CHAPTER 16 Glenohumeral Instability
It deserves to be known how a shoulder which is subject to frequent dislocations should be treated. For many persons owing to this accident have been obliged to abandon gymnastic exercises, though otherwise well qualified for them; and from the same misfortune have become inept in warlike practices, and have thus perished. And this subject deserves to be noticed, because I have never known any physician [to] treat the case properly; some abandon the attempt altogether, and others hold opinions and practice the very reverse of what is proper.
HISTORICAL REVIEW
Early Descriptions
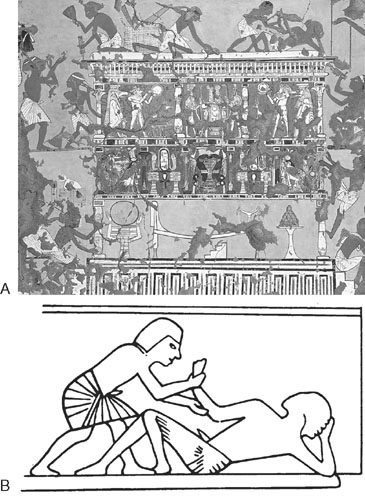
The first report of a shoulder dislocation is found in humankind’s oldest book, the Edwin Smith Papyrus (3000-2500 BCE).3 Hussein4 reported that in 1200 BCE in the tomb of Upuy, an artist and sculptor to Ramses II, there was a drawing of a scene that was strikingly similar to Kocher’s method of reduction (Fig. 16-1).
The most detailed early description of anterior dislocations came from the Father of Medicine, Hippocrates, who was born in 460 BCE on the island of Cos.5 Hippocrates described the anatomy of the shoulder, the types of dislocations, and the first surgical procedure. In one of his classic procedures for reduction, he stressed the need for suitably sized, leather-covered balls to be placed into the axilla, for without them the heel could not reach the head of the humerus in his reduction maneuver. Other Hippocratic techniques are described by Brockbank and Griffiths (Fig. 16-2).6
Hippocrates criticized his contemporaries for improper burning of the shoulder, a treatment popular at the time. In this first description of a surgical procedure for recurrent dislocation of the shoulder, he described how physicians had burned the top, anterior, and posterior aspects of the shoulder, which only caused scarring in those areas and promoted downward dislocation. He advocated the use of cautery in which an oblong, red-hot iron was inserted through the axilla to make eschars, but only in the lower part of the joint. Hippocrates displayed considerable knowledge of the anatomy of the shoulder, and he warned the surgeon to not let the iron come in contact with the major vessels and nerves because it would cause great harm. Following the burnings, he bound the arm to the side, day and night for a long time, “for thus more especially will cicatrization take place, and the wide space into which the humerus used to escape will become contracted.”32
Interested readers are referred to the text by Moseley,7 which has a particularly good section on the historical aspects of management of shoulder instability.
Humeral Head Defect
In 1861, Flower8 described the anatomic and pathologic changes found in 41 traumatically dislocated shoulders from specimens in London museums. He wrote that “where the head of the humerus rests upon the edge of the glenoid fossa absorption occurs, and a groove is evacuated, usually between the articular head and the greater tuberosity.”8 In 1880, Eve9 reported an autopsy of a patient who died 12 hours after an acute anterior dislocation in which he found a deep groove in the posterolateral aspect of the head. Joessel10 also observed the defect. According to Hill and Sachs,11 beginning in 1882, publications by Kuster,12 Cramer,13 Löbker,14 Schüller,15 Staffel,16 and Francke17 described the finding of a posterolateral defect in humeral heads resected for relief of chronic or recurrent dislocation.
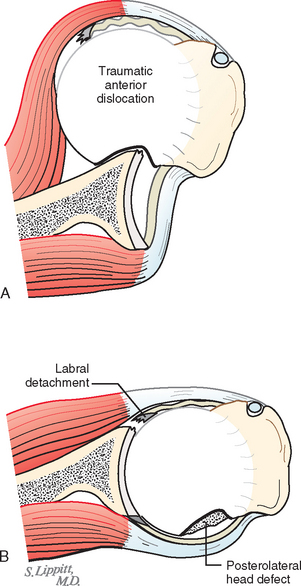
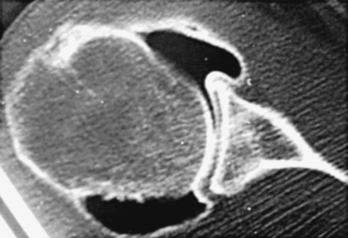
In 1887, Caird18 of Edinburgh concluded that a true subcoracoid dislocation must have an indentation fracture of the humeral head that is produced by the dense, hard anterior lip of the glenoid fossa. In cadaver experiments, he was able to produce the head defect. He said that the hard, dense glenoid lip would cut into the soft cancellous bone like a knife (Fig. 16-3).
Roentgen’s discovery of x-rays in 1895 ushered in new evaluations and studies of the anatomy of the anterior glenoid and humeral head defects. The first description of the radiographic changes in the humeral head associated with recurrent instability is attributed to Francke17 in 1898, only 3 years after Roentgen’s discovery.19 Hermodsson demonstrated that the posterolateral humeral head defect is the result of a compression fracture caused by the anterior glenoid rim following the exit of the humeral head from the glenoid fossa.19 He also observed that the defect is seen in the majority of cases; the longer the head is dislocated, the larger the defect will be; the defects are generally larger in anteroinferior dislocations than in anterior dislocations; and the defect is usually larger in recurrent anterior dislocations of the shoulder.
In 1925, Pilz20 reported the first detailed radiographic examination of recurrent dislocation of the shoulder and stated that routine radiographs were of little help. He stressed the need for an angled-beam projection to observe the defect. In 1940, Hill and Sachs11 published a very clear and concise review of the available information on the humeral head compression fracture defect that now carries their names.
Anterior Capsule and Muscle Defects
According to the Hunterian Lecture given by Reeves in 1967, Roger of Palermo in the 13th century taught that the lesion in an acute dislocation was a capsular rupture. Bankart,21 following the concepts of Broca and Hartmann,22 Perthes,1 Flower,8 and Caird,18 claimed that the essential lesion was detachment of the labrum and capsule from the anterior glenoid as a result of forward translation of the humeral head (referred to by subsequent authors as the Bankart lesion) (see Fig. 16-3). Later experimental and clinical work by Reeves23 and Townley24 suggested that other lesions might be responsible for recurrent dislocation, such as failure of the initial injury to incite a healing response, detachment of the subscapularis tendon, and variance in attachment of the inferior glenohumeral ligament.
Moseley and Overgaard25 found laxity in 25 consecutive cases, and DePalma and associates26 reported subscapularis laxity, rupture, and decreased muscle tone in 38 consecutive cases. Several of their cases and some from Hauser27 revealed a definite defect along the anterior or inferior aspect of the subscapularis tendon, as though it had been partially torn from its bone attachment, along with separation of the muscle fibers that insert into the humerus directly below the lesser tuberosity. McLaughlin,28 DePalma and associates,26 Jens,29 and Reeves30 have noted at the time of surgery before arthrotomy that with abduction and external rotation, the humeral head would dislocate under the lower edge of the subscapularis tendon. Symeonides31 took biopsy samples of the subscapularis muscle-tendon unit at the time of surgery and found microscopic evidence of “healed post-traumatic lesions.” He stated that instability results because traumatic lengthening of the subscapularis muscle leads to loss of the power necessary to stabilize the shoulder.
Rotator Cuff Injuries
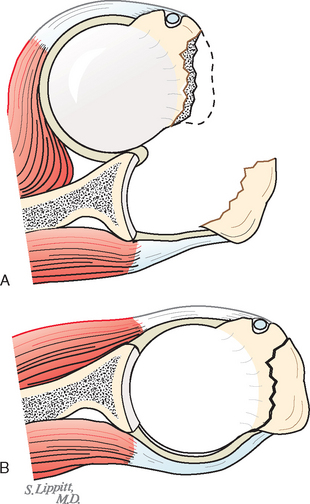
In 1880, Joessel10 reported on his careful postmortem studies of four cases of known recurrent dislocation of the shoulder. In all cases he found a rupture of the posterolateral portion of the rotator cuff from the greater tuberosity and a greatly increased shoulder joint capsule volume (Fig. 16-4). He also noted fractures of the humeral head and the anterior glenoid rim (Figs. 16-5 and 16-6). Joessel concluded that cuff disruptions that did not heal predisposed to recurrence of the problem, that recurrences were facilitated by the enlarged capsule, and that fractures of the glenoid or the head of the humerus resulted in a smaller articular surface, which can tend to produce recurrent dislocation. However, his four patients were elderly and might have had the degenerative cuff changes common in older people.
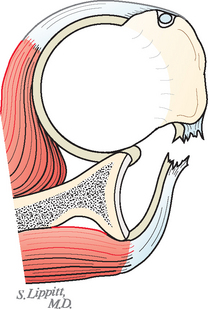
FIGURE 16-4 An anterior dislocation shown in an axillary projection with a tear in the posterior rotator cuff.
Treatment of Acute Traumatic Dislocations
Hippocrates32 discussed in detail at least six different techniques to reduce a dislocated shoulder. From century to century the literature has included woodcuts, drawings, and redrawings illustrating modifications of Hippocrates’ teachings by such investigators as Paré, de Cruce, Vidius, and Scultetus. Hippocrates’ original technique5 is still used on occasion. The stockinged foot of the physician is used as countertraction. The heel should not go into the axilla (i.e., between the anterior and posterior axillary folds) but should extend across the folds and against the chest wall. Traction should be slow and gentle; as with all traction techniques, the arm may be gently rotated internally and externally to disengage the head.
In 1870, Theodore Kocher,33 who won the Nobel Prize for medicine in 1909, gave a somewhat confusing report of his technique for levering in an anteriorly dislocated shoulder. Had Kocher not been so famous as a thyroid surgeon, his article might have received only scant attention. In the Kocher technique, the humeral head is levered on the anterior glenoid and the shaft is levered against the anterior thoracic wall until the reduction is completed.
In 1938, Milch34 described a technique for reduction in the supine position whereby the arm is abducted and externally rotated and the thumb is used to gently push the head of the humerus back into place. Lacey35 modified the technique by performing the maneuver with the patient prone on an examining table. Russell and associates36 reported on the ease and success of this technique.
DePalma37 warned that with the Kocher technique, undue forces used in rotation leverage can damage the soft tissues of the shoulder joint, the vessels, and the brachial plexus. Beattie and coworkers38 reported a fracture of the humeral neck during a Kocher procedure. Other authors have described spiral fractures of the upper shaft of the humerus and further damage to the anterior capsular mechanism when the Kocher leverage technique of reduction was used. McMurray39 reported that of 64 dislocations reduced by the Kocher method, 40% became recurrent, whereas of 112 dislocations reduced by gently lifting the head into place, only 12% became recurrent.
Since 1975, numerous articles have described simple techniques to reduce a dislocated shoulder: the forward elevation maneuver,40,41 the external rotation method,42,43 scapular manipulation,44 the modified gravity method,45 the crutch and chair technique,46 the chair and pillow technique,47 and others.48,49
Operative Reconstructions for Anterior Instability
Most of the published literature on shoulder dislocations is concerned with the problem of recurrent anterior dislocations. As mentioned previously, Hippocrates32 described the use of a white-hot poker to scar the anteroinferior part of the capsule. Since then, hundreds of operative procedures have been described for the management of recurrent anterior dislocations. Readers who have a yearning for the detailed history should read the classic texts by Moseley7 and Hermodsson.19
Various operative techniques have been based on the posterolateral defect and soft tissue disruptions on the front of the shoulder. Bardenheuer50 in 1886 and Thomas51,52 in 1909 and 1921 discussed capsular plication or shrinking. In 1898, Albert53 performed arthrodesis, and in 1902, Hildebrand54 deepened the glenoid socket.
In 1906, Perthes1 wrote a classic paper on the operative treatment of recurrent dislocations. He stated that the operation should be directed at repairing the underlying lesion (i.e., repair of the capsule, the glenoid labrum detachment from the anterior bony rim, and the rotator cuff tear). He repaired the capsule with suture to the anterior glenoid rim through drill holes, and in several cases he used staples to repair the anterior capsular structures. This report gave the first description of repair of the anterior labrum and capsule to the anterior glenoid rim. Two patients were monitored for 17 years, one for 12 years, two for 3 years, and one for 1 year and 9 months. All had excellent function with no recurrence.
The muscle sling myoplasty operation was used in 1909 by Clairmont and Ehrlich.55 The posterior third of the deltoid, with its innervation left intact, was removed from its insertion on the humerus, passed through the quadrilateral space, and sutured to the coracoid process. When the arm was abducted, the deltoid contracted, which held up the humeral head. Finsterer,56 in a similar but reversed procedure, used the coracobrachialis and the short head of the biceps from the coracoid and transferred them posteriorly. Both operations failed, with high recurrence rates.
In 1923, Bankart21 first published his operative technique and noted that only two classes of operations were used at that time for recurrent dislocation of the shoulder: those designed to decrease the size of the capsule by plication or pleating51,52 and those designed to give inferior support to the capsule.55,57 Bankart condemned both in preference to his procedure. He stated that the essential lesion was detachment or rupture of the capsule from the glenoid ligament. He recommended repair with interrupted sutures of silkworm gut passed between the free edge of the capsule and the glenoid ligament. At that time he did not repair the lateral capsule to the bone of the anterior glenoid rim.
In his 1939 article, Bankart2 described the essential lesion as “detachment of the glenoid ligament from the anterior margin of the glenoid cavity” and stated, “the only rational treatment is to reattach the glenoid ligament (or the capsule) to the bone from which it has been torn.” He further wrote that “the glenoid ligament may be found lying loose either on the head of the humerus or the margin of the glenoid cavity.” He recommended repair of the lateral capsule down to the raw bone of the anterior glenoid and that it be held in place with suture through drill holes made in the anterior glenoid rim with sharp, pointed forceps. Although no references were listed in either article, Bankart must have been greatly influenced by the previously published work of Broca and Hartmann22 and particularly that of Perthes,1 which described virtually identical pathology and repair.
Beginning in 1929, Nicola58–62 published a series of articles on management of recurrent dislocation of the shoulder. He used the long head of the biceps tendon and the coracohumeral ligament as a suspension checkrein to the front of the shoulder. Henderson63,64 described another checkrein operation that looped half the peroneus longus tendon through drill holes in the acromion and the greater tuberosity. In 1927, Gallie and LeMesurier65 described the use of autogenous fascia lata suture in treating recurrent dislocation of the shoulder. This procedure has been modified by Bateman.66
Posterior Glenohumeral Instability
In 1839 in a Guy’s Hospital report,67 Sir Astley Cooper described in detail a dislocation of the os humeri on the dorsum scapulae. This report is a classic, for Cooper presented most of the characteristics associated with posterior dislocations: the dislocation occurred during an epileptic seizure; the pain was greater than with the usual anterior dislocation; external rotation of the arm was entirely impeded, and the patient could not elevate his arm from his side; the shoulder had an anterior void or flatness and a posterior fullness; and the patient was “unable to use or move his arm to any extent.” In this report of a case in which Cooper had acted as a consultant, reduction could not be accomplished and the patient never recovered the use of his shoulder. Postmortem examination of the shoulder, performed 7 years later, revealed that the subscapularis tendon was detached and the infraspinatus muscles were stretched posteriorly about the head of the humerus. The report suggested that the detached subscapularis was “the cause of the symptoms.” Cooper further described resorption of the anterior aspect of the humeral head where it was in contact with the posterior glenoid, probably the first description of the reverse Hill–Sachs lesion.
Another classic article on the subject was published in 1855 by Malgaigne,68 who reported on 37 cases of posterior dislocation of the shoulder; 3 cases were his own and 34 were reviewed from the literature. This series of cases was collected 40 years before the discovery of x-rays, and it points out that with adequate physical examination of the patient, the correct diagnosis can be made.
RELEVANT ANATOMY
Skin
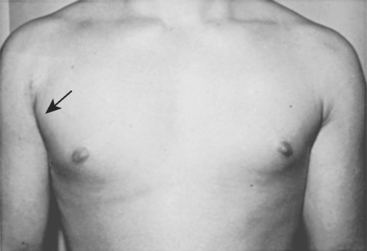
Shoulder stabilization surgery can usually be accomplished through cosmetically acceptable incisions in the lines of the skin (see Chapter 2). Anteriorly, the surgeon can identify and mark the prominent anterior axillary crease by adducting the shoulder. An incision placed in the lower part of this crease provides excellent access to the shoulder for anterior repair and yet heals nicely with subcuticular closure (Figs. 16-7 and 16-8). When cosmesis is a concern, the incision can be made more into the axilla, as described by Leslie and Ryan.69
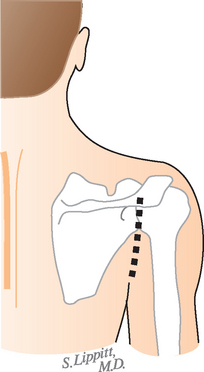
Posteriorly, an analogous vertical incision in line with the extended posterior axillary crease (best visualized by extending the shoulder backward) also heals well (Fig. 16-9). Fortuitously, these creases lie directly over the joint to which the surgeon needs access.
First Muscle Layer
The shoulder is covered by the deltoid muscle arising from the clavicle, acromion, and scapular spine. The anterior deltoid extends to a line running approximately from the midclavicle to the midlateral portion of the humerus. This line passes over the cephalic vein, the anterior venous drainage of the deltoid, and the coracoid process. The deltoid is innervated by the axillary nerve, whose branches swoop upward as they extend anteriorly (Fig. 16-10). The commonly described safe zone 5 cm distal to the acromion does not take into account these anterior branches, which can come as close as 2 cm to the acromion.
At the deltopectoral groove, the deltoid meets the clavicular head of the pectoralis major, which assists the anterior deltoid in forward flexion. The medial and lateral pectoral nerves are not in the surgical field of shoulder stabilization. Splitting the deltopectoral interval just medial to the cephalic vein preserves the deltoid’s venous drainage and takes the surgeon to the next layer. Extension of the shoulder tightens the pectoralis major and the anterior deltoid, as well as the coracoid muscles, and thus compromises the exposure. Accordingly, surgical assistants must be reminded to hold the shoulder in slight flexion to relax these muscles and facilitate access to the joint.
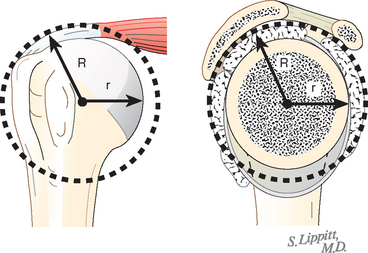
The Coracoacromial Arch and Clavipectoral Fascia
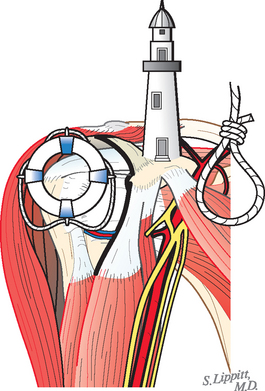
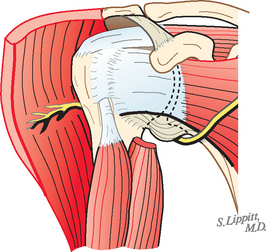
The coracoacromial arch provides a concavity that articulates with the proximal humeral convexity (Figs. 16-11 to 16-13). The center of this articulation is identical to the center of the glenohumeral articulation in the normal shoulder. The radii of these two articulations differ by the thickness of the rotator cuff and tuberosity. The concentricity of the coracoacromial and glenohumeral spheres provides stable centering of the normal shoulder through an extremely wide range of positions.
The coracoid process is the lighthouse of the anterior aspect of the shoulder in that it provides a palpable guide to the deltopectoral groove, a locator for the coracoacromial arch, and an anchor for the coracoid muscles (the coracobrachialis and short head of the biceps) that separate the lateral “safe side” from the medial “suicide” where the brachial plexus and major vessels lie (Fig. 16-14). The surgeon comes to full appreciation of the value of such a lighthouse when it is lacking—for example, when re-exploring a shoulder for complications of a coracoid transfer procedure. The clavipectoral fascia covers the floor of the deltopectoral groove. Rotating the humerus enables the surgeon to identify the subscapularis moving beneath this fascial layer. Incising the fascia up to but not through the coracoacromial ligament preserves the stabilizing function of the coracoacromial arch.
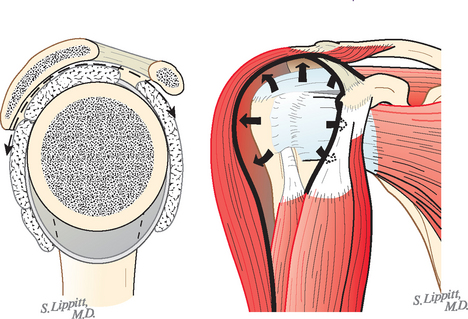
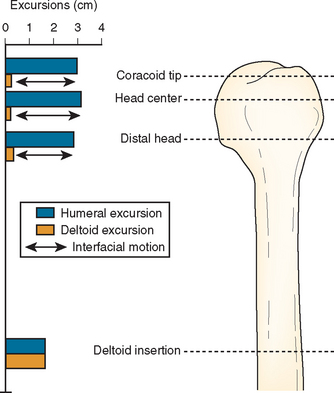
The Humeroscapular Motion Interface
The humeroscapular motion interface (Fig. 16-15) separates the structures that do not move on humeral rotation (the deltoid, coracoid muscles, acromion, and coracoacromial ligament) from those that do (the rotator cuff, long head of the biceps tendon, and humeral tuberosities). During shoulder motion, substantial gliding takes place at this interface (Fig. 16-16). The humeroscapular motion interface provides a convenient plane for medial and lateral retractors and is also the plane in which the principal nerves lie.
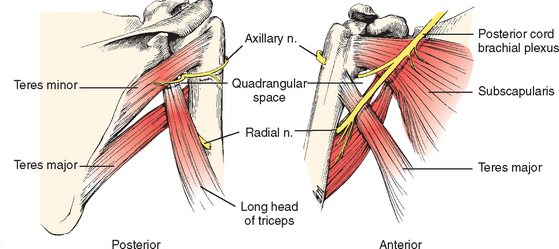
The axillary nerve runs in the humeroscapular motion interface, superficial to the humerus and cuff and deep to the deltoid and coracoid muscles (Fig. 16-17; see also Fig. 16-10). Sweeping a finger in a superior-to-inferior direction along the anterior aspect of the subscapularis muscle catches the axillary nerve, which hangs like a watch chain across the muscle belly. Tracing this nerve proximally and medially leads the finger to the bulk of the brachial plexus. Tracing it laterally and posteriorly leads the finger beneath the shoulder capsule toward the quadrangular space. From a posterior vantage, the axil lary nerve is seen to exit the quadrangular space beneath the teres minor and extend laterally, where it is applied to the deep surface of the deltoid muscle. By virtue of its prominent location in close proximity to the shoulder joint anteriorly, inferiorly, and posteriorly, the axillary nerve is the most commonly injured structure in shoulder surgery.
The musculocutaneous nerve lies on the deep surface of the coracoid muscles and penetrates the coracobrachialis with one or more branches lying a variable distance distal to the coracoid. (The often-described 5-cm safe zone for the nerve beneath the process refers only to the average position of the main trunk and not to an area that can be entered recklessly.) The musculocutane ous nerve is vulnerable to injury from retractors placed under the coracoid muscles and to traction injury during coracoid transfer. Knowledge of the position of these nerves can make the shoulder surgeon both more comfortable and more effective.
The Rotator Cuff
The next layer of the shoulder is the rotator cuff. The tendons of these muscles blend in with the capsule as they insert into the humeral tuberosities.70 Thus, in reconstructions that require splitting of these muscles from the capsule, such splitting is more easily accomplished medially, before the blending becomes complete. The nerves to these muscles run on their deep surfaces: the upper and lower subscapular to the subscapularis and the suprascapular to the supraspinatus and infraspinatus. Medial dissection on the deep surface of these muscles can jeopardize their nerve supply.71 The superior portion of the subscapularis tendon has been found to have significantly higher stiffness and ultimate load than its inferior portion has.72
The tendon of the long head of the biceps originates from the supraglenoid tubercle (Figs. 16-18 and 16-19). It runs beneath the cuff in the area of the rotator interval and exits the shoulder beneath the transverse humeral ligament and between the greater and lesser tuberosities. It is subject to injury when incising the upper subscapularis from the lesser tuberosity. In the bicipital groove of the humerus, this tendon is endangered by procedures that involve lateral transfer of the subscapularis tendon across the groove.
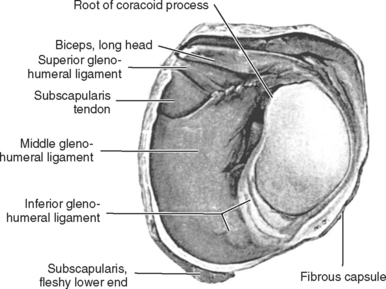
The Scapulohumeral Ligaments
Though often suggested as the primary stabilizers of the glenohumeral joint, the scapulohumeral ligaments are now recognized to play a primary role only in positions near the extremes of the allowed range of motion. The thickness of the capsule decreases as it nears the humerus. The capsule is thickest in the inferior pouch at 2.8 mm, 2.4 mm in its anterior portion, and 2.2 mm in the posterior portion. The thickness ranges from 1.3 to 4.5 mm in cadaveric specimens.73 The glenohumeral joint capsule is normally large, loose, and redundant, which allows full and free range of motion of the shoulder. By virtue of their mandatory redundancy, the capsule and its ligaments are lax throughout most of the range of joint motion. Thus, they can exert major stabilizing effects only when they come under tension as the joint approaches the limits of its range of motion. In the midrange of shoulder motion, the center of the humeral head remains within 2.2 mm of the center of the glenoid on magnetic resonance imaging (MRI).74 This limited stabilizing effect shows the importance of mechanisms of glenohumeral stability other than the capsule and its ligaments. The capsular structures are also believed to contribute to stability through their proprioceptive functions.75
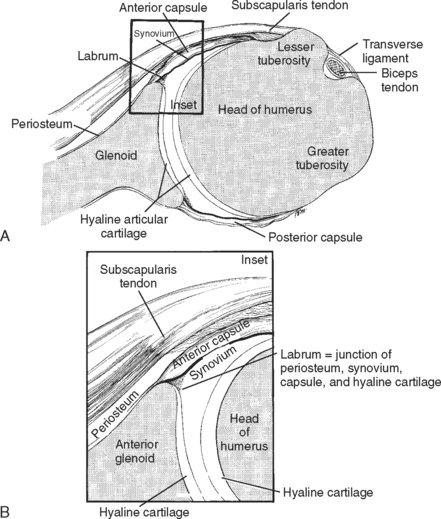
The three anterior glenohumeral ligaments were first described by Schlemm in 1853.76 Since then, many observers have described their anatomy and role in limiting glenohumeral rotation and translation (see Figs. 16-18 and 16-19).23,25,28,77–81
Codman82 and others pointed out the variability of the ligaments (see Fig. 16-19).25,37,77,79,83,84 These authors also demonstrated great variation in the size and number of synovial recesses that form in the anterior capsule above, below, and between the glenohumeral ligaments. They observed that if the capsule arises at the labrum, few if any synovial recesses are present (in this situation, because of generalized blending of all three ligaments, no room is left for synovial recesses or weaknesses, and hence the anterior glenohumeral capsule is stronger). However, the more medially the capsule arises from the glenoid (i.e., from the anterior scapular neck), the larger and more numerous the synovial recesses are. The end result is a thin, weak anterior capsule. In an embryologic study involving 52 specimens, Uhthoff and Piscopo85 demonstrated that the anterior capsule inserted into the glenoid labrum in 77% and into the medial neck of the scapula in 23%. This variation in anatomy was later classified into two different types, I and II. A type I attachment occurs when the fibers primarily originate from the labrum, with some fibers attaching to the glenoid, and it is seen 80% of the time. A type II origin of the capsuloligamentous structures occurs solely from the glenoid neck and is seen in 20% of cadaveric specimens.86
The superior glenohumeral ligament (SGHL) is identified as the most consistent capsular ligament.87 It crosses the rotator interval capsule and lies between the supraspinatus and subscapularis tendons. Another interval capsular structure, the coracohumeral ligament, originates at the base of the coracoid, blends into the cuff tendons, and inserts into the greater and lesser tuberosities.88–93
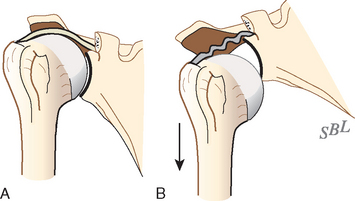
Harryman and colleagues pointed out that these two ligaments and the rotator interval capsule come under tension with glenohumeral flexion, extension, external rotation, and adduction.89 When they are under tension, these structures resist posterior and inferior displacement of the humeral head. Clinical and experimental data have shown that releasing or surgically tightening the rotator interval capsule increases or decreases the allowed posterior and inferior translational laxity, respectively.89,94–97
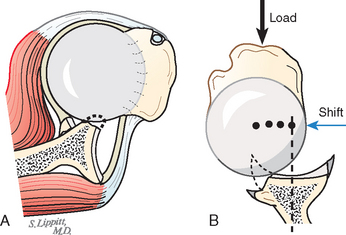
It is these ligaments and capsule, as well as the inferior glenoid lip, that provide static restraint against inferior translation.94 It is of anatomic interest and clinical significance that when the lateral aspect of the scapula is allowed to droop inferiorly, the resulting passive abduction of the humerus relaxes the rotator interval capsule and the superior ligaments; as a result, the humeral head can be dumped out of the glenoid fossa (Fig. 16-20).98 Drooping of the lateral part of the scapula is normally prevented by the postural action of the scapular stabilizers, particularly the trapezius and serratus. Elevation of the lateral aspect of the scapula with the arm at the side enhances inferior stability in two ways: the resulting glenohumeral adduction tightens the superior capsule and ligaments, and the scapular rotation places more of the inferior glenoid lip beneath the humeral head.97,99
The SGHL and coracohumeral ligament come under tension with external rotation in adduction, whereas the middle glenohumeral ligament (MGHL) is tensioned by external rotation when the humerus is abducted to 45 degrees.31,100,101 The MGHL originates anterosuperiorly on the glenoid and inserts midway along the anterior humeral articular surface adjacent to the lesser tuberosity. In more than a third of shoulders, the MGHL is absent or poorly defined, a situation that can place the shoulder at greater risk for anterior glenohumeral instability.102
With greater degrees of shoulder abduction, for example, in the apprehension position, the inferior glenohumeral ligament (IGHL) and the inferior capsular sling come into play.100,101 The IGHL originates below the sigmoid notch and courses obliquely between the anteroinferior glenoid and its humeral capsular insertion.83 O’Brien and coworkers have described an anterior thickening of the IGHL, the anterior superior band.83 The anterior and posterior aspects of the IGHL are said to function as a cruciate construct in which they alternately tighten in external and internal rotation.83,97,103 These ligaments can be stretched out with repeated use. The dominant shoulders of handball athletes were placed in 90 degrees of abduction and external rotation and then brought into extension while being observed in a computed tomography (CT) scanner. The dominant shoulders were seen to have more external rotation of the humeral head and more of a shift from the posterior aspect of the glenoid to its center than noted in normal shoulders when brought into the late cocking position.104
When the humerus is elevated anteriorly in the sagittal plane (flexion), the posterior-inferior capsular pouch and the rotator interval capsule come into tension.83,89,97,105,106 If the humerus is internally rotated while elevated in the sagittal plane, the interval capsule slackens but the posterior inferior pouch tightens. Posteroinferior capsular tension also limits flexion, internal rotation, and horizontal adduction.89,105,106 Excessive tightness of this portion of the capsule is a well-recognized clinical entity (see Chapter 17 on the rotator cuff).
Coracoacromial Ligament
Resection of the coracoacromial ligament in cadaveric shoulders was found to result in significantly greater anterior translation of the humeral head with the shoulder in 0 and 30 degrees of abduction. At 0 degrees of abduction, significantly greater inferior translation occurred after resection of the coracoacromial ligament.107 This observation should encourage caution with needless resection of the ligament.
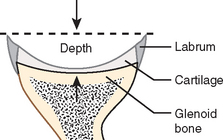
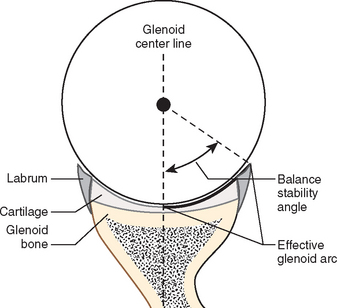
Glenoid Concavity and Labrum
The predominant method for centering the humeral head in the glenoid fossa is concavity compression.108 The glenoid concavity provides the essential concavity (see Figs. 16-18 and 16-19). The deeper the concavity, the more stability results from compression of the humeral head in it (Fig. 16-21). The glenoid concavity is provided by the shape of the bony socket, which is functionally deepened by the fact that the articular cartilage at the periphery is thicker than at the center (Fig. 16-22). Weldon and colleagues109 showed that removal of the glenoid cartilage dramatically compromised the intrinsic stability offered by the glenoid fossa, especially in the posterior-inferior direction, where the balance stability angle was reduced almost 50% by cartilage removal.
The socket is further deepened by the presence of the labrum around the rim of the socket (Fig. 16-23). The glenoid labrum is a fibrous rim that serves to deepen the glenoid fossa and allow attachment of the glenohumeral ligaments and the biceps tendon to the glenoid. Anatomically, it is the interconnection of the periosteum of the glenoid, the glenoid bone, the glenoid articular cartilage, the synovium, and the capsule. Although microscopic studies have shown that a small amount of fibrocartilage is located at the junction of the hyaline cartilage of the glenoid and the fibrous capsule, the vast majority of the labrum consists of dense fibrous tissue with a few elastic fibers (Fig. 16-24).24,25,110 The posterosuperior portion of the labrum is continuous with the tendon of the long head of the biceps. Anteriorly, it is continuous with the IGHL (see Fig. 16-19).111–114 Hertz and colleagues115 detailed the microanatomy of the labrum, and Prodromos and associates,116 DePalma,37 and Olsson117 described changes in the glenoid labrum with age.
In cadavers, isolated labral lesions are not usually sufficient to allow complete glenohumeral dislocation.24,30,118,119 However, cadaveric studies have shown diminished stability with labral lesions. Fehringer and colleagues have demonstrated that a simple incision in its attachment to the glenoid uncenters the humeral head.120 Resection of the labrum was found to decrease the stability ratio of cadaveric shoulders by 9.6%.121 Lazarus and coworkers122 demonstrated that resection of the cartilage and labrum from the anteroinferior glenoid reduced the height of the glenoid by approximately 80% and the stability ratio by approximately 65% for translation in the direction of the defect. Halder and colleagues121 again demonstrated the stabilizing effect of the labrum in a cadaver model.
Clinical studies reveal a high incidence of labral deficiency in patients with recurrent traumatic instability.2,123–127 In our experience, it is rare to see a shoulder with recurrent anterior traumatic instability without a detachment of the glenoid labrum from the glenoid lip.
For a review of the gross anatomy of the glenohumeral joint surfaces, ligaments, labrum, and capsule, see Chapter 2.
MECHANICS OF GLENOHUMERAL STABILITY
The most remarkable feature of the glenohumeral joint is its ability to precisely stabilize the humeral head in the center of the glenoid on the one hand and to allow a vast range of motion on the other. This balance of stability and mobility is achieved by a combination of mechanisms particular to this articulation.128
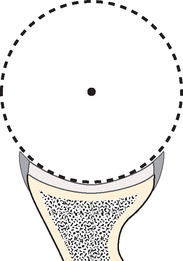
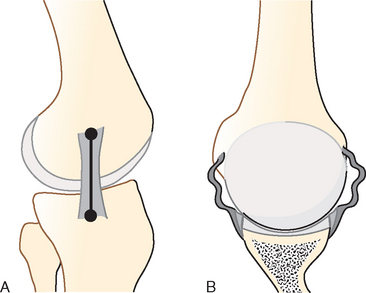
In contrast to the hip joint, the glenohumeral joint does not offer a deep stabilizing socket. An acetabulum-like socket would limit motion by contact of the anatomic neck of the humerus with its rim. Instead, the small arc of the glenoid captures relatively little of the humeral articular surface, thus neck-to-rim contact is avoided for a wide range of positions (Fig. 16-25).98,101,129–131
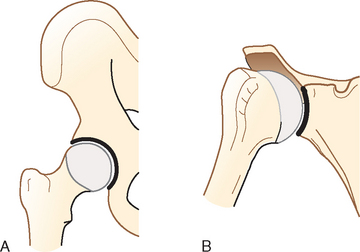
FIGURE 16-25 In contrast to the hip (A), the shallow glenoid captures relatively little of the articulating ball (B).
(From Matsen FA III, Lippitt SB, Sidles JA, Harryman DT II: Practical Evaluation and Management of the Shoulder. Philadelphia: WB Saunders, 1994.)
In contrast to hinge-like joints with shallow sockets, such as the knee, interphalangeal joints, elbow, and ankle, the glenohumeral joint does not offer isometric articular ligaments that provide stability as the joint is flexed around a defined anatomic axis. Instead, the glenohumeral ligaments play important stabilizing roles only at the extremes of motion; they are lax and relatively ineffectual in most functional positions of the joint (Fig. 16-26).97,98
In spite of its lack of a deep socket or isometric ligaments, the normal shoulder precisely constrains the humeral head to the center of the glenoid cavity throughout most of the arc of movement.74,131–135 It is remarkable that this seemingly unconstrained joint can provide such precise centering, resist the gravitational pull on the arm hanging at the side for long periods, remain located during sleep, allow the lifting of large loads, permit throwing a baseball at speeds exceeding 100 miles per hour, and maintain stability during the application of an almost infinite variety of forces of differing magnitude, direction, duration, and abruptness.
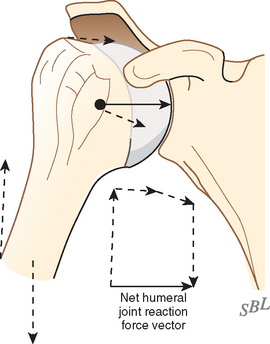
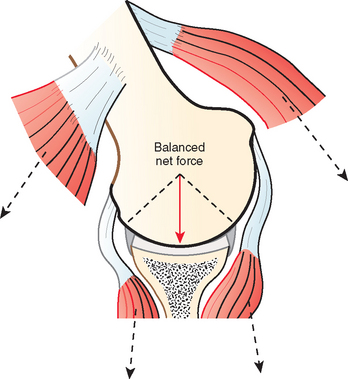
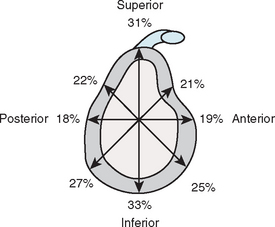
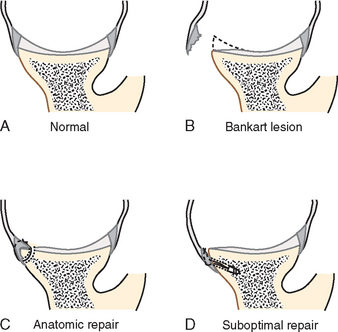
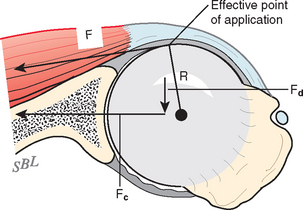
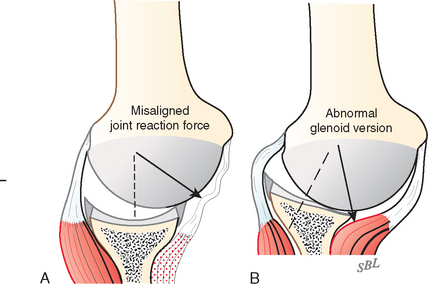
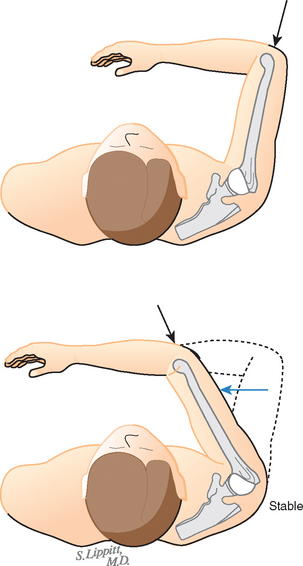
The basic law of glenohumeral stability is that the glenohumeral joint will not dislocate as long as the net humeral joint reaction force* (Fig. 16-27) is directed within the effective glenoid arc† (Figs. 16-28 and 16-29).132,136 If the net humeral joint reaction force passes outside the effective glenoid arc, the joint becomes unstable. The effective glenoid arc in a given direction is also known as the balance stability angle, the maximal angle that the net humeral joint reaction force can make with the glenoid center line in a given direction before dislocation (see Fig. 16-28). Balance stability angles vary for different directions around the glenoid (Fig. 16-30). The requisite for a stable glenohumeral joint is that the net humeral joint reaction force be maintained within the balance stability angles. The balance stability angle may be compromised by congenital deficiency (glenoid hypoplasia), excessive compliance, traumatic lesions (rim fractures or Bankart defects), or wear (Fig. 16-31).10,53,98,121,125,126,132,137–145 The balance stability angle may be restored or augmented by anatomic repair of fractures or Bankart lesions (Fig. 16-32), by rim augmentation,146 by congruent glenoid bone grafting,147 and by glenoid osteotomy.122
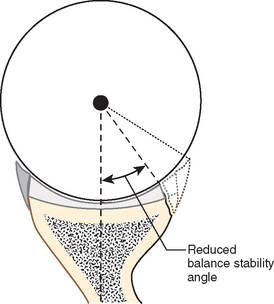
FIGURE 16-31 The balance stability angle and the effective glenoid arc are reduced by a fracture of the glenoid rim.
(Modified from Matsen FA III, Lippitt SB, Sidles JA, Harryman DT II: Practical Evaluation and Management of the Shoulder. Philadelphia: WB Saunders, 1994.)
The Net Humeral Joint Reaction Force
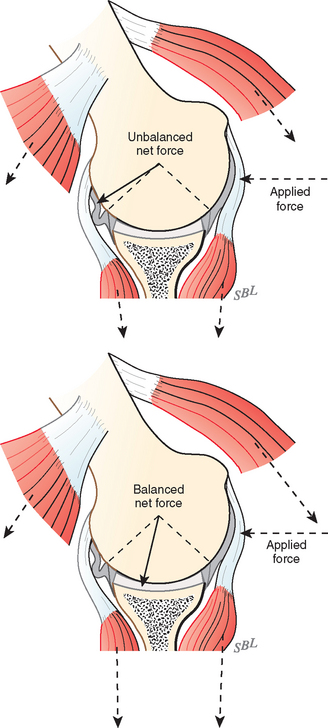
The direction of the net humeral joint reaction force is controlled actively by elements of the rotator cuff and other shoulder muscles along with the weight of the arm and externally applied forces. Each active muscle generates a force whose direction is determined by the effective origin and insertion of that muscle (Fig. 16-33). Neural control of the magnitude of these muscle forces provides the mechanism by which the direction of the net humeral joint reaction force is controlled. For example, by increasing the force of contraction of muscles whose force directions are close to the glenoid center line, the direction of the net humeral joint reaction force can be aligned more closely with the glenoid fossa (Fig. 16-34). The elements of the rotator cuff are well positioned to contribute to this muscle balance.118,148–162
In addition to the compression provided by the rotator cuff musculature, the deltoid assists in this capacity as well. The middle and posterior portions of the deltoid have been shown to be more important than the anterior portion in producing concavity compression.163,164 The long head of the biceps muscle might also contribute to shoulder stability.165
In the healthy shoulder, strengthening and neuromuscular training help optimize neuromuscular control of the net humeral joint reaction force. Conversely, the net humeral joint reaction force is difficult to optimize when muscle control is impaired by injury, disuse, contracture, paralysis, loss of coordination, or tendon defects or when the glenoid concavity is compromised (Fig. 16-35). Neuromuscular training may be guided by proprio- ceptors in the labrum and ligaments.166–169 Blasier and coworkers170 and Kronberg and colleagues171 showed that persons with generalized joint laxity have less-acute proprioception and altered muscle activation. Zuckerman and associates demonstrated that motion and position sense are compromised in the presence of traumatic anterior instability and are restored 1 year after surgical reconstruction.172
The reader is referred to reviews of neuromuscular stabilization of the shoulder by Lieber and Friden128 (Ch 4) and by Speer and Garrett.128 (Ch 8) In the same reference are found reviews of the role of capsular feedback and pattern generators in shoulder kinematics by Grigg128(Ch 9) and the role of muscle optimization by Flanders.128 (Ch 39)
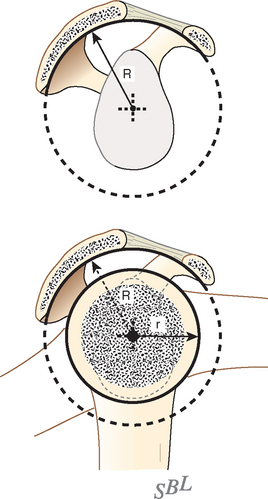
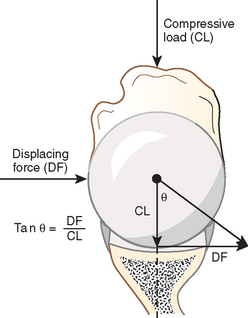
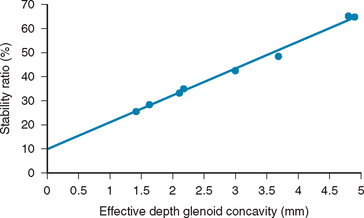
The Balance Stability Angle and the Stability Ratio
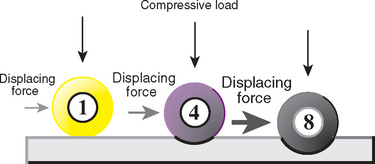
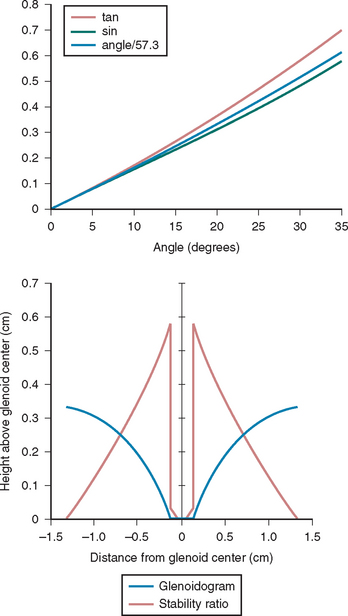
The balance stability angle is the maximal angle that the net humeral joint reaction force can make with the glenoid center line before glenohumeral dislocation occurs. The tangent of this balance stability angle is the ratio between its displacing component (perpendicular to the glenoid center line) and its compressive component (parallel to the glenoid center line), which is known as the stability ratio (Fig. 16-36). The stability ratio is the maximal displacing force in a given direction that can be stabilized by a specified compressive load, assuming frictional effects to be minimal.* The effective glenoid arc, the balance stability angle, and stability ratios vary around the perimeter of the glenoid (see Fig. 16-30). It is handy to note that for small angles, the stability ratio can be estimated by dividing the balance stability angle by 57 degrees (Fig. 16-37).*
The stability ratio is often used in the laboratory because it is relatively easy to measure: A compressive load is applied, and the displacing force is progressively increased until dislocation occurs. For example, Lippitt and colleagues137 found that a compressive load of 50 N resisted displacing loads of up to 30 N and that the effectiveness of this stabilization mechanism varied with the depth of the glenoid (Fig. 16-38). Investigation of these parameters provides important information on stability mechanics; for example, resection of the labrum has been shown to reduce the stability ratio by 20%.137 Furthermore, a 3-mm anterior glenoid defect has been shown to reduce the balance stability angle more than 25% from 18 to 13 degrees.98 Bony defects of 21% of the anterior glenoid rim were noted to reduce the balance stability angle by 50%.147,173
Clinically, the stability ratio can be sensed by using the load and shift test, wherein the examiner applies a compressive load pressing the humeral head into the glenoid while noting the amount of translating force necessary to move the humeral head from its centered position.174 This test gives the examiner an indication of the adequacy of the glenoid concavity and is one of the most practical ways to detect deficiencies of the glenoid rim.
The Glenoidogram
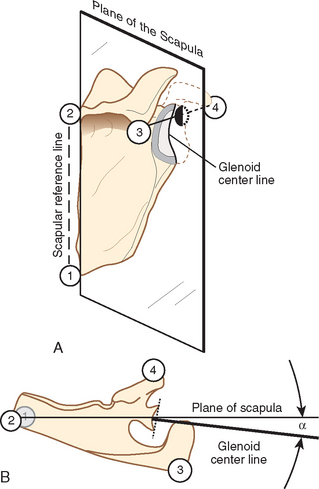
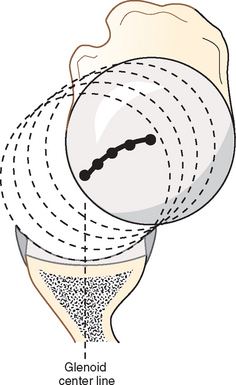
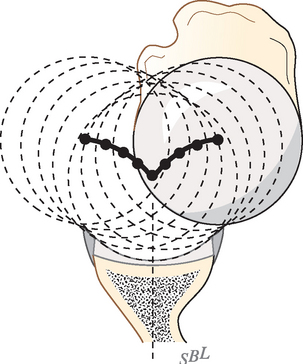
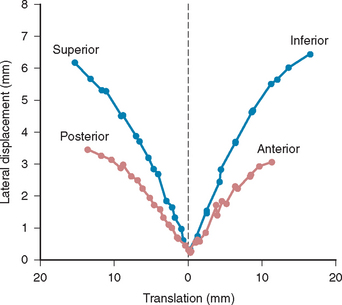
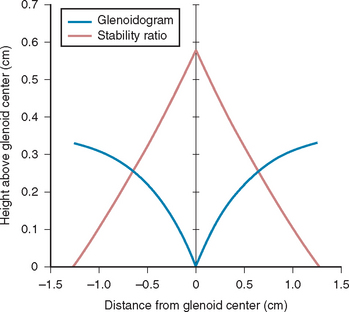
The effective shape of the glenoid is revealed by the glenoidogram, which, rather than showing how the glenoid looks, shows how it works.122,125 The glenoidogram is the path taken by the center of the humeral head as it is translated away from the center of the glenoid fossa in a specified direction. The shape of the glenoidogram indicates the extent of the effective glenoid arc in that direction. The glenoidogram is oriented with respect to the glenoid center line, a reference line perpendicular to the center of the glenoid fossa (Figs. 16-39 and 16-40). As the humeral head is translated from the center of the glenoid to the rim in a given direction, the center of the humeral head traces the glenoidogram, which has a characteristic gullwing shape (Figs. 16-41 and 16-42). The glenoidogram is different for different directions of translation (Fig. 16-43) and presents data recorded for the superior, inferior, anterior, and posterior directions in a typical shoulder.
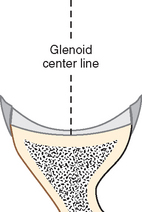
FIGURE 16-39 The glenoid center line is a line perpendicular to the surface of the glenoid fossa at its midpoint.
(Modified from Matsen FA III, Lippitt SB, Sidles JA, Harryman DT II: Practical Evaluation and Management of the Shoulder. Philadelphia: WB Saunders, 1994.)
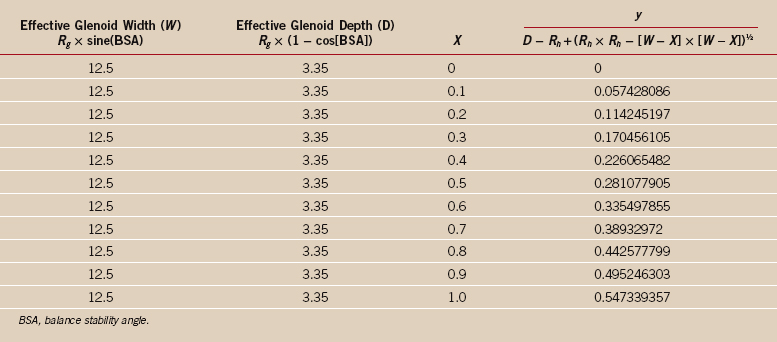
D – Rh + (Rh × Rh − [w − x] × [w − x])½
The sample spreadsheet (Table 16-1) displays the case in which R g = Rh = 25 mm and the BSA = 30 degrees = 0.5236 radians. In this case, the effective glenoid width (W) = Rg × sin(BSA), and the effective glenoid depth (D) = Rg × (1 − cos[BSA]). The results of this prediction are shown in Table 16-1 and Fig. 16-44.
Predicted glenoidograms are qualitatively similar to glenoidograms measured experimentally (compare Figs. 16-43 and 16-44). The glenoidogram also reveals another important aspect of shoulder stability: The slope of the glenoidogram at any point is equal to the stability ratio at that point. For most glenoidograms it can be seen that the stability ratio is maximal when the humeral head is centered in the glenoid (see Fig. 16-44). Thus, the joint has the highly desirable property of being most stable when the head is centered. As the humeral head is moved away from the center, the slope of the glenoidogram and the stability ratio become less. Accordingly, as the head is displaced from the glenoid center, it becomes progressively more unstable. Once enough force is applied to displace the head from the center, that same amount of force easily displaces the humeral head over the glenoid lip. When the humeral head is translated to the lip of the glenoid, the stability ratio is, as expected, zero. These observations are consistent with the clinical jerk tests described for anterior175 and posterior89 instability; in these tests, there is no translation of the humeral head until the point of instability, at which sudden and substantial translation occurs (Figs. 16-45 and 16-46).122,137
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree