CHAPTER 2 Gross Anatomy of the Subtalar Joint
The subtalar joint is a complex and functionally important joint of the lower extremity that plays a major role in the movement of inversion and eversion of the foot.1,2 The complex anatomy of the subtalar joint makes arthroscopic and radiographic evaluation difficult. However, advances in small joint arthroscopic techniques and instrumentation have expanded the use of arthroscopy in the subtalar joint. Arthroscopic visualization of the subtalar joint includes the posterior joint, anterior joint, and sinus tarsi. The tarsi sinus is extra-articular, but for practical purposes, it is included in the description of subtalar arthroscopy and the relevant anatomy.
The surgeon must comprehend the gross and arthroscopic anatomy of the subtalar joint to improve surgical performance and recognize abnormal pathology. Because the lateral and posterior anatomic approaches are used for performing subtalar joint arthroscopy,3–6 knowledge of the superficial anatomy in these areas is important.
SUBTALAR JOINT ANATOMY
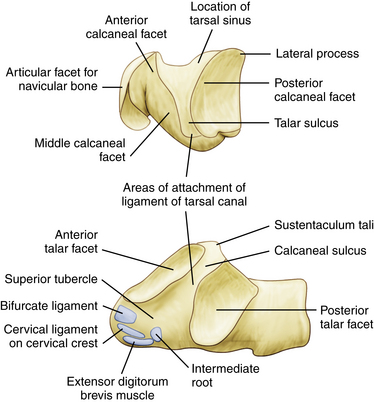
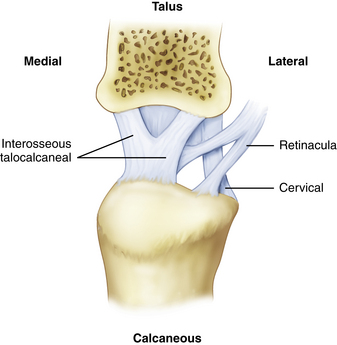
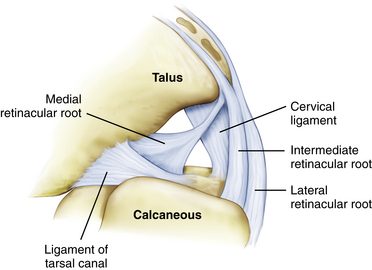
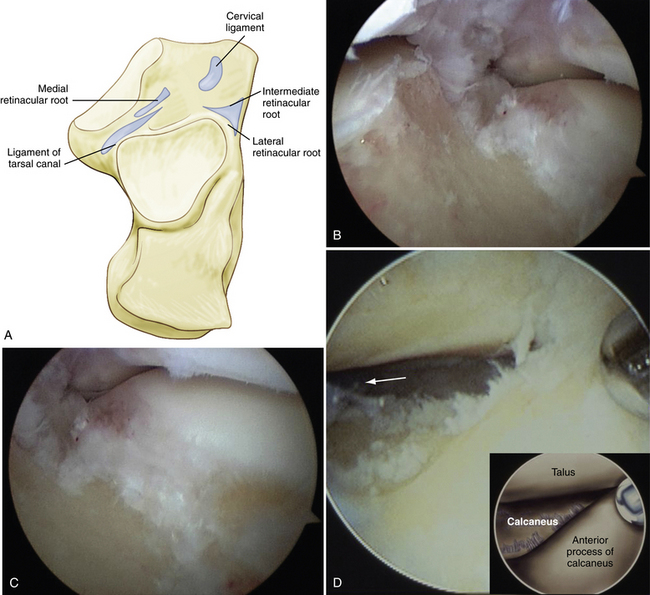
For arthroscopic purposes, the subtalar joint can be divided into anterior (talocalcaneonavicular) and posterior (talocalcaneal) articulations (Fig. 2-1).3–7 The anterior and posterior articulations are separated by the tarsal canal and the lateral opening of this canal, called the sinus tarsi, which is a soft, palpable area approximately 2 cm anterior to the tip of the lateral malleolus. The medial root of the inferior extensor retinaculum, the cervical and talocalcaneal interosseous ligaments, fatty tissue, and blood vessels are found within the sinus tarsi and tarsal canal. The ligaments that support the subtalar joint on the lateral side consist of a superficial, intermediate, and deep layer (Fig. 2-2). The superficial layer consists of the lateral talocalcaneal ligament, the posterior talocalcaneal ligament, the medial talocalcaneal ligament, the lateral root of the inferior extensor retinaculum, and the calcaneofibular ligament. The intermediate layer is formed by the intermediate root of the inferior extensor retinaculum and the cervical ligament. The deep layer consists of the medial root of the inferior extensor retinaculum and the interosseous ligament (Fig. 2-3).8–11
The talocalcaneonavicular joint, or anterior subtalar joint, is composed of the talus, the posterior surface of the tarsal navicular, the anterior surface of the calcaneus, and the plantar calcaneonavicular (spring) ligament. The anterior portion of the subtalar joint includes the anterior and middle articulating facets. Compared with the posterior joint, the anterior subtalar joint is more difficult to examine with the arthroscope because the thick ligaments that fill the sinus tarsi and tarsal canal may block the initial view. The anterior joint normally has no connection to the posterior joint because the thick interosseous ligament fills the tarsal canal and separates the two anatomic areas (Fig. 2-4).
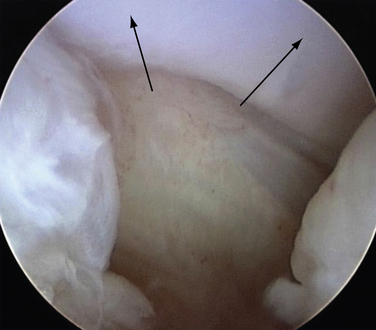
The posterior subtalar joint has a long axis oriented obliquely 40 degrees to the midline of the foot, facing laterally. It is a synovium-lined joint consisting of the convex posterior facet of the calcaneus and the concave posterior facet of the talus. The posterior subtalar joint consists of the posterior calcaneal facet of the undersurface of the talus and the posterior articular surface of the calcaneus. The joint capsule is reinforced on the lateral side by the lateral talocalcaneal ligament and the calcaneofibular ligament. The posterior joint has a posterior capsular pouch with small lateral, medial, and anterior recesses (Fig. 2-5).
ANATOMY OF PORTAL PLACEMENT AND SAFETY
Lateral Approach Anatomy
Arthroscopic evaluation of the subtalar joint has traditionally been performed using a lateral approach. Three portals are recommended for visualization and instrumentation of the subtalar joint using the lateral approach (Fig. 2-6). The anatomic landmarks for lateral portal placement include the lateral malleolus, the anterior process of the calcaneus, the sinus tarsi, and the Achilles tendon. The lateral malleolus and anterior process of the calcaneus are easy to palpate. The sinus tarsi is a palpable depression between the distal tip of the fibula and the anterior process of the calcaneus, although it can be filled with large amounts of adipose tissue. Inversion and eversion of the foot may be helpful in palpating the sinus tarsi.
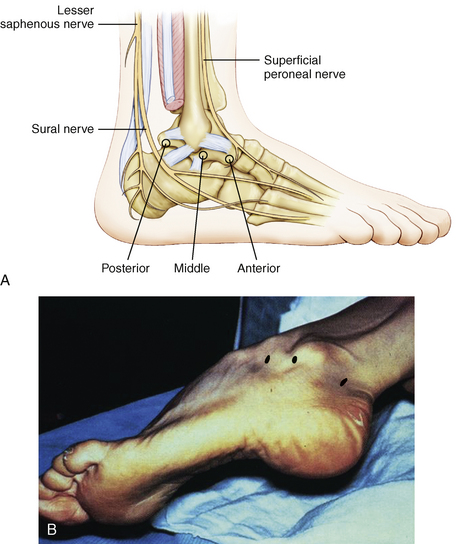
FIGURE 2-6 A, Three standard portals are used to approach the subtalar joint: anterior, middle, and posterior. B, Anatomic landmarks are used for placement of the lateral portals: the distal fibula, the anterior process of the calcaneus, and the sinus tarsi between the fibula and calcaneus. The patient is in the lateral decubitus position.
The point of entry for the anterior portal is usually about 2 cm anterior and 1 cm distal to the tip of the distal fibula, directing the instrument slightly upward and about 40 degrees posteriorly. The location of the portal in cadaveric dissection studies is an average of 28 mm (range, 23 to 35 mm) anterior to the tip of the fibula (Fig. 2-7).7
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree