 2142 (64.8%) were considered overweight or obese. They found that BMI was significantly associated with increased length of hospital stay (P < .001); the mean length of stay for overweight patients was 4.7% (95% confidence interval [CI], 2.0 to 7.3) longer, and for obese patients was 7.09% (95% CI, 2.9 to 11.1) longer, than for patients of normal weight. Patients with increased BMI spent up to 7% longer in the hospital than normal weight patients. The authors found a trend for increased risk of postoperative complications with increasing BMI (P = .082); obese patients had a 58% increased risk (odds ratio [OR], 1.58; 95% CI 1.06 to 2.35) compared with patients of normal weight; study authors defined systemic complications as venous thromboembolism, acute cardiac or cerebrovascular events, postoperative anemia, blood transfusion or gastrointestinal bleeding, urinary tract infection, and pneumonia.33
Namba and coworkers15 prospectively evaluated 1071 THA patients to review the effects of obesity on perioperative morbidity. Their study categorized obesity as BMI greater than 30, high obesity as BMI greater than 35, and morbid obesity as BMI greater than 40. Patient data were obtained using a prospective joint replacement registry, and postoperative complications (superficial and deep space infections) were recorded up to 1 year post THA. Researchers defined superficial infection as wound drainage or erythema requiring intravenous antibiotics and prolonged hospital stay, or readmission, and deep infection as any infection treated operatively or with a positive culture.
Reviewers found that the mean BMI of highly obese patients was significantly greater than the mean BMI of non–highly obese patients (39.5 vs. 27; P < .001). Highly obese patients had significantly higher rates of two comorbid conditions compared with non–highly obese patients: diabetes mellitus, 14% vs. 9% (P < .04) and hypertension, 53% vs. 36% (P < .001). A trend for increased infection rate was observed among highly obese patients (1.3% vs. 0.3%; P = .09); the odds ratio yielded a 4.3 times higher risk for infection in highly obese patients.15
Andrew and associates34 conducted a prospective study of 1356 THA patients (1421 hips) from seven centers to determine whether clinical outcomes for obese versus nonobese patients differed. Patients were grouped according to BMI: nonobese (BMI < 30), obese (BMI 30 to < 40), and morbidly obese (BMI ≥ 40). Change in the Oxford hip score (OHS) was the primary outcome measure, and dislocation, hemorrhage requiring transfusion, deep infection, perioperative DVT requiring anticoagulation therapy, pulmonary embolism, and revision surgery were secondary outcomes. At 5 years post THA, 795 nonobese, 249 obese, and 15 morbidly obese hips were available for follow-up. Mean absolute OHS values (although improved greatly for each BMI group) of the obese and morbidly obese groups were significantly worse than that of the nonobese group (P = .005). However, all OHS results improved from preoperative values, thus illustrating the clinical benefit of THA for patients with an excessive BMI.34
A 2005 prospective study conducted in the United Kingdom consisted of 759 patients (800 hips) undergoing THA who were evaluated preoperatively and at 6 and 18 months postoperatively using SF-36 and Harris hip scores.35 Researchers recorded length of stay, death, dislocation, reoperation, superficial and deep wound infections, blood loss and need for transfusion, and concomitant medical problems (e.g., smoking, cancer, atherosclerosis, cardiac disease, diabetes mellitus, osteoporosis, thromboembolism). All patients completed the preoperative HHS and SF-36, and 774 were assessed at 6 months and 687 at 18 months post THA. The mean BMI was 27.8 kg/m2 (range, 17 to 49 kg/m2). A statistically significant improvement in HHS scores as compared with preoperative scores was noted at 6 and 18 months (P < .0001). A total of 7 deep and 56 superficial wound infections were reported; univariate analysis indicated that BMI might be associated with higher rates of superficial infection and lower HHS at the two postoperative time points (P < .05). However, additional statistical evaluation of postoperative HHS using multiple regression analysis showed that BMI was not a significant independent predictor of superficial wound infection. Multiple regression analysis further noted that a postoperative increase in BMI was inversely related to a change in Harris hip score at 6-month (P = .02) and 18-month (P < .001) evaluations; for every 1-point increase in BMI, the HHS decreased by 0.25 at 6 months and by 0.35 points at 18 months. Body mass index did not have an effect on early THA failure. The authors added that although higher patient body weight places a greater load on the arthroplasty, obese patients tend to be less active, which may temper the effect of greater BMI on the durability of the implant.35
One recent study evaluated the effects of obesity on complications, functional outcome, and satisfaction after THA with emphasis on identifying differences between men and women.36 This prospective study evaluated 2495 THAs (2186 patients), comparing outcomes of interest between obese and nonobese patients. The primary outcome was the prevalence of “main” complications (deep infection, dislocation, and revision); secondary outcomes included disease-specific quality of life, patient satisfaction, and general health, assessed using HHS, SF-12, two visual analogue scales measuring pain relief and function, and the Western Ontario and McMaster University Osteoarthritis Index (WOMAC). Obesity was more prevalent in male patients (26.7% vs. 20.5%). With a follow-up period ranging from 3 to 72 months, 91 hips with main complications were reported: Infection was more prevalent in the hips of obese patients (1.7% vs. 0.4%). Obesity in women was associated with infection (prevalence ratio of obese vs. nonobese women was 16.1; 95% CI, 3.4 to 75.7), but obesity among male patients did not appear to be associated with an increased infection rate (rate ratio, 1.0; 95% CI, 0.2 to 5.3). For dislocation, the adjusted rate ratio was 2.4 (95% CI, 1.4 to 4.2) among obese patients, and the prevalence of dislocation was approximately twice as high among men, but the relative rate increase due to obesity was higher in women (rate ratio, 3.0 vs. 1.8). Revision THA was performed in 13 nonobese and 8 obese patients (adjusted rate ratio, 2.0; 95% CI, 0.9 to 4.8). Among hips available for 5-year follow-up, 81% of hips in the nonobese group and 70% in the obese group had good to excellent results as measured by the HHS. Investigators found that obesity was related to increased infection and dislocation rates, as well as an increased need for revision due to septic loosening. Further, obese women had higher rates of infection than obese men, as well as lower functional outcome and less satisfaction with THA than obese men.36
Patel and colleagues14 studied the factors possibly related to prolonged wound drainage and their effects on rate of wound infection and longer hospital stay. They retrospectively reviewed the records of 1211 primary THAs, 15 of which developed acute infection postoperatively. Their analysis revealed that morbid obesity and prolonged wound drainage were statistically associated (P = .001), and that prolonged wound drainage led to significantly prolonged length of hospital stay (P < .001). Their analysis also revealed that for each day of prolonged wound drainage, the risk of wound infection increased by 42% following THA.14
Stickles and coworkers37 reviewed the relationship between obesity and patient subjective assessments of outcome after THA using the SF-36 instrument and the WOMAC questionnaire. They found no difference between obese and nonobese patients in terms of self-reported patient satisfaction, whether they would undergo total joint arthroplasty again, a physical component summary, a mental component summary, and WOMAC (all P > .05). The only difference between obese and nonobese patients was that obese patients reported difficulty in negotiating stairs at the 1-year postarthroplasty time point (odds ratio, 1.2 to 1.3). This observation, however, may apply to obese individuals in general, not just those who are post THA. 37
Jiganti and associates38 in 1993 reported on the safety of total joint arthroplasty performed in an obese population and noted that losing weight before total joint arthroplasty may have little effect on the patient’s postoperative course. Through a retrospective review of 51 nonobese and 103 obese THA patients, they found that intravenous fluid administration and total blood loss were slightly higher for obese patients, and that operative time was significantly longer for obese THA patients (P < .001). Investigators reported 0.29 minor complications per nonobese patient and 0.22 per obese patient. A total of 0.22 major complications occurred per nonobese patient and 0.10 per obese patient.38
A 2005 report by Ibrahim and colleagues39 assessed the effects of obesity on complications and reoperations after THA with a minimum of 1-year follow-up via a self-administered validated questionnaire. Patient satisfaction with the procedure was high, and no difference between obese and nonobese patient groups was noted. Similarly, no difference in length of hospital stay, American Society of Anesthesiologists (ASA) grade, or proportion of intraoperative complications, total complications, or revision procedures was observed. However, because of the short follow-up period in this study, the authors note that long-term studies are still necessary to determine further effects of obesity on outcomes of THA.39
A Mayo Clinic study found that preemptive bariatric surgery is beneficial for morbidly obese patients undergoing total joint arthroplasty. Parvizi and coworkers40 reported the results of THA in seven patients who underwent bariatric surgery before their total joint procedure. Average time from bariatric surgery to joint replacement was 23 months (range, 7 to 65 months). One staged bilateral THA and six unilateral THAs were reported. The follow-up period averaged 3.7 years (range, 2 to 11 years), and no patients were lost to follow-up. No radiographic evidence of loosening or wear of components was noted at the latest follow-up evaluation. Postoperatively, two cases of DVT were treated successfully with intravenous heparin and oral warfarin for 3 months. In two hips, superficial infection was treated with oral antibiotics. One revision was performed in a patient who underwent primary THA at age 25. After the bariatric surgery, the patient lost more than 40% of her weight and became very physically active, which may have contributed to early failure. In this series, patients who first underwent bariatric surgery had very acceptable results after total joint arthroplasty with few complications.40
Super-Obese Patients
Although the studies reviewed have shown, in general, acceptable and even equal results for obese and morbidly obese patients undergoing THA, one report focused on studying “super-obese” patients with BMI greater than 50. Polga and associates41 retrospectively reviewed the outcomes of 41 patients (43 hips) who underwent THA between 1996 and 2006, all with BMI greater than 50 (range, 50 to 77). The mean age of patients at surgery was 56.8 years, and the mean follow-up period was 36.8 months. In all, 17 surgical complications (39.5%) and 7 (17%) medical complications occurred; 5 patients died between 3 and 28 months postoperatively. Ten hips had prolonged wound drainage. The major complication rate was 12.2%, which included 15 reoperations (5 patients): 1 for irrigation and débridement with component retention, 3 for recurrent dislocation (2 of which became chronically infected requiring resection), 1 for periprosthetic fracture that also became infected and required resection, and 1 fractured stem that required revision 4 years after the index THA. Two intraoperative complications (1 acetabular fracture and 1 femur fracture) were treated at the time of primary THA. These high rates of complications should alert surgeons to counsel super-obese patients about the importance of weight loss before THA and suggest the advantages of preoperative referral to a bariatric surgeon.41
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








