Our hands are our primary tools for interacting with our environment. One may argue that the most significant function of the shoulder, elbow, and wrist is to position the hand in space. Once the hand is positioned, it is able to proceed with its functional task. Therefore, any abnormalities of hand function are important to evaluate and when possible treat, because of the critical role that our hands play in our daily routines.
The anatomy of the human hand is extremely complex, with many intricate mechanisms that allow us to grip a tennis racket, hold a pencil, or play the piano. Perhaps because of its intricacy, the care of the hand, both surgical and nonsurgical, has been relegated to specialists in hand surgery. Physiatrists have stayed on the sidelines. However, with a thorough understanding of the hand anatomy and pathophysiology, a well-trained physiatrist is in a strong position to manage all medical aspects of hand care.
The goal of this chapter is to provide a brief overview of common hand problems, their pathophysiology, and their treatment. Most of the treatment discussed is nonsurgical in nature. However, a brief overview of surgical options and their indications is also provided. A more detailed account of these clinical entities and their treatment is available in hand surgical texts and in this chapter’s reference section.
CARPAL TUNNEL SYNDROME
Carpal tunnel syndrome (CTS) is the most common compressive neuropathy in the upper extremity (
1) (
Tables 37-1 and
37-2). This condition typically causes paresthesias in the median nerve distribution. Fifteen percent of the general population has symptoms consistent with CTS. The prevalence of electromyogram-confirmed CTS is 3% in women and 2% in men. Prevalence is greatest in women older than 55 years (
2). It is more frequently found in people who are obese or smoke and in those with diabetes mellitus (
3,
4). Cervical root compression and thoracic outlet abnormalities can also be associated with CTS (
5). No hand preference, dominant or nondominant, has been identified, and 60% of patients have bilateral symptoms (
2,
6). Many factors contribute to the development of CTS, including vibration, local pressure over the carpal tunnel, awkward wrist positions, and forceful hand positions (
7,
8,
9). However, there remains considerable debate about whether CTS is a result of repetitive stress without other factors being present (
10,
11). Food processing, construction, and manufacturing are occupations that have a higher incidence of CTS (
12). Debate remains as to the association of CTS and computer keyboard work (
13,
14,
15). It has even been hypothesized that keyboard work may be associated with less CTS (
16).
The diagnosis of CTS is usually straightforward and is based on history and clinical evaluation. Electromyogram (EMG) is often used for diagnostic confirmation of CTS. It can measure the extent of damage and demyelination of the median nerve (
15). In mild cases, there may be an absence of electromyographic and nerve conduction changes. As symptoms progress, sensory distal latency is usually the first abnormal EMG finding. Therefore, the diagnosis of CTS is first established on history and clinical findings and then may be confirmed by EMG evaluation. Recently, there have been multiple reports on using ultrasound evaluation of the median nerve to diagnose CTS. These studies have shown that there is a change in the cross-sectional area of the median nerve when CTS is present (
17,
18,
19).
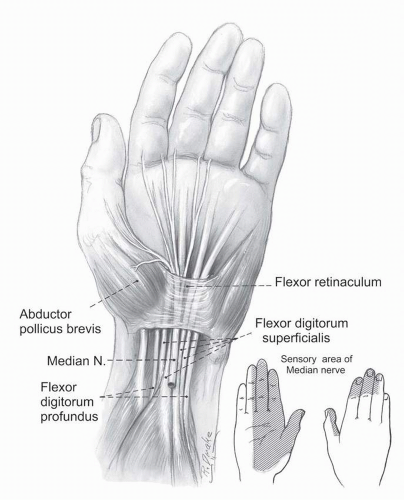
The carpal tunnel is located just distal to the palmar wrist crease. It is surrounded on three sides by the carpal bones, creating an arch. The radial wall is bordered by the scaphoid and trapezium, the dorsal is bordered by the lunate and capitate, and the ulnar wall is composed of the hamate. The arch is covered by a thick fibrocartilaginous band called the
flexor retinaculum (or transverse carpal ligament.) Nine tendons—two tendons that flex each finger, flexor digitorum superficialis (FDS) and flexor digitorum profundus (FDP), and one to the thumb, flexor pollicis longus (FPL)—course through the carpal tunnel (
20). The median nerve traverses with these tendons through the tunnel on its way to provide innervation to the thenar muscles and to provide sensation to the radial three and one half digits (
Fig. 37-1).
CTS is thought to be the result of increased pressure within the fibroosseous tunnel. Normal pressure within the carpal tunnel is 7 to 8 mm Hg with the wrist in neutral. Increased pressure of 30 mm Hg can result in symptoms of CTS and 90 mm Hg can be observed with wrist flexion and extension (
21,
22). This pressure increase causes relative ischemia and impaired nerve conduction of the median nerve (
23,
24). If abnormally increased pressure continues, segmental demyelination occurs. The median nerve sensory fibers are the first to be affected owing to their extensive myelination and high metabolic demands. Prolonged pressure causes injury to the motor fibers, and weakness ensues. The prevalence of CTS increases with pregnancy, inflammatory arthritis, distal wrist fracture, amyloidosis, hypothyroidism, diabetes, acromegaly, and in individuals who use corticosteroids and estrogens (
13,
20,
25). One third of all cases of carpal tunnel are associated with these
medical conditions (
26); diabetes is the most common association (
13,
26).
The typical symptoms of CTS are numbness, tingling, pain, burning, or a combination of these (
27). These symptoms occur in the radial three and one half digits: the thumb, index, middle, and half of the ring finger. CTS often causes nocturnal awakening secondary to the hand paresthesias. These nocturnal symptoms are 51% to 77% sensitive and 27% to 68% specific for CTS (
28). Gripping, driving, holding vibrating objects, or prolonged pinching, such as holding a book, may result in increased paresthesias. Many patients describe relief of their symptoms with shaking of the hands (
29). With progression, patients may describe an awkward feeling or weakness of the hand and begin dropping objects.
Physical examination (
Table 37-3) usually begins with the exclusion of any cervical, shoulder, or elbow pathology, which may produce similar symptoms. C6 radiculopathies are often confused with CTS because the sensory symptoms involve the radial aspect of the hand. Strength testing should include wrist flexion-extension, grip, and thumb opposition. Specific CTS provocative tests include Phalen’s test, in which the wrist is held in full passive wrist flexion. This position increases pressure within the carpal tunnel and may reproduce paresthesias
in individuals with CTS. This test has a wide reported range of sensitivity and specificity (40% to 80%) (
28,
30,
31). The time to the development of paresthesias should be noted because it can be used to monitor change with treatment. Tinel’s test involves tapping the median nerve just proximal to the transverse carpal ligament (
32). Reproduction of the paresthesias into the hand by the Tinel’s test is 20% to 60% sensitive and 67% to 87% specific for CTS (
30,
31). Carpal tunnel compression involves pressure placed with the examiner’s thumb or index and long fingers over the carpal tunnel. This pressure is maintained for 30 seconds to 1 minute and if positive will reproduce paresthesias. Durkan (
33) believes that this test is more sensitive and specific for CTS than Tinel’s or Phalen’s test.
Treatment of CTS begins with modification of repetitive or awkward activities that precipitate paresthesias. Splinting the wrist in a neutral position at night has been demonstrated to reduce symptoms in 80% of patients (
34,
35). Nonsteroidal anti-inflammatory drugs (NSAIDs), diuretics, vitamin B6, and oral steroids have been tested, but no specific recommendations have been given for their prolonged usage (
27,
36). Therapeutic interventions such as ultrasound, iontophoresis, gentle stretching and strengthening exercises, ice, and carpal tunnel protection principles may be employed. Their application is clinically accepted but not scientifically determined to be efficacious. Protection principles stress avoidance of positions or activities that increase pressure within the carpal tunnel. Nerve and tendon gliding exercises have been described and are thought to be useful (
37,
38,
39). Acupuncture and yoga have also been demonstrated to decrease symptoms (
40).
Corticosteroid injections into the carpal tunnel are recommended if splinting and other conservative measures fail to reduce the symptoms. They have been shown to decrease symptoms in 75% of patients and improve nerve conduction (
41,
42,
43,
44). These injections are performed in a sterile fashion with needle placement ulnar to the palmaris longus. The needle is directed dorsally, distally, and radially at a 45-degree angle. In patients with severe CTS, 80% have return of symptoms in 1 year despite appropriate conservative care (
21). If the patient has signs or symptoms of constant numbness, loss of sensation, or thenar muscle atrophy lasting longer than 1 year, serious consideration of surgery is recommended (
20). There are many approaches to a CTS release. Traditionally, an open incision has been performed and the transverse carpal ligament resected. Endoscopic CTS release can be performed but may pose a slightly greater risk for injury to the median nerve (
45). Relief of symptoms is similar in the two approaches, but patients typically return to work quicker with the endoscopic technique (
46,
47). Postoperative rehabilitation versus home exercises seem to have the same outcomes, except that it has been shown that rehabilitation hastens the time to return to work (
48).
ULNAR NEUROPATHY
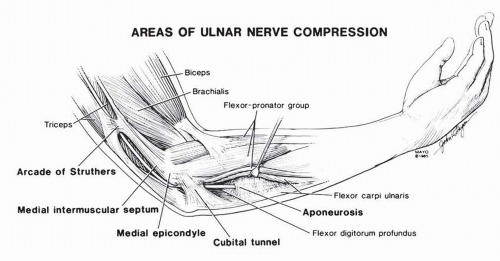
The ulnar nerve may be compressed at a number of points along its course. There are four areas of common compression around the elbow and one area at the wrist at Guyon’s canal. The areas of compression about the elbow include the medial intermuscular septum, the arcade of Struthers, the cubital tunnel, and the deep flexor aponeurosis (
49) (
Fig. 37-2). Compression of the ulnar nerve at Guyon’s canal may be secondary to thrombus at the ulnar artery (hypothenar hammer syndrome) or to ganglion cyst from the pisotriquetral joint or the triquetral hamate joint.
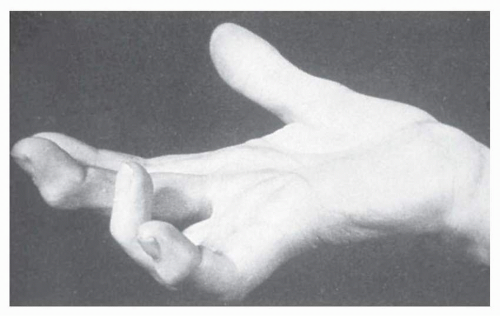
Ulnar neuropathy at the elbow produces weakness of the wrist ulnar deviators, the lumbricals of the ring and small fingers,
and all of the interosseus muscles. Sensory loss is at the ulnar side of the hand extending from the wrist crease to the tips of the small finger and ulnar half of the ring finger both dorsally and in a palmar direction. Entrapment at Guyon’s canal spares the wrist muscles as well as the dorsal hand cutaneous sensation. A small sensory branch of the ulnar nerve, the superficial cutaneous branch, is also spared, thus preserving a small area of sensory innervation to the base of the hypothenar eminence. Patients may complain of pain at the medial elbow and anywhere along the course of the ulnar nerve. Numbness and paresthesias may also be present. Weakness is usually a later sign. Patients may develop atrophy of the interosseus and hypothenar muscles and show posturing of their hand. Because the extrinsic finger extensors are spared, a mismatch of strength is seen between the extrinsic and intrinsic finger muscles. This disparity produces the classic “claw” deformity of the fingers. Because the lumbricals of the index and long fingers are median nerve innervated, these two digits may show normal posturing. This “clawing” of the ring and small fingers is called the “benediction sign” (
Fig. 37-3).
The conservative treatment of ulnar neuropathy at the elbow is based largely on protection principles. The ulnar nerve in the cubital tunnel lies in a position that is vulnerable to trauma. Therefore, counseling the patient to avoid leaning the elbow on tables, counters, or arm rests may prevent repetitive trauma to the nerve. The patient may also wear various forms of elbow pads or protective elbow sleeves. These not only cushion the cubital tunnel area but also serve as a constant reminder to the patient to avoid pressure on the elbow.
Even though the cubital tunnel resides at the center of rotation for the elbow joint, flexing the elbow may still stretch the ulnar nerve. This is possible because the ulnar nerve may show as much as 21.9 mm of excursion at the elbow and 23.2 mm at the wrist with combined motion of the shoulder, elbow, wrist, and fingers (
50). This excursion may be inhibited by fibrosis or entrapment of the nerve at one or more of the aforementioned compression sites. Thus, the normal gliding of the ulnar nerve may be limited and cause tension on the nerve with movement either proximal or distal to the elbow as well as with elbow flexion and extension. The patient should be counseled to avoid prolonged elbow flexion or posturing of the upper extremity in any position that reproduces their symptoms.
Surgical decompression or transposition of the ulnar nerve should be considered when the site of compression is clear either by EMG findings or by imaging and when the symptoms are progressive or debilitating. Many types of idiopathic ulnar neuropathies may be unresponsive to surgical treatment or may improve spontaneously. Nonetheless, when invasive treatment is considered, there are three major categories of surgical treatments for ulnar neuropathy at the elbow (
51). The first is simple decompression of the nerve usually combined with medial epicondylectomy. The second and third are subcutaneous and submuscular transpositions of the ulnar nerve. In general, greater amounts of dissection around the elbow lead to greater chances of postoperative elbow stiffness. Moreover, the amount of manipulation of the ulnar nerve is directly related to the chances of damage or continued neuropathy postoperatively. Therefore, the simpler procedures of decompression tend to be the safest. However, placing the ulnar nerve anterior to the medial epicondyle protects it from direct trauma and from stretching. In addition, the deeper the nerve is buried, the less chance for further trauma to the nerve.
THUMB CARPOMETACARPAL OSTEOARTHRITIS
Basilar thumb osteoarthritis is the most common symptomatic arthropathy of the hand. Thirty-three percent of postmenopausal women older than 50 years have radiographic evidence of osteoarthritis of the thumb carpometacarpal (CMC) joint (
52). The etiology of CMC arthritis is likely to be multifactorial, including genetic, environmental, and physiological contributions (
53). The thumb CMC joint is a double-saddle configuration. This configuration allows for movement in multiple planes such as flexion-extension, adduction-abduction, and pronation-supination. Sixteen ligaments have been described stabilizing the trapezium and the CMC joint (
54). The most important of these is thought to be the so-called beak ligament or deep anterior oblique ligament. Ligamentous laxity plus axial loading of the joint are thought to be major contributors to the development of osteoarthritis at the base of the thumb. However, there may also be a link between hand osteoarthritis and obesity (
55).
Classification of the thumb OA is radiographic and is graded according to the change in the trapeziometacarpal space, degree of synovitis, and subluxation. Stage 1 is associated with a normal joint space, whereas stages 2 to 4 have a decreased joint space. Stage 3 has obligatory osteophyte changes and sclerosis of the joint. Stage 4 has all of the observations plus involvement of the scaphotrapezial joint (
56). Symptoms vary with each stage.
In the treatment of basilar thumb degenerative joint disease (DJD), one tries to manage the symptoms. No cure is known. We are not even sure that we can slow the progression of the disease. Ideally, the patient acquires new prehensile patterns and adaptive equipment in order to minimize symptoms and maximize function. No single intervention is necessarily superior to others. There is no specific time frame or window of opportunity to follow. The CMC joint biomechanics is such that any pinch force generated at the thumb and
index finger is greatly magnified at the CMC joint interface. In fact, 1 kg of pinch force translates to 12 kg of intra-articular pressure; thus, one strives to minimize fingertip-to-fingertip pinch activities (
57). When pinching cannot be avoided, one tries to increase the size of the objects being pinched. In other words, the greater the distance between the thumb and the fingertip, the less pressure on the CMC joint; therefore, enlarging the grip of tools or objects that are being gripped decreases the pressure at the base of the thumb.
Twisting activities also stress the CMC joint by causing a torque or twisting force on the joint. Therefore, various gadgets such as key holders and electric can openers may be helpful. In addition, one may use pens, kitchen utensils, or gardening implements with built-up grips. Many companies manufacture such items.
Splints are used to help stabilize the thumb, reducing pain and enabling more symptom-free function. There are two commonly used splints for this problem: a short opponens splint which is hand-based and crosses the first metacarpophalangeal (MCP) joint; and a long opponens splint which is forearm-based, supports the wrist, and crosses the interphalangeal joint. Patients typically best tolerate the long opponens, forearm-based splint at night and prefer the less obstructive hand-based splint for daytime activities. These splints usually put the thumb in palmar abduction with the MCP in 30 degrees of flexion. Several authors have documented benefits from splinting in stabilizing the joint and providing pain relief (
53,
58). Others have found studies of the efficacy of splints to be methodologically weak and unconvincing (
58a). Splints usually are not successful in symptom reduction when there is fixed deformity of the joint. A review of the evidence for splinting the CMC joint in arthritis is available (
59).
Many patients use pain-relieving modalities such as contrast baths, hot-water soaks, or paraffin baths. Anti-inflammatory medications are often used for pain control. In addition, one may consider cortisone injections into the CMC joint (
60). If the patient has involvement of the scapho-trapezio-trapezoidal (STT) joint, this may be injected at the same time with a single needle stick.
As a last resort, some patients may consider surgical options for basilar thumb DJD. The most common procedure used to treat this problem is ligamentous reconstruction of the joint (
61). The trapezium is wholly or partially excised. The base of the first metacarpal is then reattached to the carpus using a tendon slip from the flexor carpi radialis (FCR), the abductor pollicis longus (APL), or the extensor pollicis brevis (EPB). Various techniques are used to weave the tendon between the bases of the first and second metacarpals with the distal scaphoid. Some variations also employ the remaining tendon slip as a cushion to fill in the gap left by the trapezium. This is also called the ligamentous reconstruction tendon interposition (LRTI) or the “anchovy” procedure. Although the tendon reconstruction procedures help restore mobility of the thumb and reduce pain, they are not suited for heavy activities or manual labor. The patients requiring a large amount of grip strength and durability would be better served by arthrodesis of the joint (
62,
63). This allows for quicker recovery and preservation of grip strength. The tendon reconstruction method requires 6 months of recovery and often only results in 60% to 70% of normal grip and pinch strength (
64). Various interposition arthroplasty procedures are less common and are not as well established as tendon or fusion procedures.
Other sequelae of osteoarthritis, such as instability or pain of the first MCP joint, may contribute to pain and prehensile abnormalities.