CHAPTER 31 Occupational Shoulder Disorders
Musculoskeletal disorders can be characterized as work-related diseases. The World Health Organization (WHO) defines these diseases as multifactorial, with work contributing significantly, though not exclusively, to causing the disease.1 The term disorder is more appropriate when some of the outcomes are of uncertain pathogenesis and may consist of symptoms without obvious clinical signs.2 The term work-related musculoskeletal disorders (WMSDs) has come to replace repetitive strain injuries or cumulative trauma disorders. The National Safety Council Standards Committee, accredited by the American National Standards Institute (ANSI), combined the etiologic notions implied in these terms to define a musculoskeletal dis-order (MSD) as a disturbance in the regular or normal function of muscle, tendon, tendon sheath, nerve, bursa, blood vessel, bone, joint, or ligament that results in altered structure or impaired motor or sensory function.
Accordingly, WMSDs are MSDs that may be caused, aggravated, or precipitated by intense, repeated, or sustained work activities with insufficient recovery; they generally develop over a period of weeks, months, and years.3 It follows that MSDs can be partially caused by adverse work conditions, can be exacerbated by workplace exposure, and can impair work capacity. The National Research Council adopted a similar definition but emphasized that none of the common MSDs are uniquely caused by work exposure and that physical and social aspects of life outside work need to be considered.4 In this respect, MSDs would be more accurately defined as activity-related conditions rather than work-related ones. Nevertheless, this chapter focuses on the impact of occupational factors.
MSDs of the upper extremities are diffuse neuromuscular illnesses with significant proximal upper body findings that affect distal function.5 The boundaries of the shoulder region are not clearly defined because the neck, shoulders, and upper part of the arms operate as a functional unit. The boundaries are further complicated in that most of the musculoskeletal problems of this region are nonspecific and lack well-defined diagnoses. Aside from variable location, the current definitions of MSDs lack criteria for the intensity, frequency, and duration of the symptoms that indicate a case. Case status is currently based on symptoms that have occurred within a specific time frame (e.g., 1 week), at a specific frequency (e.g., three episodes in the past year), for a given duration (e.g., a single episode lasting 5 days), or with a combination of frequency and severity.6
The chapter excludes several other clinical diagnoses. Primary frozen shoulder is idiopathic, and secondary frozen shoulder is usually the result of a progression of one of the aforementioned conditions or is a consequence of systemic disease. Therefore, it does not conform to the definition of MSD. Thoracic outlet syndrome has been defined as an essentially vascular phenomenon that can be objectively documented. Neurogenic thoracic outlet syndrome, however, is a controversial diagnosis that relies on physical findings when laboratory tests are often negative. Pascarelli and Hsu5 encountered neurogenic thoracic outlet syndrome in 70% of shoulder and upper extremity patients, mostly computer operators and musicians, and postulated that the condition is related to postural derangement. We cannot comment on the etiologic relationship or its work-relatedness and do not consider this condition under OSDs at this point.
OCCUPATIONAL SHOULDER DISORDERS
This chapter uses the descriptive term occupational shoulder disorder to denote WMSDs of the shoulder.7 The term occupational cervicobrachial disorders appeared mainly in the Japanese, Australian, and Scandinavian literature in the 1970s and 1980s but has not been adopted in the United States. Another term, work-related upper extremity musculoskeletal disorders, has also been used, but it includes the elbow, forearm, wrist, and hand.8 Similarly, the Cochran Collaboration review coined the term work-related complaints of the arms, neck and shoulders (CANS).9
An OSD is a symptom complex that is characterized by vague pain about the shoulder girdle, including the paracervical, parascapular, and glenohumeral musculature.7,10–13 It may also be associated with pain that radiates into the region of the upper part of the arm.14 OSDs are thought to be the result of cumulative trauma associated with performing certain activities and tasks.15–17
Epidemiology
The variable definitions of the disorders make it difficult to estimate the burden of OSDs in the general population. The National Health Interview Survey for 1995 showed a 1.74% prevalence of impairment from upper extremity or shoulder MSDs. However, estimates of incidence in the general population, as opposed to the working population, are unreliable because more than 80% of the adult population in the United States is in the workforce.4
The annual survey of occupational injuries and illnesses conducted by the Bureau of Labor Statistics (BLS) is the most frequently referenced source of information on WMSDs in the United States. The U.S. Department of Labor defines a musculoskeletal disorder as an injury or disorder of the muscles, nerves, tendons, joints, cartilage, or spinal disks. MSDs do not include disorders caused by slips, trips, falls, motor vehicle accidents, or similar accidents. In 2005, MSDs accounted for 375,540 cases, or 30% of the injuries and illnesses with days away from work–similar to previous years. Shoulder injuries amounted to 77,800 or 6.3% of all nonfatal injuries in the private industry and 39% of all WMSD. Most were incurred by goods-producing industries. The incidence of shoulder injuries was 8.6 per 10,000 full-time employees; the highest rate (12.3) was in transportation and utility services. The median time away from work due to an occupational shoulder injury was 15 days.18
Connective tissue diseases and disorders, rheumatism, and tendinitis were the most frequent conditions affecting the shoulder. Courtney and Webster19 cross-tabulated the BLS data and found that the most common shoulder injuries were sprains, strains, and tears caused by overexertion; they ranked second to overexertion back injuries. In half the cases, these injuries resulted in 6 days’ absence from work. The most severe shoulder injuries, however, were general symptoms resulting from bodily reaction and overexertion, with a median of 128 days away from work.
The Safety and Health Assessment and Research for Prevention (SHARP) program of the Department of Labor and Industries in Washington State used Washington State fund accepted claims data to estimate the burden of workers’ compensation claims for rotator cuff syndrome (International Classification of Diseases [ICD] codes 7261, 72611, and 8404; Current Procedural Terminology [CPT] codes 23410, 23412, 23415, and 23420) and shoulder WMSDs.20 Men accounted for about two thirds of the claims, and the median age of the claimants was the mid-30s. Of all WMSDs of the upper extremity, rotator cuff syndrome incurred the highest median cost per compensable claim: The cost increased from $3570 in 1987 to $9410 in 1992 and then decreased to $6462 in 1995. The median cost of shoulder WMSDs in that period was $350. In both cases, the average burden is much higher than the median because of skewed distribution. Thus, the average cost was $15,790 per case of rotator cuff syndrome and $7980 per shoulder WMSD. The average time lost per claim was 263 days (median, 97) for rotator cuff syndrome and 213 (median, 41) for shoulder injury. The data for Washington State are probably representative of other states: the data for WMSDs of the upper extremity collected by Liberty Mutual across the United States (10% of the private workers’ compensation market) were similarly skewed.21
Most of what we know about the etiology of MSDs comes from epidemiologic studies.4 These show that MSDs are not unique to any occupational group. Occupations reportedly range from meat processors, to apparel workers or assemblers in the manufacturing industries, to data entry operators in offices. Etiologically, therefore, MSD may be activity related rather than work related. These activities are examined with respect to OSDs.
The data published in various studies of the prevalence and incidence of neck and shoulder WMSDs should be viewed critically. As stated earlier, in the absence of agreement on case definitions in epidemiologic studies, widely different estimates have been obtained for the burden associated with these disorders. Contrasting between two extreme definitions, differences were found in prevalence (55% vs 20%), overall disability (14.6% vs 23.2%), difficulty at work (8% vs 15.5%), and the percentage reporting pain interfering with work (27.3% vs 16.2%). Studies using different case definitions therefore lack comparability.5
In 1997, the National Institute of Occupational Safety and Health (NIOSH) studied the epidemiologic evidence for the work-relatedness of neck, shoulder, and upper extremity disorders.22 The focus of the review was to assess the evidence for a relationship between MSDs and workplace exposure to repetitive exertion, awkward posture, forceful exertion, and hand-arm vibration. Included were studies relevant to shoulder disorders. These disorders were defined by a combination of symptoms and physical examination findings or by symptoms alone, but not specifically defined as tendinitis. NIOSH also included studies for which the health outcome combined neck and shoulder disorders (tension neck, cervical syndrome, thoracic outlet syndrome, frozen shoulder, tendinitis, acromioclavicular syndrome), but in which the exposure was likely to have been specific to the shoulder. Diagnoses of shoulder disorders were based on symptoms determined by interview and physical examination. Shoulder tendinitis included supraspinatus, infraspinatus, and bicipital tendinitis.
The review used five criteria for assessing the evidence:
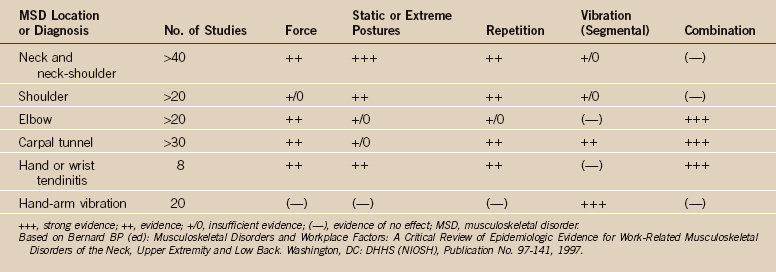
These studies generally compared workers in jobs that involved higher levels of exposure with workers who had lower levels of exposure, with the degree of exposure determined by observation or measurement of job characteristics. The epidemiologic evidence for the risk factors of upper extremity MSDs is summarized in Table 31-1. In the following we focus on risk factors that could be associated with OSDs.
TABLE 31-1 Evidence for a Causal Relationship Between Physical Work Factors and Musculoskeletal Disorders of the Upper Extremities
The NIOSH review also found evidence of a relationship between OSDs and repeated or sustained shoulder postures with greater than 60 degrees of flexion or abduction (factor 2). Of 13 studies examined, 7 reported significant risk estimates (odds ratios, 2.3-10.6). There was evidence for both shoulder tendinitis and nonspecific shoulder pain. The evidence for risk involved in maintaining specific shoulder postures was strongest in those with combined exposure to several physical risk factors, such as holding a tool while working overhead. The association was positive and consistent in the 6 studies that used diagnosed cases of shoulder tendinitis or a constellation of symptoms and physical findings compatible with tendinitis as the health outcome. Only 1 of the 13 studies failed to find a positive association between exposure and symptoms or a specific shoulder disorder. This result was consistent with evidence in the biomechanical, physiologic, and psychosocial literature.
Hildebrandt and colleagues23 reviewed 27 studies that related climatic factors to MSDs, although none of these studies specifically addressed the subject. In a questionnaire distributed to 2030 workers in 24 different occupations, they found that a third of the workers related symptoms at the lower back and neck-shoulder region to climatic conditions. They perceived that these conditions aggravate their symptoms. Sick leave as a result of neck-shoulder symptoms was associated with climatic factors, particularly drafts. The authors concluded that researchers, workers, and patients consider such a relationship plausible but that the epidemiologic evidence is still very weak.
The NIOSH review of the epidemiologic evidence for WMSDs of the lower part of the back found the strongest associations with combined risk factors. Few studies attempted to investigate combined effects on OSDs. Nevertheless, NIOSH needed to combine risk factors to estimate some risk indicators, for example, force exertion and exposure to hand-arm vibration while operating powered hand tools. The combined effect of the latter risk factors for the upper extremities was demonstrated empirically.24
OSDs are multifactorial in origin and may be associated with both occupational and nonoccupational factors. The relative contributions of these covariates may be specific to particular disorders. For example, the confounders for nonspecific shoulder pain may differ from those for shoulder tendinitis. Two of the most important confounders or effect modifiers for shoulder tendinitis are age and sport activities. Subjects who have been extremely active in sports seem to have an increased risk for shoulder tendinitis and acromioclavicular osteoarthrosis, and those who have been extremely active in sports and also report high exposure to load lifting during work are at even higher risk.25 In other words, sports activities add to the workload on the shoulder and increase the risk for OSDs.
Most of the shoulder studies considered the effects of age in their analysis. However, the NIOSH review concluded that it is unlikely that the majority of the positive associations between physical exposure and OSDs are due to the effects of non–work-related confounders.22 In view of the NIOSH estimate of an average risk ratio for OSDs of 4.76 (median, 3.3), it is possible to calculate that on average, 79% of the OSD cases may be attributable to exposure to risk factors at work (the median attributable fraction is close to 70%).
Etiology
The etiology of OSDs, and trapezial myalgia in particular, is uncertain. Two theories have been proposed: the organic or physiologic theory and the psychosocial theory.12
In a study of 20 assembly-line workers with neck and shoulder pain, Bjelle and colleagues found significantly high levels of muscle enzymes, including creatine phosphokinase and aldolase, in 8 workers without any underlying pathology.26,27 The elevated muscle enzyme levels were found to diminish after 2 to 8 weeks of sick leave. In addition, elevated serum creatine kinase levels have been found in welders, cash register operators, and assembly-line workers.28 Such high levels have not been observed in control groups (controllers and forklift drivers). The sustained load necessary for light, static work has been theorized to cause severe adenosine triphosphate depletion, increased permeability, and resultant release of muscle enzymes.29
The level of activity at which a static, isometric contraction of shoulder muscles causes injury is unknown.30 Several researchers have attempted to identify an endurance limit, defined as the highest force that can be maintain for an unlimited period. Jonsson and coworkers suggested that the static load level should always be less than 5% of the maximal voluntary contraction (MVC).31–33 In support of this suggestion, Sjogaard and coworkers have shown that muscle fatigue occurs at 5% of MVC after 1 hour of sustained contraction.34
Multiple EMG studies have suggested that myalgia patients have abnormally elevated muscle tension. Findings among these patients include higher muscle tension in symptomatic patients,35,36 higher muscle tension at sleep,37 higher muscle tension at the painful site,35 pain even when static muscle contraction is as low as 2% to 5% of MVC,38 faster fatigue on the painful side,39 and shorter muscle endurance.40 EMG findings showing decrements in the generation of muscle force during repetitive use provide evidence of either transient motor unit fatigue or permanent skeletal fiber damage.
One theory for decreased fatigue resistance and force generation in myalgia patients is the Cinderella hypothesis.4 This hypothesis suggests that muscle damage may be mediated by mechanisms related to muscle recruitment. According to this theory, relatively small, low-threshold, type I motor units are persistently activated and loaded. These are the first motor units recruited for low-force, repetitive endurance work. They remain in action throughout low-level contractions. Because they carry a disproportionate burden, they are referred to as Cinderella fibers. Sustained contraction and activation of these motor units causes pain and fatigue and can eventually lead to permanent injury. Muscle fiber damage can ultimately result in interstitial myofibrositis with a persistent reduction in blood flow.41 Larsson and colleagues performed bilateral open biopsies of the trapezius muscle in 17 patients with chronic myalgia related to static loads during repetitive assembly work.42,43 Pathologic muscle fibers were identified and found to be related to the presence of myalgia. Additional muscle biopsy studies have demonstrated degenerated mitochondria and increased glycogen deposits.44 Fiber structural damage is also accompanied by products of cell inflammation and necrosis, edema, and leaking of intrafiber proteins and enzymes.4
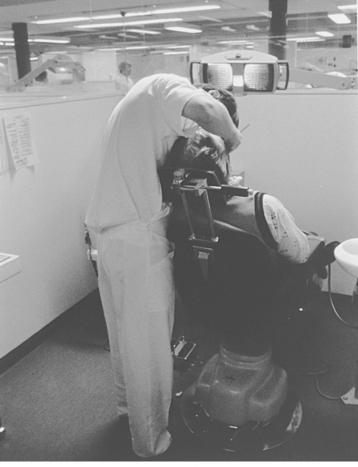
With dropout of some of the muscle fibers, the overall resistance of the motor unit to fatigue is reduced. Clinically, localized fatigue, muscle strain, and pain can occur with very low level contractions, such as those needed to hold the arms in an elevated posture. The trapezius muscle has been found to be affected by jobs that require static muscle overload.32,33,38,45–51 For example, a high prevalence of OSDs has been reported among dental care workers; some were 5.4 times more likely to experience symptoms than a control group of pharmacists.52 This increased risk is considered to be secondary to maintaining an unsupported awkward working posture with cervical flexion of 45 to 90 degrees and shoulder flexion and abduction of more than 30 degrees for extended periods (Fig. 31-1). Excessive scapular elevation as a result of mental stress or workstation design may also contribute to the increased trapezius load.53,54
The psychosocial theory55–60 maintains that emotional stress is an etiologic factor in the development of OSDs. The proponents of this theory contend that OSDs occur in jobs that do not involve excessive muscle strain and, consequently, they are not related to overuse but are more a result of psychosocial factors.61–64 In a study of 607 metal industry workers, depression and distress symptoms were found to be predictors of low back pain, neck and shoulder pain, and other musculoskeletal complaints.65 Workers might fear that if they ignore their symptoms, the symptoms will progress and become permanently disabling. The workers’ compensation system can contribute to this problem by awarding benefits based on the recognition that cumulative trauma can cause significant disability. In a study of 201 patients with chronic pain, Tait and coauthors found that patients with litigation claims reported having pain of significantly longer duration and had significantly more disability than nonlitigating patients.65 Bongers and colleagues found that monotonous work, high perceived workload, and time pressure were causally related to musculoskeletal symptoms.66
In an attempt to address the complex, multifactorial nature of OSDs, Armstrong and colleagues proposed a model that incorporates both the organic and psychosocial theories.67 In this model, exposure refers to external factors such as work requirements. The external exposure produces an internal dose, which in turn disturbs the internal state of the individual person. Such disturbances may be mechanical, physiologic, or psychological. These disturbances in turn evoke a certain response, mechanical or metabolic changes (or both), that occur at the tissue level of the person. Finally, capacity, which can be either physical or psychological, refers to the ability of the person to resist destabilization after various doses of exposure. This model provides a framework to explain the relationship between work exposure factors and the different responses that occur, both psychological and physiologic. A similar model was adopted by the panel of the National Research Council.4
Management
Evaluation of a patient with a suspected OSD involves a thorough history and physical examination. The hallmark of OSD is musculoskeletal pain or discomfort that occurs on the job. Symptoms vary based on the patient’s specific diagnosis. Usually, the underlying diagnosis falls into one of the categories of myalgia, tendinitis, or bursitis. In a prospective study of 204 workers with occupationally related upper limb or neck pain, Sikorski and coworkers found that a discrete MSD existed in 58% of cases.36
Several classifications of OSDs have been proposed, and such systems have been used for the development of treatment protocols. A five-grade classification system was developed by the OCD committee of the Japanese Association of Industrial Health (Box 31-1). This system includes tendinitis as well as several neurologic and vascular symptoms that often accompany occupational shoulder pain. A simplified three-stage system was developed by the Occupational Repetition Strain Advisory Committee in Australia. This system is based on persistence of symptom and interference with work (Box 31-2).
BOX 31-1 Japanese Grading System
Grade II
Subjective complaints with induration and tenderness of the neck, shoulder, and arm muscles
Grade IV
Luck and Andersson12 proposed a pathophysiologic grading system that is a modification of the Australian classification (Box 31-3). This system focuses on myogenic pain. The pathophysiologic basis for pain in grade I is metabolic changes that occur in response to a sustained static load. Progression to grade II involves pain that does not resolve overnight and is secondary to muscle inflammation and early interstitial fibrosis. Grade III is characterized by progression to severe myopathy with interstitial fibrosis. The more advanced the grade, the longer and more aggressive treatment must be in terms of having time off work and using a multidisciplinary approach.
BOX 31-3 Pathophysiologic Grading System
Successful management of the patient requires a multidisciplinary approach. Treatment of physical disorders, evaluation of the psychosocial situation, and an appropriate understanding of the work demands are all equally important. Feuerstein and Hickey suggested a multidisciplinary approach that focuses on physical, ergonomic, and psychological factors.68 They noted that patients treated with a multidisciplinary approach had a significantly higher rate of return to work than did those treated with usual care. Johansson and colleagues reported a significant decrease in sick leave, pain intensity, and analgesic use in patients treated with a cognitive behavior pain-management program. The treatment team included a clinical psychologist, physical therapist, occupational therapist, physical education teacher, vocational counselor, physician, and nurse.69
The medical and surgical management of rotator cuff disease, biceps tendinitis, bursitis, and adhesive capsulitis has been covered elsewhere in this text. The management of myalgia consists of modalities such as the application of ice and heat. Range-of-motion exercises together with strengthening exercises should also be instituted. Antiinflammatory agents may be used in moderate cases, supplemented with low doses of tricyclic antidepressants in more refractory cases. A recent evidence-based systematic review provided evidence for the efficacy of conservative treatments in the management of rotator cuff tendinitis, biceps tendinitis, and trapezius myalgia.70
Changes in the workplace can also be beneficial. Introducing more frequent rest breaks and altering the posture and exertion of force at work can help prevent or alleviate OSDs. Mekhora and coauthors showed that simple ergonomic interventions, such as adjusting monitor height, seat height, and keyboard height can help decrease symptoms in patients suffering from trapezius myalgia. This in turn results in less lost work time and higher productivity.71
Himmelstein and colleagues suggested that in addition to medical management, more aggressive approaches to obtaining control, avoidance of unnecessary surgery, assistance to patients in managing residual pain and stress, and attention to employer–employee conflicts are all important in preventing prolonged work disability secondary to upper extremity disorders.72
DEGENERATIVE JOINT DISEASE
Although the relationship between cumulative trauma and injury to soft tissues about the shoulder girdle has been delineated, the association of glenohumeral arthritis with occupational factors is less clear.60,73–77 Unlike the hip and knee, the shoulder is not a weight-bearing joint, and therefore symptomatic degenerative arthritis of the glenohumeral joint is less common.
A few studies have investigated the association of glenohumeral arthritis with various occupations. Although some of these studies have reported a relationship between certain occupations and osteoarthritis of the shoulder, a direct association has not been found. Kellgren and Lawrence78 and later Lawrence79 found that the prevalence of glenohumeral arthritis in men was influenced by occupation. Waldron and Cox studied the skeletons of 367 workers buried in London between 1729 and 1869 and found no significant relationship between occupation and osteoarthritis of the shoulder.80 Similarly, in a study that included 151 shoulder dissections, Petersson did not find any convincing evidence to support the notion that occupation is a factor in the development of osteoarthritis of the glenohumeral joint.81
As with OSDs, sustained load may be associated with the development of glenohumeral arthritis. Dentists seem to be susceptible as a result of sustained static loads while maintaining the shoulder in a position of flexion and abduction with elevation of the scapula. In a Finnish study that included 40 dentists, Katevuo and coworkers found that 46% had radiographic evidence of osteoarthritis and 44% had bilateral disease.82 In contrast, only 13% in the control group–82 farmers presumably un-exposed to static load–had findings consistent with osteoarthritis.
It has been speculated that pneumatic drilling can predispose workers to degenerative arthritis. To examine the effect of vibration exposure on the shoulder, Bovenzi and colleagues compared 67 foundry workers who used vibratory tools with 46 heavy manual laborers.83 They found no significant difference between the two groups in the prevalence of radiographic changes in the shoulder. In general, it has been difficult to differentiate degenerative changes caused by vibration from those that can simply be attributed to heavy manual work.
Degeneration of the acromioclavicular joint is more common than glenohumeral arthritis. As with glenohumeral arthritis, there is little evidence for a relationship with specific occupations. The NIOSH review cites one study as evidence for an association between acromioclavicular osteoarthritis and occupational force exertion, as well as a dose-response relationship. In a radiographic study of bricklayers and blasters, Stenlund and coworkers84 found that the odds ratios increased with the level of lifetime weight handled on the job. When adjusted for age, construction workers had more than a two times greater risk of osteoarthritis of the acromioclavicular joint than their supervisors did. The authors found that construction workers who also engaged in sports activity were more susceptible to acromioclavicular osteoarthritis. Unlike tendinitis, the risk for those with high workloads did not show job-specific trends: Although the left side seems to have been mostly loaded at work, the risk for the left shoulder was not higher than that for the right side.25 It is possible, though, that the odds ratios for the left side in these studies were underestimated.22
Other studies report contrary findings. In a cadaver study, De Palma found degenerative changes in almost all subjects older than 50 years.85 Petersson often identified degeneration in 30- to 50-year-old persons and regularly in persons older than 60 years.86 Because degeneration occurred with equal frequency in men and women and was of the same severity in the right and left shoulders, the occupation might not have been a contributing factor. In a retrospective study that included 83 patients who underwent distal clavicular resection for arthritis, Worcester and Green found no relationship to occupation.87
PREVENTION
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree