CHAPTER 19 Complications of Shoulder Arthroscopy
Shoulder arthroscopy has undergone dramatic growth since the first clinical report by Andren and Lundberg in 1965.1 Since the 1980s, advances in technology and growing clinical experience have led to an expansion of indications. Treatment of a wide spectrum of shoulder disorders is now within the realm of arthroscopy. The growing volume along with the development of more complex procedures has led to an increase in the incidence and variety of associated complications. Reported complications in the literature, however, are relatively sparse. They are often limited to isolated case reports and small clinical series. Incidences might also be confounded by underreporting and inconsistent definitions of complication.2,3 Despite these limitations, awareness of complications remains important for prevention as well as early recognition and management when they occur. In this chapter we discuss general surgical and anesthesia complications as related to shoulder arthroscopy and complications specific to shoulder arthroscopy.
EARLY REPORTS AND REVIEWS
The first effort to report on complications of shoulder arthroscopy was made by Small4 in 1986. Through the efforts of the Committee on Complications of the Arthroscopy Association of North America (AANA), the complications of 14,329 shoulder arthroscopies were collected from surveys completed by AANA members. Extremely low incidences of nerve injury (0.03%), vascular injuries (0.0%), and infection (0.01%) were reported. Procedure-specific complications were found to be highest with staple capsulorrhaphy (5.3%) and lowest with subacromial surgery (0.76%). The author expressed concerns of underreported rates in this study, given the survey’s reliance on surgeon recall. In a later study, Small5 prospectively collected the complications of 21 experienced arthroscopists over a 19-month period. Shoulder arthroscopy accounted for 1184 of these cases. The overall complication rate was 0.7%. The highest complication rates were associated with rotator cuff repair (11.1%), staple capsulorrhaphy (3.3%), and anterior acromioplasty (1.1%). These pioneering studies represent the early surgical experience with shoulder arthroscopy.
The diversity of subsequent reviews reflects the accumulation of clinical experience that has come with increasing numbers of arthroscopic shoulder procedures and continued technical developments. Curtis and associates6 retrospectively reviewed 660 arthroscopic shoulder procedures with an overall complication rate of 6.5%. A higher rate was found with arthroscopy combined with open procedures (8.8%) compared to all arthroscopic procedures (4.8%). The most common complications reported were adhesive capsulitis (2.7%), wound complications (1.7%), and neurologic complications (0.9%). No infections were reported.
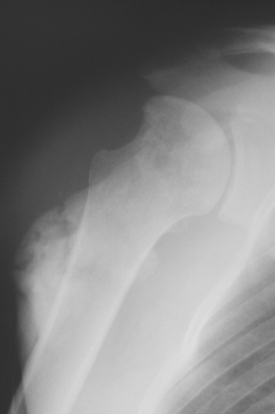
Müller and Landsiedl7 retrospectively reviewed 846 shoulder arthroscopies with an overall complication rate of 5.2%; 43% of the complications were related to infection (Figs. 19-1 and 19-2). Antibiotic prophylaxis, however, was not routinely used in this series. Common complications included adhesive capsulitis (0.78%), neurologic injury (0.68%), and instrument problems (0.78%). A higher incidence of complications was associated with increased surgical time, combined arthroscopic with open procedures, and capsulorrhaphy.

FIGURE 19-1 A draining wound as a result of an infection after combined arthroscopic and mini-open rotator cuff repair.
Berjano and associates2 reviewed a series of 179 arthroscopic shoulder procedures. The overall complication rate was 9.49%. Unlike the previous two reviews, a higher complication rate was found in the all-arthroscopic subset of patients compared to arthroscopic with open procedures. Reported complications included implant failure, neurologic injury, and postoperative edema. Stiffness was not considered a complication in this series.
These retrospective reviews have helped to develop a general profile of shoulder arthroscopy complications. In the rest of this chapter we attempt to formulate a more detailed understanding of the incidence, etiology, and management of specific complications.
ANESTHESIA-RELATED COMPLICATIONS
Interscalene Block
The risks of general anesthesia are well described and not exclusive to shoulder arthroscopy. The complications of regional anesthesia, specifically interscalene block, however, deserve attention given its frequent use during shoulder arthroscopy.8
A reported complication of interscalene block for patients in the beach chair position is the sudden onset of hypotension and bradycardia. Incidence as high as 24% has been reported.9 D’Alessio and associates10 found the average time of symptom onset was 60 minutes from placement of interscalene block and 33 minutes from attainment of the beach chair position. Patients acutely experienced a mean decrease in systolic blood pressure of 36 mm Hg and a mean decrease in heart rate of 21 bpm. One case of subsequent asystolic cardiac arrest requiring resuscitation was reported.
This complication has been attributed to activation of the Bezold–Jarisch reflex.10,11 The proposed mechanism is thought to be a combination of venous blood pooling and decreased ventricular volume induced by the beach chair position and a heightened cardiac contractile state induced by epinephrine introduced from the interscalene block, local infiltration at portal sites, or the arthroscopic irrigation solution. This results in reflex arterial vasodilation and vagally mediated bradycardia.10 Once the complication is recognized, intraoperative therapy usuallyconsists of atropine, epinephrine, glycopyrrolate, or ephedrine, or some combination of these.10,12
Recommended prophylaxis of the reflex includes adequate intravenous fluids to prevent decreased ventricular volume, use of a β-adrenergic blocker to prevent the hypercontractile state, or use of a vagolytic to inhibit the vagally mediated efferent limb of the reflex.10,12 In a prospective, randomized trial, Liguori and associates12 studied 150 patients who received an interscalene block for shoulder arthroscopy in the beach chair position. A significant decrease in the incidence of the Bezold–Jarisch reflex was found with prophylactic β-adrenergic blockade with metoprolol.
Interscalene block anesthesia has also been associated with other complications, including sensory neuropathy, hematoma formation, inadvertent high epidural block, seizure, phrenic and recurrent laryngeal nerve blockade, respiratory distress, and Horner’s syndrome.8,13–18 Although most reported complications are uncommon and rarely permanent, it is also important to realize that this is not always the case. In literature, the incidence of phrenic nerve paralysis has been reported as high as 100%.19 Brachial plexopathies persisting for more than a year and permanent loss of cervical spinal cord function have also been reported.20,21 Although it is not without serious risks, interscalene block remains a reasonably safe means of anesthesia in the hands of experienced anesthesiologists.22
Airway Compromise
Case reports of several additional anesthesia related concerns are also worth discussion. Several authors have reported intraoperative airway obstruction during shoulder arthroscopy performed with interscalene block in the lateral decubitus position.23,24 In both instances, significant extra-articular soft tissue swelling from the arthroscopic irrigation led to compression of the upper airway. Immediate cessation of surgery and management of the airway was required. The patients all recovered uneventfully. Proposed contributing factors included the use of high pump pressure (up to 150 mm Hg),24 long duration of procedure, lateral decubitus position, and procedures involving resection of the joint capsule.23,24 Careful intraoperative monitoring for neck swelling, especially with prolonged procedures, and judicious use of pump pressure, preferably below 50 mm Hg, is important for preventing this rare but serious complication.
Air Extravasation
Air extravasation following shoulder arthroscopy has been reported in the literature in several forms including subcutaneous emphysema, pneumomediastinum, tension pneumothorax, and air embolism.25–29
Lee and associates25 reported on three patients who developed subcutaneous emphysema and pneumomediastinum after undergoing shoulder arthroscopy for subacromial decompression. In all cases, the physicians were alerted after noticing either significant swelling around the neck, face, and chest regions or extensive subcutaneous emphysema. Chest radiographs subsequently revealed bilateral pneumothorax in one patient and unilateral tension pneumothorax in another; patients were treated with chest tube placement, and all recovered uneventfully. The authors attributed the extravasation of air to transient changes of pressure in the subacromial space. They hypothesized that use of suction from the power shaver can create a temporary negative pressure that draws air into the subacromial space from the portals. This air can then be pushed into surrounding tissue when the suction is turned off and positive pressure from the irrigation pump is re-established.
Lau26 also reported a case of subcutaneous emphysema and pneumomediastinum following shoulder arthroscopy. In this case, the author thought air was introduced through a loose junction between the bags of saline solution and the inflow tubing, which resulted in a mixture of air and saline being injected into the shoulder. Vigilance and early recognition of swelling and subcutaneous emphysema is important for appropriate management.
Pneumothorax
Dietzel and Ciullo27 reported on four patients who developed spontaneous pneumothorax following shoulder arthroscopy performed under general anesthesia. All of the patients had significant smoking history and two had a history of asthma as well. The proposed mechanism was that positive pressure ventilation might have ruptured blebs or bullae that were present from the history of heavy smoking and pulmonary diseases. All of the patients were treated with placement of a chest tube and recovered uneventfully. The authors recommended obtaining preoperative chest radiographs to help identify bullae in patients with significant smoking history or pulmonary disease. If bullae are present, the authors recommend performing the surgery under interscalene block anesthesia to avoid the positive pressure ventilation.
Air Embolism
Venous air embolism is a rare complication that can occur during any procedure in which the surgical site is above the level of the heart and noncollapsible veins are exposed to atmospheric pressure, or when any gas is introduced under pressure into a body cavity.29 Although the overall incidence of this complication is 1%, the incidence can increase to 15% when the patient is in the sitting position and air is forcefully insufflated into the operative field.30,31
There are only two case reports of this complication following shoulder arthroscopy.28,29 In both cases, the patients were placed in beach chair position and a large bolus of air (50 mL) was injected into the glenohumeral joint at the beginning of the arthroscopy. Hegde and Avatgere29 believe the mechanism involved a vein being punctured during the portal stab incision or during introduction of the arthroscope; increased intra-articular pressure, caused by the injected air or joint manipulation, then leads to air entering an open vein. They also theorized that in an injured joint, injected air could enter the venous system through exposed venous sinuses.
Clinically, venous air embolism can manifest as decreased end-tidal carbon dioxide, hypoxemia, hypotension, bronchospasm, and cardiovascular collapse.28,29 Management of suspected air embolism includes positioning the patient into the Trendelenburg position, filling the operative site with fluid, and quickly obtaining hemostasis. Blood pressure should be supported with fluids, vasopressors, and inotropes.29 Ideally, avoiding the use of air insufflation during arthroscopy would minimize the incidence of this complication.
GENERAL SURGICAL COMPLICATIONS
Infection
The incidence of infection following shoulder arthroscopy is low. Reported rates in the literature range from 0 to 3.4%.3,6,7,32,33 Two important factors that have been found to be important in minimizing infection are proper disinfection of arthroscopic instruments and preoperative antibiotics. Johnson and associates32 reviewed 12,505 arthroscopic procedures in which 2% glutaraldehyde was used as a disinfectant for cold sterilization of arthroscopes and arthroscopic surgical instruments. The disinfectant offered an advantage over both steam autoclaving, which can damage arthroscopes over time, and ethylene oxide gas sterilization, which is a more time-consuming process. Based on an overall infection rate of 0.04%, the authors found 2% glutaraldehyde to be a safe, quick, and effective disinfecting method. Armstrong and Bolding,34 meanwhile, reported an infection rate of 2.0% in a consecutive series of 352 arthroscopic procedures. One factor that contributed to several cases of postarthroscopic septic arthritis was inadequate arthroscope disinfection.
In a cost-to-benefit analysis, D’Angelo and Ogilvie-Harris33 reviewed 4000 arthroscopic procedures performed without antibiotic prophylaxis. The overall infection rate was 0.23% in this series. A comparison was made between the cost of hospitalization for treating infection and the cost of a single preoperative dose of antibiotic followed by a 24-hour course. Based on an expected fourfold reduction in infection rate with antibiotic use, the authors concluded that it might be cost beneficial to routinely use antibiotic prophylaxis for arthroscopic procedures.
Neurovascular Injury
Injury to neurovascular structures is a risk that must be considered with all surgical procedures. Reports of vascular injury following shoulder arthroscopy are extremely rare. Cephalic vein laceration, leading to hematoma, has been reported during establishment of the anterior portal without residual morbidity.6 Cameron35 reported a single case of venous pseudoaneurysm that developed after inadvertent laceration of a high-pressure cephalic vein during placement of an anterior portal in a dialysis patient. The author recommends alternatives to the anterior portal or using careful blunt dissection when placing the anterior portal in patients with upper extremity arteriovenous fistulas.
Neurologic injuries following shoulder arthroscopy are more common. Incidences ranging from 0 to 30% have been reported in literature, though the majority are transient, neurapraxic injuries.36–39 Injuries to the musculocutaneous nerve,36,40,41 ulnar nerve,40 radial nerve,36,42 axillary nerve,4,39 median nerve, medial pectoral nerve43 and anterior interosseous nerve43 have all been reported. Patient positioning and portal placements are two important factors specific to shoulder arthroscopy that must be considered when evaluating neurologic as well as possible vascular complications.
Traction
Most neurologic complications associated with positioning have been related to the use of traction in the lateral decubitus position. Paulos44 reported a 20% incidence of transient paresthesias in the upper extremity following subacromial decompression performed with traction. Andrews and Carson40 reported a 3% incidence of neurapraxia following 120 shoulder arthroscopies. The injuries were attributed to excessive traction in the lateral decubitus position. Symptoms resolved by 6 weeks in all cases. Ellman42 reported transient dysethesias in the radial sensory nerve distribution secondary to inadequate padding of the wrist during traction.
Several studies have attempted to better understand the mechanism behind these traction injuries. Klein and associates,37 in a cadaver study, measured the strain on the brachial plexus that occurs with traction in the lateral decubitus position. Maximum strain was found with the arm in 0 degrees of forward flexion and 10 degrees of abduction. The minimum overall strain was noted with the arm in 90 degrees of flexion and 0 degrees of abduction. Arthroscopic visibility, however, was limited in this position. The authors concluded that two positions, 45 degrees of flexion with either 90 degrees or 0 degrees of abduction, would minimize strain on the plexus and maximize visibility.
Pitman and associates36 monitored somatosensory evoked potentials (SEP) in 20 patients who underwent shoulder arthroscopy in the lateral decubitus position with traction. Two different arm positions with variable longitudinal or perpendicular traction weights were studied. In 13 patients, the arm was placed in 10 degrees of flexion and 70 degrees of abduction with longitudinal traction. In the remaining 7 patients, the arm was placed in minimal abduction and traction was applied perpendicular to the long axis of the arm. Transient clinical neurapraxia developed in 10% of the patients, all in the 70 degrees of abduction group. Abnormal SEP of the musculocutaneous nerve was detected in all the patients intraoperatively. In half of the patients, abnormal involvement of the median, ulnar, and radial nerves was also noted. The authors felt the high incidence of subclinical, transient decrease in SEP was related to a combination of traction, arm position, and joint distention. They found that decrease in SEP of all nerves could be avoided if longitudinal traction was less than 12 lb and perpendicular traction was kept to less than 7 lb.
Hennrikus and associates45 used pulse oximetry to study the effects of traction on tissue perfusion during shoulder arthroscopy in the lateral decubitus position. Longitudinal traction was found to be the least harmful to perfusion, whereas adding vertical, or perpendicular, traction was most likely to cause tissue hypoxia. The authors found, however, that using a 4-in (10 cm) instead of a 2-in (5 cm) sling for vertical traction improved perfusion.
The beach chair position has been used for shoulder arthroscopy in part to avoid the traction-related complications of the lateral decubitus position (Fig. 19-3). Skyhar and associates38 reported no neurologic complications in 50 consecutive shoulder arthroscopies performed in the beach chair position. In this position, the operative arm is allowed to hang free, with traction provided only by the weight of the arm. Although the risk of traction neurapraxia is decreased in this position, neural injury has also been reported with the beach chair position. Mullins and associates46 reported a case of transient hypoglossal nerve palsy following a combined arthroscopic and open rotator cuff repair performed in the beach chair position. The authors hypothesized that intraoperative changes in neck position might have led to compression of the nerve beneath the angle of the mandible. They recommended frequent intraoperative monitoring of the head and neck position when the beach chair position is used.
Portal Placement
Portal placement is another important factor that must be considered when evaluating neurovascular complications of shoulder arthroscopy. Unlike patient positioning, proper portal placement is important for minimizing direct injury to surrounding neurovascular structures. The key to properly placed portals is a thorough understanding of palpable bony landmarks and regional shoulder anatomy. The standard posterior portal is well described. Its standard location is 2 to 3 cm inferior and 1 to 2 cm medial to the posterolateral corner of the acromion. This portal has been found to be at least 3 cm from the axillary nerve and posterior humeral circumflex artery, and at least 1 cm lateral to the suprascapular nerve and artery.47,48 An accessory posterolateral portal placed up to 3 cm lateral and 5 cm inferior to the posterolateral corner can also be safely established at a minimum distance of 3 cm from the axillary nerve.47
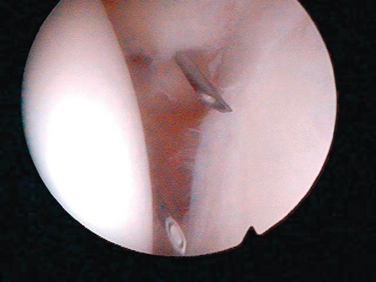
The anterior portal is placed through the rotator interval (Fig. 19-4). Arthroscopically, it is a triangle defined medially by the glenoid, superiorly by the biceps tendon, and inferiorly by the rolled border of the subscapularis tendon. In a cadaveric study, Matthews and associates49 demonstrated the safety of this portal when using the intra-articular triangle as a landmark. They noted that the cephalic vein was the most superficial structure felt to be at significant risk when establishing this portal. The importance of staying lateral to the coracoid with anterior portals in order to avoid inferior and medial neurovascular structures has been stressed by numerous studies.48,50,51 An anteroinferior, or 5-o’clock, portal has also been described.52 The portal has been found to be an average of 22 mm from the musculocutaneous nerve and 24 mm from the axillary nerve.52 Lo and associates47 found that the structure at greatest risk with the anterior portals was the cephalic vein, averaging 18.8 mm from the standard anterior portal and 9.8 mm from the 5-o’clock portal.
Superolateral portals, including the Port of Wilmington and anterosuperolateral portal, are established in the anteroposterior plane along the lateral acromion. The key to these portals is understanding the anatomy of the axillary nerve as it traverses the undersurface of the deltoid from posterior to anterior. The minimum safe distance from the lateral acromial edge increases slightly from 3 cm at the posterolateral corner to 4 cm at the acromioclavicular joint with the arm adducted.53 Segmuller and associates39 reported a 7% incidence of postoperative sensory deficits, with 3% persistent at 8 months, following shoulder arthroscopy. Despite describing posterior and superolateral portals within recommended safe zones, the authors attributed the complications to direct trauma of cutaneous branches of the axillary nerve during portal placement.
The suprascapular fossa portal, or Neviaser’s portal, has also been described.54 The portal is in the superior soft spot surrounded by the distal clavicle and acromioclavicular joint anteriorly, the scapular spine posteriorly, and the acromion laterally. The suprascapular nerve and vessel pass approximately 3 cm medial to this portal.55 Therefore, it is important to pass obliquely into the joint, from medial to lateral, in order to avoid injury to the suprascapular neurovascular bundle when establishing this portal.
Most neurologic complications following shoulder arthroscopy are transient neurapraxias that can be observed. However, permanent direct neurologic injury requiring tendon transfers has been reported.49 Careful attention to patient positioning and proper portal placement are important in minimizing the incidence of this complication.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree