Hallux Osteotomies
Thomas F. Smith
Jared L. Moon
The goals of corrective surgical procedures involving the hallux include realigning linear or angular deformities of the proximal and distal phalanx, addressing any catharsis at the hallux interphalangeal joint (HIPJ), or both (1,2). The choice of hallux phalangeal osteotomies or arthrodesis of the HIPJ is based not only on the location of the deformity within the hallux but also on the involvement of the HIPJ with patient complaints and needs. Patient complaints and needs addressed with HIPJ arthrodesis include joint pain with or without angular hallux deformity, muscle imbalance of the hallux, and HIPJ instability. Patient complaints and needs addressed with hallux osteotomies include painful hallux and second toe interdigital keratoses, hallux to shoe irritation problems, extrinsic hallux muscle-tendon positioning and cosmesis. Preoperative evaluation to aid surgical procedure selection involves not only assessment of any clinical and radiographic angular deformities of the first ray but also hallux and first ray joint assessment.
Hallux phalangeal osteotomies are primarily utilized as a component of hallux abducto valgus corrections. As the first ray surgical correction process progresses in hallux valgus surgery, changes in first metatarsal and hallux phalangeal angular positioning can occur through procedures remote from the actual site of correction. Reassessment of these changing angular first ray alignments is important to appreciate for possible intraoperative alterations or adjustments in the preoperative surgical plan. A preoperative plan to perform a hallux osteotomy may be obviated by improved overall hallux positioning following the first metatarsal osteotomy, first metatarsophalangeal joint (MTPJ) soft tissue reconstruction or both (1,3,4,5,6,7 and 8). Proximal phalangeal osteotomies of the hallux can be expected to correct primarily phalangeal hallux angular deformities and not necessarily first ray deformities in general (1,3,9). Similarly, the use of first metatarsal or first MTPJ procedures to address significant hallux phalangeal angular issues can result in other malalignment problems of the first ray.
In terms of surgical technique multiple incisional approaches, osteotomy site orientations and locations, and bone fixation options are available for hallux phalangeal osteotomies. There are advantages and disadvantages to be considered in the choice of each possibility. Their selection and use is determined by both the level of the deformity to be corrected as well as meeting the needs and expectations of the patient. Hallux osteotomies may be performed alone in isolated hallux interphalangeal deformities or as an adjunctive procedure in more complex first ray deformities based on specific patient needs (10,11,12,13 and 14). Since Akin (15) first described the proximal phalangeal osteotomy for hallux valgus correction in 1925 that has come to bear his name, refinements not only in surgical technique but also in indication and application have helped define the role of this procedure in first ray pathology (Fig. 26.1).
EVALUATION AND DIAGNOSIS
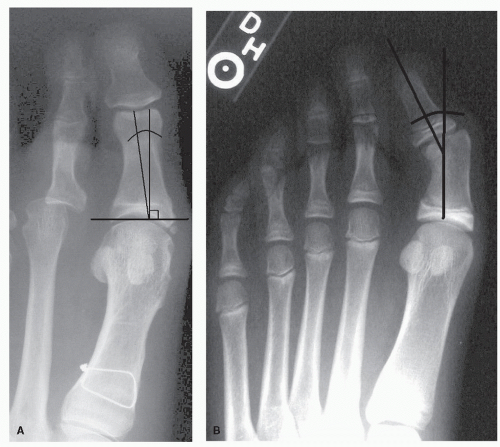
The clinical and radiographic signs that imply the need to consider a phalangeal osteotomy of the hallux are multiple. The most prominent clinical sign is an angular deformity of abduction in the transverse plane isolated within the hallux itself (Fig. 26.2). This deformity has been termed hallux abductus interphalangeus or simply hallux interphalangeus. Negating other first ray clinical pathology such as medial prominence of the head of the first metatarsal or hallux valgus at the MTPJ, the hallux within itself appears abducted. The hallux interphalangeal abductus may appear to arise more proximally within the base of the proximal phalanx of the hallux or more distally at the HIPJ. Angular deformity at the base of the proximal phalanx represents an increase in the angle the proximal articulation of the base of the proximal phalanx makes with the long axis of the proximal phalanx. Angular deformity more distally within the hallux represents abduction of the long axis of the distal phalanx relative to the long axis of the proximal phalanx. The more distal deformity is an abduction of the distal articular surface of the proximal phalanx relative to the long axis of the proximal phalanx. More proximal hallux phalangeal abduction is clinically evidenced by angulation within the hallux itself toward the second toe in the presence of a congruous first MTPJ without significant structural deformity of the distal articulation of the first metatarsal. The hallux appears linear and not angular at the HIPJ. More distal hallux phalangeal abduction is clinically evidenced by the transverse base of the hallux nail appearing angulated in abduction relative to the proximal phalanx or long axis of the hallux. Passive clinical flexion of the HIPJ results in an exaggeration of the hallux interphalangeal abductus with the hallux underlapping the second toe in more distal deformities. This is not seen in more proximal hallux phalangeal angular deformity.
In the presence of clinical hallux interphalangeal abductus, whether alone or in conjunction with other first ray angular deformities, the HIPJ should be assessed for degree of motion, contracture, and pain. Limited HIPJ motion can be seen with hallux interphalangeal abduction deformity, following hallux trauma, any of the arthritides that can affect the foot, or a history of prior hallux surgical intervention. Careful assessment of the HIPJ may demonstrate a degree of joint flexion or extension contracture as either a flexible or rigid deformity. HIPJ flexion deformity can be seen in hallux interphalangeal abductus deformity especially in congenital deformities of childhood, as well as hallux varus as a complication of previous attempted hallux valgus correction. HIPJ dorsiflexion deformity can be seen in hallux rigidus. Clinical symptoms of hallux interphalangeal abductus deformity may include painful interdigital keratoses between the hallux and second toe or keratoses overlying the medial HIPJ area from shoe pressure. An abduction angulation within the hallux may result in the hallux underriding or
overriding the second toe resulting in subsequent second digital deformity and symptoms. Patient concerns may be more cosmetic than involving pain. Aesthetically, the hallux is typically parallel to the second and lesser toes not overly angled relative to them on the transverse plane. The hallux is generally more visually acceptable with the nail facing directly upward and not rotated on the frontal plane. The distal digital parabola is more variable for the hallux in visual terms acceptable as either somewhat shorter or longer than the second toe. The hallux nail base and HIPJ should be relatively perpendicular to the long axis of the toe.
overriding the second toe resulting in subsequent second digital deformity and symptoms. Patient concerns may be more cosmetic than involving pain. Aesthetically, the hallux is typically parallel to the second and lesser toes not overly angled relative to them on the transverse plane. The hallux is generally more visually acceptable with the nail facing directly upward and not rotated on the frontal plane. The distal digital parabola is more variable for the hallux in visual terms acceptable as either somewhat shorter or longer than the second toe. The hallux nail base and HIPJ should be relatively perpendicular to the long axis of the toe.
Radiographic evaluation of the proximal and distal phalanx of the hallux as well as their relationship not only to one another but the first ray in general must be correlated with the overall clinical evaluation of hallux abducto valgus with associated hallux interphalangeus deformity, as either alone can be misleading (Figs. 26.2 and 26.3). The transverses plane angular relationship on the anteroposterior foot radiograph of the long axis of the proximal phalanx of the hallux to the long axis of the first metatarsal is the hallux abductus angle and is normally 15 degrees abducted (16). The angular relationship of the long axis of the proximal phalanx to the distal phalanx of the hallux is termed the hallux interphalangeal angle (HIA) and is normally 10 degrees abducted (16). The angular relationship of the articular surface at the base of the proximal phalanx to the long axis of the proximal phalanx is termed the distal articular set angle (DASA) and is normally 7.5 degrees (16). An increase of abduction within the hallux itself is typically within the proximal phalanx with an elongated medial margin relative to the lateral margin. This medial elongation can represent two possible deformities of the proximal phalanx, as noted clinically. The first is an increase in DASA that represents a more proximal deformity within the proximal phalanx. Radiographic measurement of DASA can be affected by arthritic deformity and exostosis formation at the base of the proximal phalanx of the hallux as well as varus or valgus malpositioning of the hallux on the frontal plane of the anteroposterior foot radiograph. The second is an increase in the HIA that represents an angular malalignment of the distal aspect of the proximal phalanx. Radiographic assessment of the HIA can be difficult if frontal plane hallux rotation, as commonly seen in hallux abducto valgus deformity, affects a strict anteroposterior radiographic view of the hallux. Abduction deformity through the distal phalanx,
either congenital or traumatic in origin, is rare but possible and can be misleading. On the lateral foot radiograph in the sagittal plane the distal and proximal phalanx are relatively linear and parallel. Any angular malalignment of dorsiflexion or plantarflexion should be correlated with clinical deformity.
either congenital or traumatic in origin, is rare but possible and can be misleading. On the lateral foot radiograph in the sagittal plane the distal and proximal phalanx are relatively linear and parallel. Any angular malalignment of dorsiflexion or plantarflexion should be correlated with clinical deformity.
 Figure 26.2 Hallux abductus interphalangeus. Clinical presentation of hallux deformity arising more proximally within the hallux (A) and arising more distally within the hallux (B). |
Ongoing clinical and radiographic intraoperative assessment of first ray deformity corrections is important especially where hallux phalangeal osteotomies such as the Akin osteotomy are considered in multilevel first ray pathologies. The Akin osteotomy is typically performed as one of the last steps in the overall first ray correction process. In multilevel hallux valgus corrections, the first metatarsal is generally realigned first by such procedures as a first metatarsal osteotomy or first metatarsocunieform arthrodesis after completing the first MTPJ arthrotomy and joint release. The relationship of the distal articular cartilage of the first metatarsal to its long axis and the proximal articular set angle (PASA) is then visually assessed and redirected by osseous correction if needed. The first MTPJ is then carefully manually reduced to a congruous alignment. The position of the hallux relative to the second toe can then be most appropriately assessed. Any persistent abductory deformity within the toe itself may require an Akin osteotomy type procedure for correction. Performing the Akin osteotomy sooner in this sequential approach surgical process may be premature and found not to have been necessary resulting in hallux overcorrection or hallux varus positioning (17). Realigning the hallux away from the second toe by medial first MTPJ capsular tightening in the presence of a high DASA or HIA can result in inadvertent medial first MTPJ subluxation. This is especially possible when an increased DASA deformity of the proximal phalanx exists (Fig. 26.4). The first ray deformity reduction assessments are primarily visual, but can be correlated with intraoperative radiographs as needed.
Contraindications to the Akin osteotomy include performing the osteotomy only to reduce a high HIA even in the presence of a satisfactorily corrected position of the hallux relative to the first ray and lesser toes through other means. The relatively parallel clinical relationship of the hallux to the second and lesser toes is the primary goal of hallux positional deformity correction, not necessarily establishing a normal HIA. Conversely, overcorrecting an Akin osteotomy to create a parallel lesser digital relationship without correcting the other components of the first ray deformity may not be appropriate. An increased HIA or DASA requiring correction combined with rigid flexion deformity or pain at the HIPJ may indicate more a need to consider HIPJ arthrodesis with angular realignment of the proximal and distal phalanx than consideration of an Akin osteotomy. A significant degree of lesser digital abductus, as seen typically in
the metatarsus adductus foot or rheumatoid foot, may warrant consideration for not correcting an increased HIA or PASA to maintain the more cosmetically acceptable parallel hallux and lesser digital positioning over the possibility of a wide spacing from the hallux to the second toe. The same principles apply for a significant degree of lesser digital adductus. Postoperative splinting of a proximal phalangeal osteotomy may delay early range of motion of the first MTPJ in hallux rigidus surgical corrections coincidentally associated with hallux angular deformity. Painful interdigital keratosis between the hallux and second toe may be as a result of an increased HIA and undue interdigital contact or simply a prominent lateral base of the distal phalanx of the hallux abutting the proximal interphalangeal joint of the second toe. In the absence of an increased HIA, resection of the prominent base alone may be indicated, not an Akin osteotomy. An Akin osteotomy may be combined with resection of the prominent lateral base of the distal phalanx where combined deformity of a prominent base and an increased HIA exists.
the metatarsus adductus foot or rheumatoid foot, may warrant consideration for not correcting an increased HIA or PASA to maintain the more cosmetically acceptable parallel hallux and lesser digital positioning over the possibility of a wide spacing from the hallux to the second toe. The same principles apply for a significant degree of lesser digital adductus. Postoperative splinting of a proximal phalangeal osteotomy may delay early range of motion of the first MTPJ in hallux rigidus surgical corrections coincidentally associated with hallux angular deformity. Painful interdigital keratosis between the hallux and second toe may be as a result of an increased HIA and undue interdigital contact or simply a prominent lateral base of the distal phalanx of the hallux abutting the proximal interphalangeal joint of the second toe. In the absence of an increased HIA, resection of the prominent base alone may be indicated, not an Akin osteotomy. An Akin osteotomy may be combined with resection of the prominent lateral base of the distal phalanx where combined deformity of a prominent base and an increased HIA exists.
PROCEDURE SELECTION
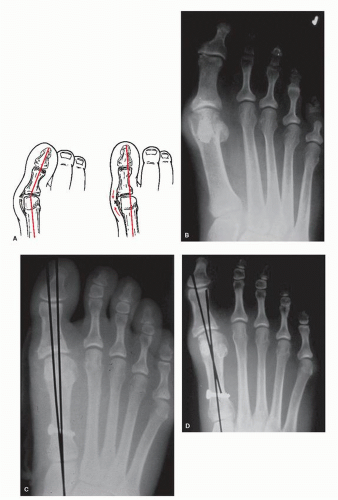
A proximal phalangeal osteotomy or Akin osteotomy to correct abductory deformity of the hallux within itself can be performed at the base, midshaft, or head of the proximal phalanx (Fig. 26.5). The osteotomy has a medial base and a lateral apex and may be oriented either transverse or oblique through the proximal phalanx. The goal of the Akin osteotomy is basically to shorten the medial side of the proximal phalanx relative to the lateral side creating a more parallel relationship of the two proximal phalangeal articular surfaces. This goal can be accomplished with an osteotomy of the proximal phalanx regardless of the osteotomy location within the phalanx. The choice of performing a proximal or distal osteotomy within the proximal phalanx of the hallux is the subtle difference between a high DASA and a high HIA. Both represent a longer medial and shorter lateral surface of the proximal phalanx. The distinction of a high DASA relative to a high HIA is more the clinical and radiographic apex of the
deformity within the proximal phalanx. A high DASA is a more proximal malalignment of the proximal joint surface of the proximal phalanx to its long axis resulting in a longer medial surface relative to the lateral surface of the proximal phalanx. The main body of the proximal phalanx is in a relatively normal alignment to the distal phalanx. This relationship results in a more subtly proximal hallux interphalangeal abductory deformity. The distal phalanx does not appear angulated to the proximal phalanx distally within the hallux. A hallux abductus interphalangeus as a result of an increased DASA responds best to a transverse osteotomy of the base of the proximal phalanx or an oblique osteotomy with the apex proximally oriented (Fig.26. 6).
deformity within the proximal phalanx. A high DASA is a more proximal malalignment of the proximal joint surface of the proximal phalanx to its long axis resulting in a longer medial surface relative to the lateral surface of the proximal phalanx. The main body of the proximal phalanx is in a relatively normal alignment to the distal phalanx. This relationship results in a more subtly proximal hallux interphalangeal abductory deformity. The distal phalanx does not appear angulated to the proximal phalanx distally within the hallux. A hallux abductus interphalangeus as a result of an increased DASA responds best to a transverse osteotomy of the base of the proximal phalanx or an oblique osteotomy with the apex proximally oriented (Fig.26. 6).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree