CHAPTER 29 The Stiff Shoulder
Stiffness about the shoulder was described clinically more than a century ago. It remains a common and frustrating problem seen in orthopaedic practice today. A number of clinical scenarios manifest with loss of motion in the shoulder, and the terminology can be confusing. Despite ongoing basic science and clinical research, the mechanisms that lead to the development of a stiff shoulder are not fully understood and there is still no consensus on the optimal method of treatment.
DEFINITION
Shoulder stiffness is a general term encompassing a spectrum of pathology. It was first described as a clinical entity in the late 19th century by both Duplay1 in France and Putnam2 in the United States. The original term for the condition was scapulohumeral peri-arthritis, which encompassed a number of painful afflictions of the shoulder resulting in stiffness. As more information has developed about the specific conditions that can cause a stiff shoulder, this term has fallen out of favor.
In 1934, Codman described a clinical pattern of muscle spasms and glenohumeral stiffness, which he termed the frozen shoulder.3 He stated that this entity was “difficult to define, difficult to treat and difficult to explain from the point of view of pathology.” In many respects, this is still true today.
A decade after Codman, Neviaser described a similar condition, which he called adhesive capsulitis.4 He believed this term better represented the underlying pathology. Neviaser identified a “chronic inflammatory process involving the capsule of the shoulder causing a thickening and contracture of this structure which secondarily becomes adherent to the humeral head.” The term adhesive capsulitis, however, may be ambiguous because it is sometimes used indiscriminately to describe both the idiopathic frozen shoulder as well as shoulder stiffness related to other causes. Because these are now considered separate entities, it is probably no longer appropriate to use the same term for both.
At a symposium sponsored by the American Academy of Orthopaedic Surgeons in 1992, a workshop committee defined frozen shoulder as “a condition of uncertain etiology characterized by significant restriction of both active and passive shoulder motion that occurs in the absence of a known intrinsic shoulder disorder.”5 We use the term frozen shoulder to describe the idiopathic condition.
CLASSIFICATION
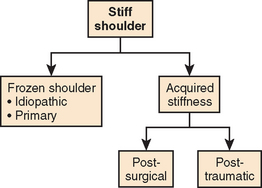
In this chapter, we use the term frozen shoulder to describe the idiopathic condition. This group includes patients with diabetes mellitus. All other conditions fall under the category of acquired stiffness. Acquired stiffness can be subdivided to indicate the mechanism associated with the condition (e.g., post-traumatic or postsurgical) (Fig. 29-1).
NORMAL MOTION AND PATHOMECHANICS
Glenohumeral Articulation
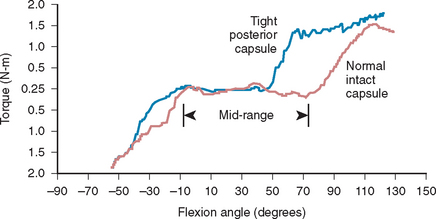
Under normal circumstances, the shoulder is a remarkably mobile joint. The normal ratio of glenohumeral motion to scapulothoracic motion is 2 : 1.6–8 The normal surface area of the capsule is nearly twice that of the humeral head,9 and the capsule is inherently loose. In cadaveric tests, Harryman and associates measured torsional resistance of the glenohumeral joint with an intact capsule.10 The capsule remained essentially free of tension until terminal degrees of motion were reached (Fig. 29-2). The majority of motions performed during work and activities of daily living are carried out in positions within midrange.11,12 At the end ranges of motion (ROMs) increased tension is seen in the static restraints, notably in the capsule and its associated ligaments: the superior, middle, and inferior glenohumeral ligaments.
The anterosuperior capsule in the region of the rotator interval contains the coracohumeral and superior glenohumeral ligament. It assumes tension with increasing external rotation with the arm in 0 degrees of abduction.13–15 The middle glenohumeral ligament and the anterior band of the inferior glenohumeral ligament become taut with maximal external rotation at 45 degrees and 90 degrees of abduction, respectively.16,17 The inferior region of the capsule becomes tighter with increasing abduction. The posterior capsule becomes tight in internal rotation with the arm at the side. Tension is shifted inferiorly with increasing angles of elevation.10,18
Isolated contractures in specific capsular regions have been described.19–25 Often, they are created intentionally during procedures for instability.26 A contracted capsule reduces glenohumeral motion.10 In a cadaveric study, eight shoulders underwent posterior capsular plication. This resulted in limitation of forward elevation, internal rotation, and horizontal adduction. External rotation was unaffected. Tightening of the capsule also increased the torque necessary to achieve an elevated position (see Fig. 29-2).10
Asymmetric tightness of the capsule can cause an obligate translation of the humeral head.18,27 Normally, the glenohumeral joint displays ball-and-socket mechanics, and the humeral head remains centered within the glenoid fossa except at the extreme degrees of motion.8,27 In a cadaveric study, when the posterior capsule was surgically tightened, forward flexion caused consistent anterosuperior translation of the humeral head.10 Clinically, this can lead to impingement of the rotator cuff against the coracoacromial arch. This has been described in throwing athletes who develop isolated posterior capsular contractures.
A similar phenomenon can occur with overtightening of the anterior structures, such as with nonanatomic repairs for anterior instability (Putti–Platt). A chronic contracture of the anterior aspect of the shoulder is almost always associated with a deficit in external rotation compared to the contralateral shoulder. This scenario can result in greater joint reaction forces directed toward the opposite side of the glenoid and can cause excessive wear of the posterior glenoid articular cartilage, posterior bony erosion, and osteoarthrosis.28 Matsen and colleagues have called this process capsulorrhaphy arthropathy (Fig. 29-3).18
To eliminate pathologic restrictions in motion, a number of techniques, both nonoperative and operative, have been described for capsular release. Although newer techniques have evolved over time, the basic concept of releasing either localized or general contractures to improve ROM remains the same.18,22,29–32 The technical details and results of these procedures are discussed in depth later.
Subacromial and Subdeltoid Plane
In 1934, Codman stated that “the subacromial bursa itself is the largest in the body and the most complicated in structure and in its component parts. It is, in fact, a secondary scapulohumeral joint, although no part of its surface is cartilage.”3
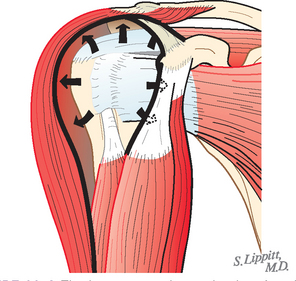
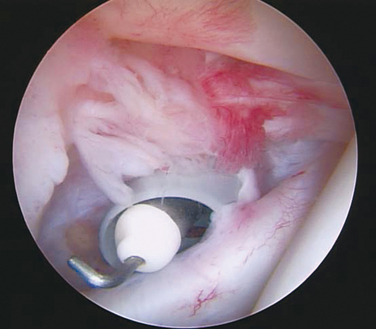
Matsen and Romeo have defined this interface as a sliding surface between the deep side of the deltoid, the acromion, the coracoid process and its tendons, and the superficial side of the humerus and rotator cuff (Fig. 29-4).18,33 Normal biceps glide is also necessary for full glenohumeral ROM. If synovitis is present within the glenohumeral joint or biceps tendon sheath, adhesions can spot-weld the long head of the biceps tendon to the capsule or bicipital groove (Fig. 29-5).20,21,23 Pasteur, in 1932, described peritendinous adhesions within the bicipital groove in patients with frozen shoulder. This finding has also been described by other authors.4,34–37
If adhesions occur in this area, usually secondary to trauma or surgery, shoulder motion can be substantially limited. Potential benefits of arthroscopic procedures (e.g., arthroscopic rotator cuff repair and arthroscopic instability repairs) include a decreased risk of adhesion formation and lower rates of postoperative stiffness when compared with open procedures. Many orthopaedic surgeons also struggle with the rehabilitation protocol after shoulder trauma, specifically with proximal humerus fractures. On the one hand, immobilization can reduce the risk of fracture displacement, but on the other hand, prolonged immobilization clearly is a risk factor for stiffness. Stiffness after proximal humerus fractures can be quite debilitating, even if the fracture has healed in a satisfactory position. One may consider risking some degree of fracture malalignment for improved motion, especially in elderly patients, who seem more prone to developing stiffness after fracture.
Scapulothoracic Motion
Scapulothoracic mechanics are another important component of shoulder motion. Past investigators have determined that scapulothoracic motion is responsible for approximately one third of total shoulder elevation.6,7 Harryman14 and McClure38 have performed studies that describe scapulothoracic motion in detail. Loss of glenohumeral ROM (e.g., after arthrodesis) can result in an accommodative increase in scapulothoracic ROM.20 Although it is a challenge to clinically measure scapulothoracic motion accurately, Nicholson recorded excessive scapular upward rotation (elevation) during active attempts at humeral elevation in patients with frozen shoulder.39 Recent studies have examined shoulder kinematics in patients with stiff shoulders.40,41 Lin showed increased EMG activity in the upper trapezius, with relatively lower activity in the lower trapezius. These findings have potential implications in the rehabilitation of patients with frozen shoulder.42
PATHOPHYSIOLOGY
Although many plausible mechanisms for the development of the stiff shoulder have been proposed, the etiology remains elusive.43 Advances in basic science research, however, have improved our understanding of the condition. Current efforts are focused on determining both an immunologic basis for the stiff shoulder and the role of cell signaling and inflammatory mediators in the development of the condition.
Originally, Duplay felt that stiff shoulder arose from the subdeltoid region. Others have suggested that the source of pathology is found in the intra-articular portion of the biceps and the rotator cuff.9
Riedel was the first to suggest that shoulder stiffness may be related to the joint capsule.44 In 1945, Neviaser correlated the surgical, arthrographic, and histologic findings that occurred in the synovium and capsule of patients with painful shoulder stiffness.4 On histologic examination, he identified perivascular infiltration and capsular fibrosis. The synovial layer itself appeared normal.
Lundberg also did not discover any pathologic changes in the synovium. He described increased collagen density within the capsule and a pattern of glycosaminogly-can distribution that resembled a reparative process.45 McLaughlin found obvious inflammation in the synovium and biceps sheath in only 10% of his cases.30 He posited that “acute synovitis represents one phase in the life cycle of this condition.”
Macnab studied the association between rotator cuff degeneration and painful stiffness.46 He took biopsy samples at the time of open capsular release and identified round and lymphoid cell infiltrates. He hypothesized that this was the result of an autoimmune response directed toward degenerative collagen particles from a hypovascular supraspinatus tendon.
In an attempt to determine an immunologic basis for the condition, a study of 40 patients with frozen shoulder was undertaken by Bulgen and colleagues. They found that patients initially had increased levels of circulating immune complex and C-reactive protein and decreased lymphocyte transformation compared to a control group.47 Repeat testing showed that values tended to approach normal levels following treatment.
Bulgen and associates analyzed serum immunoglobulin (Ig) levels in 25 patients with frozen shoulder, comparing them to age- and sex-matched controls.48,49 Serum IgA levels were found to be significantly reduced in patients with frozen shoulder, and this decrease persisted even after clinical recovery. Lymphocyte transformation in response to phytohemagglutinin was also significantly depressed in the majority of patients. Despite these early findings indicating an immunologic basis for the disease, subsequent reports have failed to support these findings or to identify immunologic tests useful in diagnosis, treatment, or predicting outcome.50
Investigation has also centered on identifying persons predisposed to stiffness by using immunologic markers. Initial research was focused on the presence of certain histocompatibility antigens. The presence of human leukocyte antigen (HLA)-B27 was reported as being more common in patients with frozen shoulder (42%) than in controls (10%).51 This finding, however, was later refuted by the same authors.48 As of yet, no definite immunologic markers have been defined for patients with frozen shoulder.
An association between frozen shoulder and Dupuytren’s contracture has been identified by multiple authors dating back to 1936.52 These reports identify rates of association ranging from 18% to as high as 52%. More recent investigators have likened the histologic changes seen in the glenohumeral joint capsule to those seen in Dupuytren’s contracture of the hand.53,54
Bunker and Anthony performed manipulation and open excisional biopsy of the coracohumeral ligament and rotator interval capsule in patients who failed to improve with nonoperative treatment of frozen shoulder.53 Tissue specimens revealed active fibroblast proliferation amidst thick nodular bands of collagen, accompanied by some transformation to a smooth muscle phenotype (myofibroblasts). These histologic features are very similar to those seen in Dupuytren’s disease, namely, there is neither inflammation nor synovial involvement. Fibrosis is most evident in later phases of the inflammatory response, and collagen and matrix synthesis take place after chemotactic and cellular responses have occurred. These findings, therefore, might reflect a later phase of the disease, and an inflammatory phase might occur earlier.30 Uhthoff and Boileau confirmed the presence of vimentin, a cytocontractile protein known to be present in Dupuytren’s disease, in histologic sections of only the anterior capsular structures in patients with frozen shoulder. This protein was not seen in specimens of the posterior capsule. However, type I and III collagen were seen globally, in both anterior and posterior capsular specimens. They hypothesized that contracture selectively involves only the anterior capsule, whereas fibroplasia involves the entire capsule.55
A proliferative pathologic repair process initiated by active fibroblasts might occur in response to inflammatory infiltration of connective tissue by mononuclear cells that produce polypeptide growth factors. Recently, Mullett and colleagues56 examined the response of human fibroblasts to joint aspirates from patients with frozen shoulder and a control group. Significantly, increased fibroblast proliferation was seen in patients with frozen shoulder. In another study, biopsies were taken from the rotator interval in 22 patients undergoing arthroscopic capsular release. Histologic and immunocytochemical analysis revealed the presence of fibroblasts, proliferating fibroblasts, and chronic inflammatory cells (predominantly mast cells). T-cells, B-cells, and macrophages were also present.57
To determine the specific cytokines involved in the inflammatory and fibroblastic response, Rodeo and associates compared capsular tissue samples from patients undergoing arthroscopy who had frozen shoulder, nonspecific synovitis, or a normal capsule.58 Their results indicate that cytokines such as transforming growth factor (TGF)-β, platelet-derived growth factor (PDGF), and hepatocyte growth factor (HGF) are involved in the early inflammatory stages of frozen shoulder. PDGF is a mitogenic agent that causes fibroblastic cell proliferation, and TGF-β increases extracellular matrix production. Suzuki and associates further demonstrated that specific growth factors stimulate capsular fibroblasts in a canine model. They found that PDGF-AB, HGF, and insulin-like growth factor type I all stimulated the migration of fibroblasts from three different parts of a canine shoulder model: the upper and lower parts of the middle glenohumeral ligament and the posterior capsule.59 A more recent study by Ryu found increased vascular endothelial growth factor (VEGF) expression in the synovial tissue of a group of diabetic patients with frozen shoulder. However, its exact role remains undetermined.60
Matrix metalloproteinases (MMPs), a family of naturally occurring proteinases that control collagen matrix remodeling, have also been implicated as a contributing factor in the pathogenesis of frozen shoulder.61,62 Hutchinson and colleagues reported the onset of frozen shoulder in 12 patients with gastric carcinoma after treatment with the MMP inhibitor, marimastat.62 Bunker and colleagues examined capsular tissue from patients with frozen shoulder, patients with Dupuytren’s contracture, and from normal controls.61 The tissue was analyzed for various factors, one of which was MMPs and their inhibitors. When compared to normal capsule or capsule derived from patients with Dupuytren’s contracture, the capsule of patients with frozen shoulder demonstrated an increase in messenger RNA (mRNA) for MMPs, as well as a natural MMP inhibitor. These results suggest that abnormalities in MMP expression are a factor in frozen shoulder, although a causal relationship has still not been established.
Hannafin and colleagues attempted to correlate the three histopathologic phases of fibroplasia detected in biopsy samples of patients with frozen shoulder, as described by Neviaser, with findings from clinical examination and arthroscopy. They hypothesized that hypervascular synovitis provokes a progressive fibroblastic response in the adjacent capsule that results in diffuse capsular fibroplasia and contracture.54 Based on immunohistochemical and histologic findings, these investigators proposed a cellular pathway, which eventually results in the clinical scenario of a frozen shoulder.
DIAGNOSTIC CRITERIA
Idiopathic frozen shoulder implies a global glenohumeral capsular contracture that occurs in the absence of a definable traumatic event. Acquired stiffness is an extrinsic process related to some other, often traumatic, cause. These conditions might not be mutually exclusive. On rare occasions, inflammation and adhesions have been identified in the subacromial bursa in association with idiopathic frozen shoulder.20 Although acquired stiffness is generally the result of an extracapsular process, subsequent capsular contracture can develop.
Acquired Shoulder Stiffness
The earliest description of shoulder stiffness occurring after trauma was recorded in 1859 by Malgaigne, who wrote with regard to minor nondisplaced extracapsular fractures about the shoulder1:
Some degree of shoulder stiffness is typical after bone or soft tissue injuries around the shoulder. Restriction in shoulder motion has been reported after simple contusions, subluxations, dislocations, acromioclavicular joint injuries, clavicle and scapula fractures, and especially after proximal fractures of the humerus in the elderly.63,64
Localized contractures can develop, usually after repetitive, low-level trauma, and can cause motion loss in specific patterns. Isolated posterior capsular contracture is the most commonly described. Neer discussed the impingement syndrome and encouraged therapeutic stretching in forward elevation, internal rotation, and cross-body adduction.65 Thomas66 and Ticker25 have made similar recommendations. In a review of 30 patients from a prospective study of refractory shoulder stiffness, 11 experienced isolated restriction in motion that was attributed to posterior capsular contracture.21 In each of these patients, an associated pathologic process was identified; in 7 cases, a partial-thickness rotator cuff tear was the pathology.
Surgical procedures are widely recognized as a cause of shoulder stiffness. Anterior or posterior capsulorrhaphy, inferior capsular shift, and rotator cuff surgery can all result in limitation of motion, often by design. Tauro found a relatively high incidence of stiffness in patients undergoing surgery for a rotator cuff tear. Patients with more pronounced stiffness often had difficulty regaining normal motion after surgery.67
EPIDEMIOLOGY
Studies employing stringent diagnostic criteria for frozen shoulder have defined the incidence in the general population as ranging from 2% to 5%.9,68 Nearly 70% of patients presenting with frozen shoulder are women, and 20% to 30% develop stiffness in the contralateral shoulder.69 Recurrence in the same shoulder is quite unusual.70,71 An accurate incidence of acquired stiffness has yet to be determined, partly because of the variability in this patient population.
PREDISPOSING FACTORS
Age
The majority of patients who seek care for a stiff shoulder, regardless of etiology, are between 40 and 60 years of age.18,69,72–75 It is unusual for an idiopathic frozen shoulder to develop in patients younger than 40 years with the exception of those who have had insulin-dependent diabetes since childhood. In a large study, Lundberg noted a slightly higher mean age at the time of presentation in men than in women.45 In contrast, a difference in age relative to sex or type of stiffness was not evident in Harryman’s series of 126 patients with refractory shoulder stiffness.76
Diabetes Mellitus
Patients with diabetes mellitus clearly are at much greater risk for developing limited joint motion, not only in the shoulder but also in other joints.77 Most studies show a 10% to 20% incidence of frozen shoulder, but some indicate the rate of incidence may be as high as 35%.45,78–86 The longer that a patient has been taking insulin, the greater the risk of developing shoulder stiffness82 and the greater the resistance to all treatment modalities.80,85 Patients with childhood onset tend to develop stiffness at an earlier age. In adult-onset diabetics, the age at onset is similar to that of the general population.
Insulin-dependent diabetics with joint stiffness in the hands and other major articulations are categorized as having limited joint motion syndrome.77 Diabetics who have cheiroarthropathy (a waxy thickening and induration of the skin associated with flexion contractures of the fingers) and a frozen shoulder have a higher incidence of retinopathy and bilateral shoulder involvement (77%).80
Rarely, shoulder stiffness is the initial manifestation of a patient with diabetes.87 Lequesne and coworkers discovered 17 patients with glucose intolerance out of 60 new patients with idiopathic frozen shoulder.81 A diabetes work-up should be considered in any patient with newly diagnosed frozen shoulder. Because of the re-fractory nature of shoulder stiffness in long-term insulin-dependent diabetics, early intervention has been considered appropriate to prevent progressive disability.23,80,85
Non-Shoulder Surgery
Stiffness can also occur after surgery that does not involve the shoulder. Common examples include axillary node dissection and neck dissection, especially when these procedures are combined with radiation therapy.88,89 Cardiac catheterization in the axilla, coronary artery bypass grafting, and thoracotomy can also restrict shoulder range because of severe pain after the procedure.90 In addition, stiffness may be triggered by interventional cardiology procedures, such as cardiac catheterization through the brachial artery91 or placement of an ipsilateral subpectoral cardiac defibrillator.92 The incidence of frozen shoulder developing in a male patient population undergoing cardiothoracic surgery has been estimated at 3.3%.93 Frozen shoulder has been described as a barrier to rehabilitation after breast cancer surgery.94
Immobility
In adults, when the shoulder is immobilized, it is at risk of becoming stiff.95–98 A significant number of referrals for shoulder stiffness occur after a period of rest, which is often recommended by the referring physician. In a review of patients referred to Binder and colleagues, 75% were initially told to rest the shoulder rather than to perform gentle exercises.70
Cervical Disk Disease
Degenerative disk disease between C5-6 and C6-7 has been noted to be more common in patients with shoulder stiffness than in a similarly age-matched control group.99 This association has been supported in other studies.30,45,64 Patients with symptomatic cervical radiculopathy and a painful shoulder, with or without loss of motion, experienced less pain and were more likely to regain pain-free motion when cervical traction was added to the prescribed exercise regimen.100
Thyroid Disorders
Bilateral frozen shoulders are rare but have been reported in the setting of both hyperthyroidism and hypothyroidism.86,101–103 Wohlgethan felt that hyperthyroidism, frozen shoulder, and shoulder-hand syndrome were linked disorders.104 Resolution of shoulder stiffness has been shown to occur after thyroidectomy and stabilization of thyroid hormone levels.104,105
Cardiac Disease
The association between atherosclerotic coronary vascular disease and shoulder stiffness is well documented.86,106–109 In a review of 133 consecutive cases of myocardial infarction, Ernstene and Kinell found 17 patients originally, who complained of unrelenting pain in the shoulder region.106 Shoulder-hand syndrome, an autonomic dystrophy, may be a sequela of myocardial infarction in 10% to 30% of cases.110
Bunker identified increased serum lipid levels in a group of patients with primary frozen shoulder when compared to a group of age- and sex-matched controls.111
Pulmonary Disorders
In 1959, Johnson reported that the incidence of frozen shoulder was 3.2% in a population of sanatorium patients with tuberculosis.96 Saha reported that frozen shoulder occurred more frequently in patients with emphysema and chronic bronchitis, but he was unable to correlate this with the severity or the duration of illness.112
Neoplastic Disorders
Bronchogenic carcinoma and Pancoast tumors of the lung can cause severe shoulder pain that can mimic the early phase of frozen shoulder.113,114 Other occult neoplastic tumors can be masked by symptoms attributed to a frozen shoulder. These include chest wall tumors and primary or metastatic carcinoma of the humerus.109,115–117
Neurologic Conditions
Shoulder stiffness has been associated with a variety of neurologic disorders. The incidence of frozen shoulder in patients with Parkinson’s disease is significantly higher than in age-matched controls.118 In 8% of patients, the first symptom of Parkinson’s disease was shoulder stiffness. This can occur up to 2 years before the onset of generalized symptoms.118 Patients with cerebral hemorrhage and cerebral tumors are also at increased risk for frozen shoulder.72,86
At least 30% of patients with hemiplegia have shoulder pain and are susceptible to the development of shoulder stiffness.119,120 Wanklyn and associates also found that patients who required transfer assistance were more likely to suffer from shoulder pain.121 Bruckner and Nye reported a 25% incidence of frozen shoulder in patients who had suffered subarachnoid hemorrhage.72 They found that the development of stiffness was associated with impaired consciousness, hemiparesis, intravenous (IV) infusion, older age, and depression. In a patient with hemiparesis, the clinician may find it difficult to distinguish between shoulder stiffness caused by capsular contracture and muscular spasticity.121 Shoulder-hand syndrome occurs in as many as 30% to 40% of stroke patients and can be terribly disabling.
Brachial neuritis, a painful neuritic condition also known as Parsonage–Turner syndrome, has been associated with frozen shoulder.122 Thoracic outlet syndrome, suprascapular neuropathy, and spinal accessory nerve palsy have all been linked to the onset of frozen shoulder as well.88,123,124
Personality Disorders
Some authors have argued that persons with certain personality characteristics are more likely to develop frozen shoulder. This was first proposed by Codman, in 1934, who described four patients with frozen shoulder who “were a little run-down without anything particular the matter.”3 Coventry coined the term periarthritic personality and found treatment more challenging in this group.125 Fleming and associates profiled the personality type of 56 patients with a frozen shoulder by using the Middlesex Hospital Questionnaire and found that women with frozen shoulder had significantly greater anxiety levels than controls did.126 Tyber found the prevalence of depression to be relatively high in a group of 55 patients with painful shoulder syndromes. He included lithium and amitriptyline in his treatment of these patients.127
The notion of a characteristic personality disorder is controversial. Wright and Haq found no evidence of this when using the Maudsley Personality Inventory to test 186 patients who had a frozen shoulder.86 Matsen and Harryman reviewed the results on the mental health score on the Short Form-36 (SF-36) health status questionnaire for 295 patients with frozen shoulder or acquired stiffness.76 They found that patients with frozen shoulder and patients with acquired stiffness scored within 95% and 88%, respectively, of the mean for normal age-matched controls.
Reaction to Medication
Reports suggest that frozen shoulder can develop after treatment with certain medications. Grasland and coworkers described eight cases of frozen shoulder developing after treatment of human immunodeficiency virus (HIV) infection with protease inhibitors.129 Specifically, all patients received the drug indinavir as part of their regimen and had no other risk factors for frozen shoulder. This association has been confirmed by other investigators.130–133 Other medications that have been linked to the onset of frozen shoulder include barbiturates,134 fluoroquinolones,135 nelfinavir,136 and isoniazid.137,138
EVALUATION
History
Clinical Features of Idiopathic Frozen Shoulder
Frozen shoulder is classically characterized by three stages: freezing, frozen, and thawing.43,74,76
Stage 1: Freezing
This initial stage is characterized by pain. Symptoms have usually been present for several months or less. Typically, patients have what is often described as achy discomfort at rest and severe pain with attempted movements, especially sudden movements. Difficult sleeping is an almost universal complaint. Generally, patients limit their use of the affected extremity as discomfort worsens, causing loss of function to become a major issue. At this point, many patients seek medical attention, although the diagnosis can be easily missed. In fact, many patients are encouraged to immobilize their shoulders, which only exacerbates the problem. Reeves wrote that this phase generally lasts between 2 and 9 months.75
Stage 2: Frozen
In the frozen phase, pain tends to abate, but motion becomes severely limited in all planes. Even simple tasks such as turning off the light and washing one’s hair become a chore. Sleeping comfortably is usually still a major problem. A frozen shoulder is diagnosed in most patients when they enter this stage. Although it can last between 3 and 12 months, the frozen stage can become refractory and last much longer.20,21,23,140
Phase 3: Thawing
In the final stage, ROM slowly returns. As motion improves, residual discomfort generally does as well. Return of full motion can take months to years.141,142 Motion restrictions often persist.43,70 Generally, these restriction are mild and do not cause significant impairment, but patients should be counseled about this early in this disease process.
Clinical Features of Acquired Stiffness
Acquired stiffness does not follow a predictable course like idiopathic frozen shoulder. There are, however, predictable patterns of motion loss after certain injuries. A rotator cuff strain typically causes restricted forward elevation, internal rotation, and cross-body adduction.18,20,25 This is thought to be related to contracture of the posterior capsule.10 Articular-sided partial rotator cuff tears are also associated with posterior capsular contractures.21 Nonanatomic instability repairs result in diminished exter nal rotation. Immobilization after proximal humerus fractures tends to cause global loss of motion because adhesions form in the subacromial and subdeltoid plane.
Laboratory Studies
A patient with routine shoulder stiffness does not need laboratory studies for diagnosis or management.143,144 A complete blood count, C-reactive protein, and erythrocyte sedimentation rate (ESR) may be indicated if there is a concern for infection. A decreasing ESR was seen in patients with successful treatment.70,102,145,146 In more-recent studies, however, ESR has not proved to be reliable or useful when evaluating the patient or monitoring the response to medication.50,147 A fasting glucose level may be ordered if undiagnosed diabetes mellitus is a concern. Lequesne and colleagues found an abnormal glucose tolerance test in 28% of patients with a newly diagnosed frozen shoulder.81
Imaging
Radiographs
Radiographs are routinely performed in any patient with a stiff shoulder.18 Specific conditions that should be ruled out include fracture, malunion, arthrosis, osteonecrosis, and chronic dislocation. The specific views that are obtained vary depending on the clinical scenario, but a minimum of two orthogonal views is mandatory. Additional films, such as cervical spine x-rays, may be warranted depending on the clinical suspicion.
Routine shoulder radiographs in patients with shoulder stiffness and no history of trauma or surgery are typically normal.70 Osteopenia of the humeral head may be seen and is probably related to disuse of the extremity.70,148,149 In 74 cases of frozen shoulder, Lundberg and Nilsson reported approximately 50% bone loss within a short period.148 They felt that this was the result of an inflammatory process and could not be explained by disuse alone.
Nuclear Imaging
A bone scan is rarely indicated in the evaluation of a frozen shoulder because it has not proved to be useful in diagnosis, management, or prognosis. Positive bone scans have been reported in as many as 96% of frozen shoulder patients.150 However, no association between bone scan activity and the severity of disease, duration of symptoms, arthrographic findings, or ultimate out-come has been proved. A bone scan should be ordered only if there is suspicion of a neoplastic process.70
Magnetic Resonance Imaging
As techniques and access have improved, magnetic resonance imaging (MRI) has been become heavily used for evaluating shoulder disorders, including stiffness.151 Emig and colleagues reported on the MRI characteristics of 10 patients with frozen shoulder versus patients with normal shoulders.152 They found a combined thickness of the joint capsule and synovium of greater than 4 mm in patients with frozen shoulder. They did not note significant differences in the volume of intra-articular fluid seen on the MRI scan or in the thickness of the rotator cuff and rotator interval capsule.
The use of IV gadolinium can improve the diagnostic capability of MRI in patients with frozen shoulder. Connell and colleagues noted soft tissue density showing variable enhancement in the rotator interval and partially encasing the biceps anchor on MRI after gadolinium administration.153 Thickening and gadolinium enhancement of the axillary pouch was also seen. Carrillon and coworkers performed IV gadolinium administration followed by MRI and demonstrated enhancement of the synovial lining in patients with frozen shoulder.154 Tamai and Yamato found enhancement of the joint capsule, which was not seen in patients with subacromial impingement.155 One study comparing findings on MR arthrography in patients with and without frozen shoulder, however, did not detect any specific diagnostic findings of frozen shoulder.156
Ultrasound
Several investigators have reported on the use of ultrasound in the evaluation of frozen shoulder.157,158 Ryu and colleagues noted that the main sonographic feature of frozen shoulder was a constant limitation of the sliding movement of the supraspinatus tendon against the scapula.158 They reported sensitivity of 91%, specificity of 100%, and accuracy of 92% when comparing ultrasound with arthrography as the gold standard for diagnosis. As with MRI, ultrasound is not a required diagnostic study and is usually indicated only for evaluating the rotator cuff in patients whose physical examination suggests the possibility for rotator cuff tear to coexist with stiffness of the shoulder.
Arthrography
In 1957, Kernwein and associates performed arthrographic studies in 12 patients with frozen shoulder.159 On open biopsy, they found that the capsule and coracohumeral ligament were very contracted, thickened, and inelastic. They also noted the presence of subacute inflammation. Later, Neviaser described the arthrographic findings of adhesive capsulitis, which included decreased joint capacity, obliteration of the reflected axillary fold, and variable filling of the bicipital tendon sheath.115No correlation between arthrographic findings and treatment outcome has been found.70,160 In routine practice today, arthrography is rarely used.
NATURAL HISTORY
The natural history of frozen shoulder is not well understood. Many consider idiopathic frozen shoulder to be a self-limited disease.3,75,162 However, as stated earlier, it is not uncommon for patients to continue to have some discomfort and restriction of motion even after the resolution of the thawing phase.70,75,142,163 Some patients show absolutely no improvement over time at all or show mild improvement and then reach a plateau.
Meulengracht and Schwartz monitored 65 patients for 3 years and found 23% developed persistent pain and limitation of shoulder motion.102 Reeves monitored 41 patients for more than 4 years and identified residual stiffness in more than 60%, with 12% displaying severe restriction in motion.164 Interestingly, subjective and objective measures of function can differ. At a 3.5-year follow-up, Binder and coworkers found objective motion restriction in 16 of 40 patients, yet only a few complained of significant functional impairment.70 This result was quite different from the findings of Shaffer and colleagues. They monitored 68 patients with frozen shoulder for approximately 7 years. By objective criteria, 30% were restricted when compared with the opposite unaffected side, yet 50% complained of persistent pain or stiffness.142
Wolf and Green analyzed the influence of several comorbidities on the self-reported functional status of patients with frozen shoulder. Increasing numbers of comorbidities were associated with worsening scores on the Disabilities of the Arm, Shoulder, and Hand (DASH) survey, the Simple Shoulder Test (SST), and the SF-36 health status survey.165
Involvement of the dominant arm appears to be a good prognostic sign, whereas occupation, ability to work, duration of stiffness, associated injuries, and the treatment program used did not achieve statistical significance when analyzed against other outcome measures.21,70,141 Patients with insulin-dependent diabetes for more than 10 years also tend to have a poorer outcome.80,82,166
Hand and colleagues have published the long-term outcomes of 269 shoulders in 223 patients with frozen shoulder. Mean follow-up was 4.4 years (range, 2-20 years). Fifty-nine percent of patients had normal or near normal shoulders, and 41% reported some ongoing symptoms. In 94% of patients, these persistent symptoms were mild. Patients with the most severe symptoms at the onset had the worst long-term prognosis.69
TREATMENT
Nonoperative Treatment
Medication
Different types of analgesics and nonsteroidal antiinflammatory drugs (NSAIDs) have been used as supportive measures to manage the pain and inflammatory component of the stiff shoulder. Their effectiveness in alleviating the pain component has been well established.144,167–174 Some authors have reported greater improvement in pain in patients who were managed with nonsalicylate analgesics than with NSAIDs.167 Others have reported that oral steroids produce significantly better improvement in ROM, function, and pain relief in patients with frozen shoulder, but these benefits were not maintained beyond 6 weeks.175,176 Greater improvement can be expected in patients who combine the intake of such medications with a regular exercise program.177
Physical Therapy
Other modalities such as microwaves, short waves, and heat lamps are sometimes considered as additional measures in the rehabilitation process, although they have not proved to be particularly beneficial in any specific phase of shoulder stiffness.178 Similarly, adding ultrasound to the physical therapy exercises has not shown an additional benefit to therapy alone.145,179 Other modalities such as electrophysiotherapy, massage, or more atypical modalities such as hyperbaric oxygen and magnetotherapy have been used, but no additional benefit could be proved and none of these treatments fit into a standard shoulder rehabilitation algorithm.180–183
Adding stimuli to distract the mind of the patient from painful sensations has been shown to be helpful during physical therapy exercises. In one study, significant improvement in the recovery of motion and a decrease in the number of treatments necessary for recovery was demonstrated using audio analgesia as an adjunct to mobilization exercises in patients with chronic frozen shoulder.184 Using the same rationale, TENS (transcutaneous nerve stimulation) has been used in patients with frozen shoulder undergoing physical therapy. Rizk and colleagues used TENS on a group of 28 patients to control their pain during the application of progressive abduction traction.144 Jurgel and coworkers reported on 10 patients with frozen shoulder who were treated with 4 weeks of rehabilitation combining exercises with massage and electrical therapy.185 They were able to demonstrate that this protocol improved shoulder ROM in all directions except for internal and external rotation. They compared this group to another group of 28 patients who were treated with heat and therapeutic exercises. They noticed that the increase in ROM was significantly greater in the former group. This may be explained by the strong attachments between collagen fibers, which show high resistance to suddenly applied tension but which also tend to creep when prolonged tension is applied.
Exercises should be performed gently. Forceful stretching maneuvers are contraindicated, especially in the early phases of frozen shoulder. All forms of light resistance strengthening should be postponed until the patient has recovered ROM.17
For patients to see improvement from therapy, they must assume primary responsibility for their condition. They must understand and participate actively in the prescribed exercises. Some amount of discomfort will need to be tolerated.4,18,70,125,160,162,186 Although it can take several months, a closely supervised physical therapy program leads to improvement of pain and ROM in up to 90% of patients with chronic frozen shoulder.187 In addition, physical therapy has been shown to improve health-related quality of life.188
Nicholson reported on the therapeutic advantage of performing passive stretching in abduction in addition to active ROM.39 Watson-Jones recommended 3 minutes of active stretching each hour and demonstrated that only 5% of 226 frozen shoulders treated with this stretching exercise program alone failed to regain satisfactory ROM within 6 months.162 In another study, 90% of 75 patients who completed a nonoperative program for frozen shoulder achieved satisfactory results, and only 7 patients required more aggressive intervention.189
Dudkiewicz and colleagues reported a long-term follow-up on patients who were managed conservatively with physical therapy and NSAIDs for frozen shoulder190; 54 patients were followed for a mean of 9.2 years (range, 5.5-16 years). Good long-term outcomes were reported, with significantly improved motion in all measured directions.
Lin and coworkers demonstrated the existence of trapezius muscle imbalance with overactivity of the upper compared to the lower trapezius muscle in patients with frozen shoulder.191 They concluded that this imbalance in the trapezius muscle might contribute to scapular substitution in compensation for impaired glenohumeral motion, and thus rehabilitation of the trapezius should be included in the therapy protocol for patients with frozen shoulder.
Occasionally, physical therapy does not help to improve symptoms in patients with frozen shoulder and, at times, can actually exacerbate them. In one report, only 60% of patients who received physical therapy, along with other modalities, achieved the ability to sleep pain-free after 5 months of treatment.144 Hazelman reported on a group of patients who received physical therapy alone; a third of them experienced an increase in pain, and only half of this group significantly improved with exercises.192 Diercks and Steven conducted a prospective study on 77 patients with frozen shoulder to compare the effect of intensive physical therapy and manual stretching versus home exercises within the pain limits (supervised neglect).193 At 24 months’ follow-up, 89% of patients treated with supervised neglect had normal or near-normal painless shoulder function with a Constant score greater than 80. However, only 63% of patients in the group receiving intensive physical therapy reached a Constant score of 80 or higher.
Injections
Several different types of injections have been described for treating shoulder stiffness. The simplest types include intra-articular and subacromial injections. Most of the reports on intra-articular injections involve patients with frozen shoulder and not acquired stiffness.45,194–198 Intra-articular injections can be done along with distention arthrography (brisement), thus combining chemical and mechanical modalities of treatment.164,199 Other types of injections include periarticular (trigger point) injections200,201 and nerve blockade (suprascapular and upper and lower subscapular nerves).202
Intra-articular Injections
It has been proposed that shoulder stiffness begins with an inflammatory phase that is followed by scar formation. The theoretical benefit of an intra-articular steroid injection is to inhibit this inflammatory phase, decrease pain, and prevent further stiffness from developing. The reported effectiveness of intra-articular steroid injections is widely varied in the literature.66,203–205
In most instances, if an intra-articular injection is performed, it is combined with a physical therapy protocol. For this reason, it is difficult to determine the efficacy of this treatment as an isolated modality. Some investigators have suggested that intra-articular corticosteroid injections provide little or no benefit in the management of shoulder stiffness.203,205–207 However, other investigators have shown beneficial effects from intra-articular steroid injections, which consist mainly of improvement in pain but not ROM.146,205,208 When an injection and exercise regimen was compared to analgesics alone, more improvement was observed with the former.209
Widiastuti and Sianturi compared oral triamcinolone intake versus intra-articular triamcinolone injection and concluded that intra-articular steroid administration provided significantly faster improvement when compared to the oral route.210 Williams and colleagues compared exercises and repetitive intra-articular injections of hydrocortisone acetate to serial stellate ganglion blocks, but they were unable to demonstrate significant differences among the treatment groups.198
Others have demonstrated that intra-articular steroid injections were more advantageous than trigger point injections. In one study, 25% of patients with frozen shoulder benefited from an intra-articular injection, whereas none of the patients who received trigger point injections had significant relief.197 In a study by Carette and coworkers, corticosteroid injection plus exercise led to statistically significant improvement versus exercise alone or placebo treatment.211 This improvement may be related to a decrease in pain rather than a real improvement in ROM according to Thomas’s group.66 Ryans and colleagues demonstrated in a randomized, blinded, placebo-controlled study that an intra-articular steroid injection was effective in improving shoulder-related disability, which, in combination with home exercise therapy, led to improvement in shoulder external rotation 6 weeks after treatment.212
Subacromial injections might also have a role. A prospective, randomized, observer-blind study comparing subacromial steroid injection and physiotherapy demonstrated that injections were as effective as physical therapy alone or in combination.213 Some authors have suggested a combination of injections into both the joint and the subacromial space. However, in comparative studies, no significant differences in pain relief and shoulder ROM at follow-up examination were demonstrated after combined injections.194,214 This is not unexpected because in frozen shoulder and many cases of acquired stiffness, much of the pathology is intra-articular.
In our practice, we believe that, during the early phase of frozen shoulder, patients might not be able to tolerate physical therapy exercises because of pain. In this scenario, an intra-articular steroid injection might provide enough relief for the patient to begin an exercise program. We agree with the approach of Weiss and Ting208 and recommend that all intra-articular injections be performed under radiologic guidance to confirm intra-articular placement. In one study, physicians were monitored during intra-articular injection of radiopaque dye, and the majority of them were unsuccessful in delivering the fluid into the shoulder joint.214
When recommending an intra-articular steroid injection, it should be kept in mind that this treatment is not completely benign and complications have been reported. The deleterious effects of intra-articular steroids on tendon metabolism and articular cartilage have been shown in numerous studies.153,215,216 A case of fatal clostridial myonecrosis after an intra-articular injection of steroids in the shoulder has also been reported.217 Harryman reported on six cases of chronic sepsis after shoulder arthrography and steroid injections.218 Shoulder fusion was performed in some of these cases.
Other types of intra-articular injections have garnered interest.219,220 Tamai and colleagues demonstrated that intra-articular injection of hyaluronate led to suppression of synovitis, which suggests an antiinflammatory property.220 In a randomized study, intra-articular injection of sodium hyaluronate plus steroid was compared to steroid alone for the treatment of frozen shoulder, and both groups improved substantially.219 Rovetta and coworkers showed that an intra-articular injection of sodium hyaluronate was not as effective in improving ROM as an intra-articular injection of steroid or physical therapy in the first 3 months after administration.221 In another study, intra-articular hyaluronic acid injection was performed in painful shoulders with either frozen shoulder or osteoarthritis.222 In a short follow-up, both groups improved substantially in joint comfort and mobility.
Intra-articular injection of enzymatic proteases such as α-chymotrypsin and hylase have been used to break up glenohumeral capsular fibrosis.219,222,223 There are few studies in the literature reporting on the results of intra-articular injection of α-chymotrypsin and hylase combined with physiotherapy,223,224 and beneficial effects of this treatment modality were not conclusive. These enzymes are rarely used in current practice.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree