CHAPTER 5 Radiographic Evaluation of Shoulder Problems
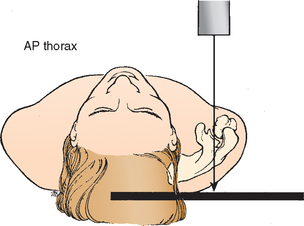
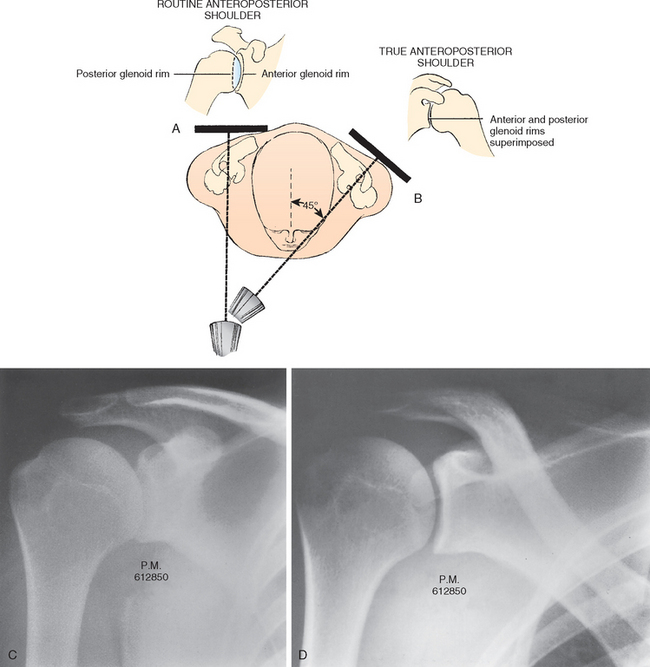
Radiographic evaluation of the shoulder requires a minimum of two views of the area that are perpendicular to each other. The shoulder is a complicated anatomic unit made up of numerous bony landmarks, projections, and joints. The scapula, which lies on the posterolateral portion of the rib cage, rests at an angle of approximately 45 degrees to the frontal plane of the thorax. Thus, the plane of the glenohumeral joint is not the plane of the thorax, and radiographs taken in the anteroposterior plane of the thorax provide oblique views of the shoulder joint (Fig. 5-1). All too commonly, a radiographic evaluation of the shoulder consists of two anteroposterior views of the rotated proximal humerus, which are taken perpendicular to the frontal axis of the thorax.
FRACTURES OF THE GLENOHUMERAL JOINT
Recommended Views
Radiographs of the injured shoulder in two planes (anteroposterior and axillary lateral or scapular lateral) are absolutely essential to evaluation of an acutely injured shoulder. McLaughlin,1 Neer,2,3 Neviaser,4 DeSmet,5 Rockwood and Green,6 Post,7 Rowe,8 Bateman,9 and many others have recognized the shortcomings of the usual two anteroposterior radiographs of the shoulder and have recommended anteroposterior and lateral views to properly assess shoulder problems. The radiographs used to evaluate traumatic shoulder problems have been referred to as the trauma series. The trauma series can also be used as baseline radiographs to evaluate many chronic shoulder problems as well.
Recommended radiographs for the trauma series include the following:
Techniques for Taking the Trauma Series
True Anteroposterior Views
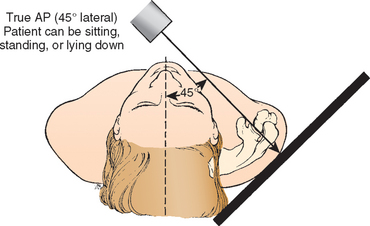
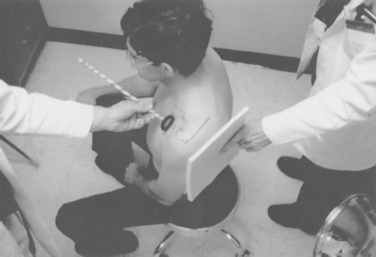
Because the scapula lies on the posterolateral aspect of the thoracic cage, the true anteroposterior view of the glenohumeral joint is obtained by angling the x-ray beam 45 degrees from medial to lateral (Fig. 5-2; see also Fig. 5-1). The patient may be supine or erect, with the arm at the side or in the sling position. An alternative technique is to rotate the patient until the scapula is flat against the x-ray cassette and then take the x-ray with the beam perpendicular to the scapula. Sometimes it is difficult for the technician to properly align the patient for the view. A simple technique to assist the technician in positioning the patient correctly consists of using a heavy marking pen to draw a line on the skin along the spine of the scapula. The technician aligns the x-ray beam perpendicular to the line on the skin and directs it at the cassette, which is placed parallel to the line and posterior to the scapula and glenohumeral joint (Fig. 5-3). Although the scapular spine is not exactly parallel to the plane of the scapula, this technique has proved effective in clinical practice.
The advantage of the true anteroposterior views of the scapula over traditional anteroposterior views in the plane of the thorax is that the x-ray demonstrates the glenoid in profile rather than obliquely and, in the normal shoulder, clearly separates the glenoid from the humeral head (Fig. 5-4). In the true anteroposterior x-ray, the cora-coid process overlaps the glenohumeral joint. If the true anteroposterior x-ray demonstrates the humeral head to be overlapping with the glenoid, the glenohumeral joint is dislocated either anteriorly or posteriorly.
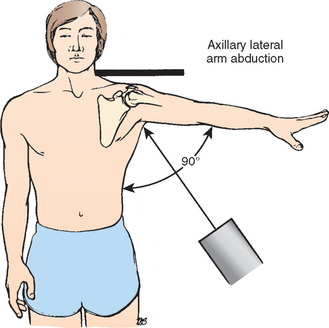
Axillary Lateral View
Initially described by Lawrence10,11 in 1915, the axillary lateral x-ray can be taken with the patient supine or erect. Ideally, the arm is positioned in 70 to 90 degrees of abduction. The x-ray beam is directed into the axilla from inferior to superior, and the x-ray cassette is placed superior to the patient’s shoulder (Fig. 5-5). To minimize the amount of abduction required to obtain an axillary lateral x-ray, an alternative technique was devised by Cleaves12 in 1941. In this technique, the patient may be sitting or supine; the arm is abducted only enough to admit a curved x-ray cassette into the axilla. The x-ray is taken from superior to inferior through the axilla. In some situations when abduction is severely limited to only 20 or 30 degrees, a rolled-up cardboard cassette can be substituted for the curved cassette in the axilla (Fig. 5-6).
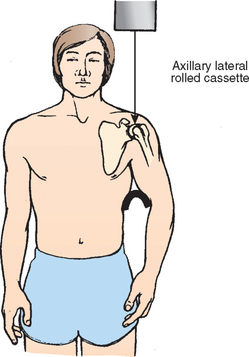
Axillary lateral x-rays provide excellent visualization of the glenoid and the humeral head and clearly delineate the spatial relationship of the two structures. Loss of glenohumeral cartilage is clearly revealed when the joint space between the glenoid and the humeral head is decreased or absent. Dislocations are easily identified, as are compression fractures of the humeral head and large fractures of the anterior or posterior glenoid rim (see Fig. 5-17). Some fractures of the coracoid and the acromion and the spatial relationship of the acromioclavicular joint can also be seen on this view.
If a good-quality axillary lateral x-ray can be obtained, the true scapulolateral view or the modified axillary lateral views are not necessary. However, if because of pain and muscle spasm the patient does not allow enough abduction to get a good axillary view, the scapulolateral or the modified axillary lateral views must be obtained.
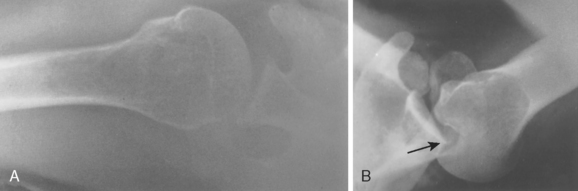
Technique for the Scapulolateral Radiograph
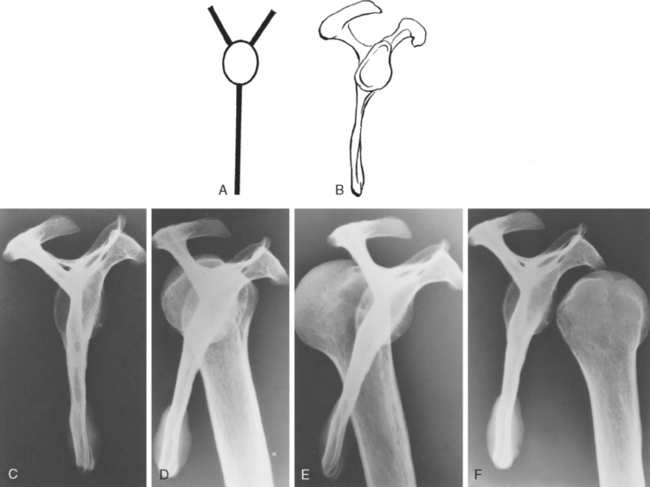
The scapulolateral view is sometimes known as the transscapular, the tangential lateral, or theY lateral.13 The position of the injured shoulder, which is usually held in internal rotation (the arm having been placed in a sling), is left undisturbed. A marking pen is used to draw a heavy line over the spine of the scapula (Fig. 5-7A). The technician then aligns the x-ray beam parallel to the line on the skin, directed to the cassette, which is placed perpendicular to the line at the anterolateral shoulder. The x-ray beam passes tangentially across the posterolateral chest, parallel to and down the spine of the scapula onto the x-ray cassette (see Fig. 5-7A and B). The projected image is a true lateral of the scapula and, hence, a lateral view of the glenohumeral joint (see Fig. 5-7B).
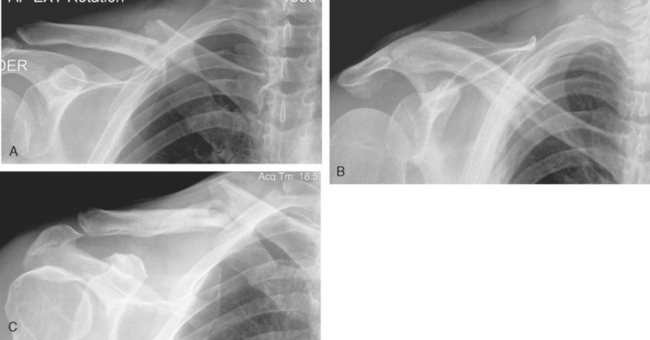
A lateral projection of the scapula forms a Y shape (Fig. 5-8A to C).14 The upper arms of the Y are formed by the coracoid process anteriorly and by the scapular spine posteriorly. The vertical portion of the Y is formed by the body of the scapula. At the intersection of the three limbs of the Y lies the glenoid fossa. In the normal shoulder, the humeral head is located overlapping the glenoid fossa (see Figs. 5-7B and 5-8D). This view is particularly helpful in determining the anterior or posterior relationship of the humeral head to the glenoid fossa.
In anterior dislocations of the shoulder, the humeral head lies anterior to the glenoid fossa (see Figs. 5-7C and 5-8F); in posterior dislocations, the humeral head lies posterior to the glenoid fossa (see Figs. 5-7D and 5-8E). The scapulolateral view does not define fractures of the anterior or posterior glenoid rim, but it does reveal displaced fractures of the greater tuberosity. When this view is added to the true anteroposterior and the axillary lateral views, they represent three views, all 90 degrees to each other, which maximizes the information available for the clinician to use to make an accurate diagnosis.
Techniques for the Modified Axillary Views
Velpeau Axillary Lateral View
Bloom and Obata’s14 modification of the axillary lateral x-ray of the shoulder is known as the Velpeau axillary lateral because it was intended to be taken with the acutely injured shoulder still in a sling without abduction.
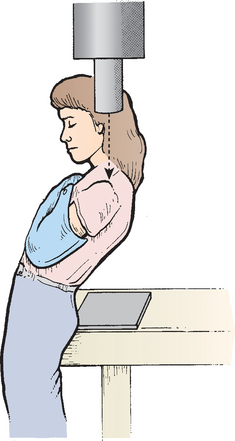
The x-ray cassette is placed on the table directly beneath the shoulder, and the x-ray machine is placed directly over the shoulder so that the beam passes vertically from superior to inferior, through the shoulder joint onto the cassette (Fig. 5-9). On this view, the humeral shaft appears foreshortened and the glenohumeral joint appears magnified, but otherwise, it demonstrates the relationship of the head of the humerus to the scapula.
Apical Oblique View
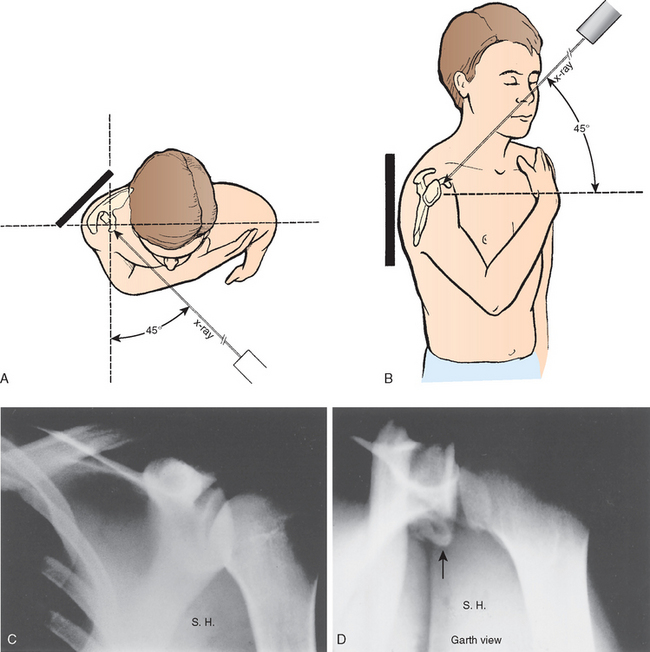
Garth, Slappey, and Ochs have described an apical oblique projection that reliably demonstrates the pathology of the glenohumeral joint.15 The patient may be seated or in a supine position, and the arm may remain in a sling. The x-ray cassette is placed posteriorly, parallel to the spine of the scapula. The x-ray beam is directed through the glenohumeral joint toward the cassette at an angle of 45 degrees to the plane of the thorax and is also tipped 45 degrees caudally (Fig. 5-10A and B).
The resultant x-ray demonstrates the relationship of the humeral head to the glenoid and therefore identifies the presence and direction of glenohumeral dislocations and subluxations. This view clearly defines the anteroinferior and posterosuperior rims of the glenoid and is useful for detecting calcifications or fractures at the glenoid rim (see Fig. 5-10C and D). Posterolateral and anterior humeral head compression fractures are also revealed by this view.
Kornguth and Salazar16 reported that this technique is excellent for diagnosis in the acute setting.
Stripp Axial Lateral View
The Stripp axial view, described by Horsfield,17 is similar to the Velpeau axillary lateral view, except that the beam passes from inferior to superior and the x-ray cassette is positioned above the shoulder.
Trauma Axillary Lateral View
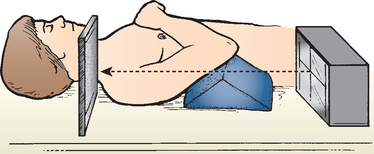
Another modification of the axillary lateral view has been described by Teitge and Ciullo.18,19 The advantage of this view over the Velpeau and Stripp views is that it can be taken while the patient is supine, as is often necessary in patients with multiple trauma. This view can be taken while the injured shoulder is still immobilized in a shoulder-immobilizer dressing. To obtain this view, the patient is supine on the x-ray table, and the involved arm is supported in 20 degrees of flexion by placing radiolucent material under the elbow. The x-ray beam is directed up through the axilla to a cassette propped up against the superior aspect of the shoulder (Fig. 5-11). This view defines the relationship of the humeral head to the glenoid fossa.
Computed Tomography Scan
A CT scan reliably demonstrates fractures, the number of fracture fragments, and fracture-dislocations of the glenohumeral joint. However the addition of a CT scan to the trauma series does not apparently improve the reproducibility of the Neer or AO (Arbeitsgemeinschaft für Osteosynthesefragen) fracture classification.20,21 The technique should consist of 3-mm-thick contiguous sections with a bone algorithm from the top of the acromion to the inferior pole of the glenoid. It is very important that the scan include both shoulders so that the physician can compare the anatomy of the injured shoulder with that of the normal shoulder. Three-dimensional CT scans can provide additional information in the acute setting to evaluate complex or multiple shoulder girdle fractures.
Magnetic Resonance Imaging
The magnetic resonance imaging (MRI) scan is rarely indicated for managing fractures of the shoulder. Specific indications include differentiating nondisplaced greater tuberosity fractures from rotator tendon tears involving a young patient in a post-traumatic situation.22–24 It might also diagnose the pattern of postfracture avascular necrosis.
ANTERIOR INSTABILITY
Recommended Views
With anterior dislocation or subluxation of the glenohumeral joint, there may be bone damage or soft tissue calcification adjacent to the anterior or, particularly, the anteroinferior rim of the glenoid. The true anteroposterior view can demonstrate a fracture of the inferior glenoid that might not be visualized on the anteroposterior views in the plane of the thorax. Although the axillary lateral may be useful to demonstrate some anterior glenoid abnormality, the West Point axillary lateral and the apical-oblique x-rays provide more information.25,26
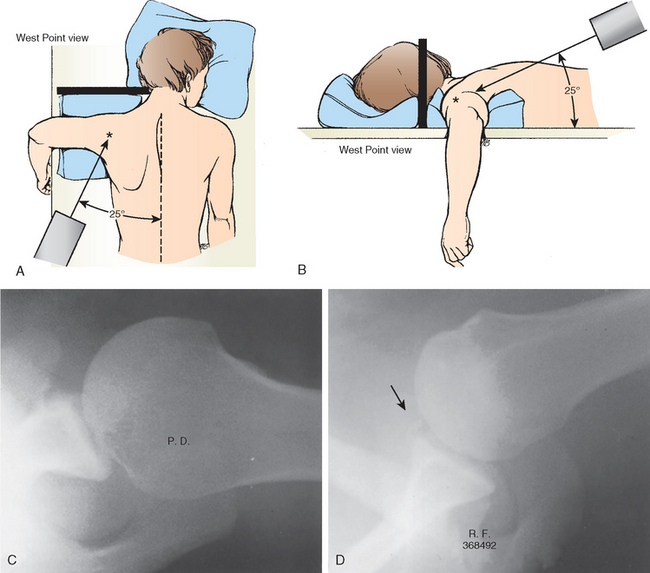
West Point Axillary Lateral View
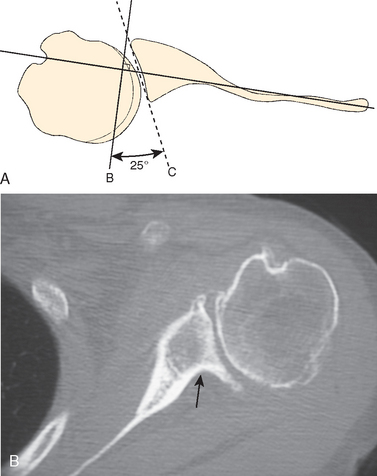
This projection was described by Rokous, Feagin, and Abbott when they were stationed at the US Military Academy at West Point, New York.26 Rockwood has referred to this technique as the West Point view.6 The patient is positioned prone on the x-ray table, with the involved shoulder on a pad raised approximately 8 cm from the top of the table. The head and neck are turned away from the involved side. With the cassette held against the superior aspect of the shoulder, the x-ray beam is centered at the axilla with 25 degrees of downward angulation of the beam from the horizontal and 25 degrees of medial angulation of the beam from the midline (Fig. 5-12A and B). The resultant x-ray is a tangential view of the anteroinferior rim of the glenoid.
The usual finding seen in the traumatic anterior-subluxating shoulder is soft tissue calcification located just anterior to the glenoid rim or anterior-inferior bony fracture avulsions (see Fig. 5-12C and D). A cadaveric study revealed that a 21% glenoid bony defect appeared to be approximately 18% of the intact glenoid on a West Point axillary radiograph.27 Therefore the West Point axillary view provides decisive information regarding anterior-inferior glenoid rim fractures and operative treatment.
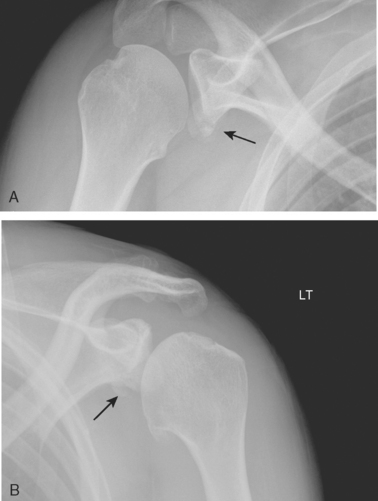
Apical Oblique View
The apical oblique view clearly defines the anteroinferior and posterior superior rims of the glenoid. Pathologic findings of the rim associated with recurrent instability such as displaced malunited rim fractures, glenoid bone loss, or anterior inferior cartilage loss are identified with this view (Fig 5-13). Posterolateral and anterior humeral head defects are also revealed by this view, although CT is necessary to quantify the size of the defect.
POSTERIOR HUMERAL HEAD COMPRESSION FRACTURES ASSOCIATED WITH ANTERIOR DISLOCATION: THE HILL–SACHS DEFECT
Recommended Views
A commonly encountered sequela of anterior shoulder dislocation is a compression fracture of the posterolateral humeral head. This fracture can occur during the first traumatic dislocation or after recurrent anterior dislocations. The lesion is commonly referred to as a Hill–Sachs lesion and was reported by Hill and Sachs in 1940 (Fig. 5-14).28 However, the defect was clearly described by Eve in 1880.29 In the period between the report by Eve in 1880 and the report by Hill and Sachs in 1940, the defect in the humeral head was described by Malgaigne,30 Kuster,31 Cramer,32 Popke,33 Caird,34 Broca and Hartman,35,36 Perthes,37 Bankart,38,39 Eden,40 Hybbinette,41 Didiee,42 and Hermodsson.43
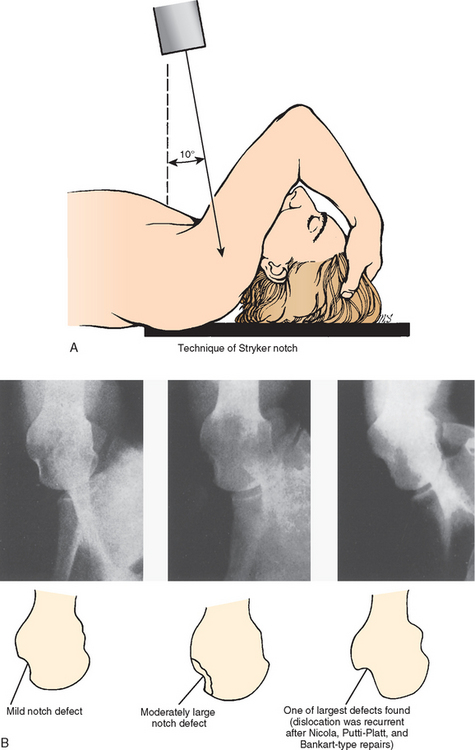
The indentation, or compression fracture, may be seen on the anteroposterior x-ray if the arm is in full internal rotation, and it may be seen occasionally on the axillary lateral view. We believe that one of the best views for identifying the compression fracture is the technique reported in 1959 by Hall and associates.44 The authors gave credit for this view to William Stryker, and Rockwood has called it the Stryker notch view.6
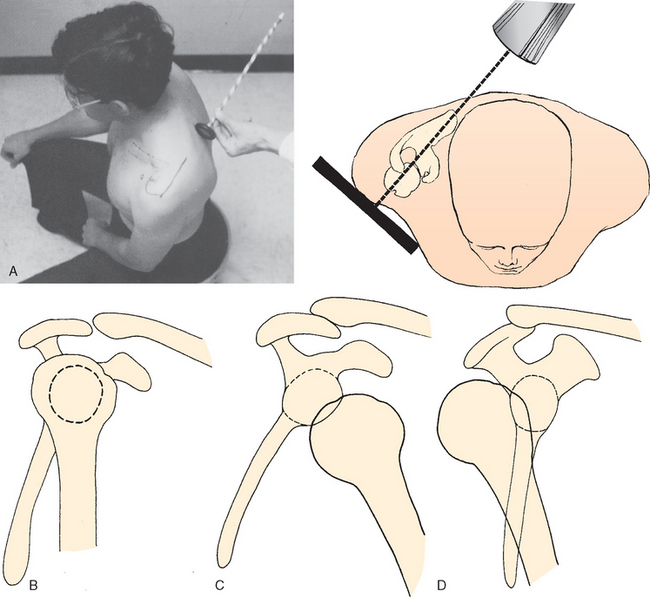
Stryker Notch View
For the Stryker notch view,44 the patient is placed supine on the x-ray table with the cassette under the involved shoulder (Fig. 5-15A). The palm of the hand of the affected upper extremity is placed on top of the head, with the fingers toward the back of the head. The x-ray beam is tilted 10 degrees cephalad and is centered over the coracoid process. A positive result is a distinct notch in the posterolateral part of the humeral head (see Fig. 5-15B).
Anteroposterior View in Internal Rotation
Probably the simplest view, but not the most diagnostic, is the one described by Adams.45 It is an anteroposterior view of the shoulder with the arm in full internal rotation. An indentation or compression can be seen in the posterolateral portion of the humeral head. The defect may simply appear as a vertical condensation of bone. Pring and colleagues46 compared the Stryker view with the internal (60 degrees) rotation view of Adams in 84 patients with anterior dislocation of the shoulder for evidence of the posterolateral defect in the humeral head. The internal rotation view was positive in 48%, whereas the Stryker notch view was positive in 70% of the patients.
Other views predating the Stryker notch view have been described by Didiee42 and Hermodsson43 and are useful in demonstrating the presence and size of the posterolateral humeral head compression fractures. Although these techniques involve views of the proximal humerus with the arm in internal rotation, they are slightly awkward to obtain. The apical oblique view described by Garth and colleagues15 also demonstrates the compression fracture. Strauss and coworkers47 and Danzig and colleagues48 have independently evaluated the efficacy of the various x-rays in revealing the Hill–Sachs lesion and reported that although none of these views always reveals the lesion in question, the Stryker notch view is probably the most effective. The presence of the compression head fracture on the x-ray confirms that the shoulder has been dislocated, whereas its absence suggests that the head may be subluxating rather than frankly dislocating.
After a study of lesions created in the posterolateral humeral head, Danzig, Greenway, and Resnick48 concluded that three views were optimal to define the defect: the anteroposterior view with the arm in 45 degrees of internal rotation, the Stryker notch view, and the modified Didiee view.
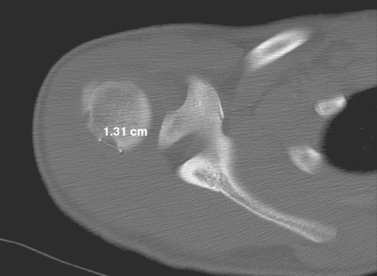
In a study of 120 patients, Strauss and colleagues49 stated that a special set of x-rays could confirm the diagnosis of anterior shoulder instability with 95% accuracy. The x-rays were the anteroposterior view of the shoulder in internal rotation and the Hermodsson, axillary lateral, Stryker notch, Didiee, and West Point views. Whereas the Stryker notch view can document the presence of the compression fracture, the CT scan can be very helpful in determining the size of the compression defect (Fig 5-16).50–56
POSTERIOR INSTABILITY
Techniques to Evaluate Posterior Instability
Posterior dislocation of the shoulder is a rare problem, consisting of 1% to 3% of all dislocations about the shoulder, and it is commonly misdiagnosed.6 There are three reasons for missing the posterior displacement:
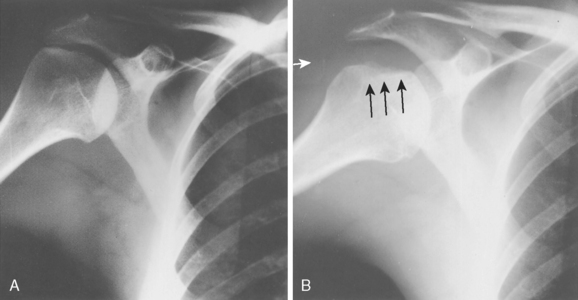
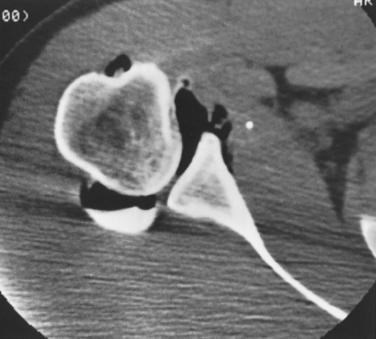
Traumatic posterior glenohumeral instability may be accompanied by either damage to the posterior glenoid rim or impaction fractures on the anteromedial surface of the humeral head, the reverse Hill–Sachs lesion (Fig. 5-17). Lesions of the posterior glenoid rim can usually be noted on the axillary x-ray. The CT scan and MRI scan are very helpful in defining the glenoid rim fracture and in determining the size of the compression fracture of the humeral head.
Special Studies to Evaluate Shoulder Instability
Occasionally in patients with recurrent anterior or posterior dislocations and subluxations, bone abnormalities are not visible on the x-rays. Despite the routine, normal radiologic examination, a significant injury to the soft tissues may be present. In anterior dislocations, the anterior capsule and the glenoid labrum may be stripped off the glenoid rim, as originally described by Perthes37 in 1906 and later by Bankart38 in 1923.
Although an arthrogram might reveal a displaced labrum with contrast material adjacent to the ante-rior glenoid rim and neck of the scapula, Albright,57 Braunstein,58 Kleinman,59 and Pappas60 have each demonstrated that the displaced labrum and capsular stripping can best be documented by arthrotomography of the shoulder joint. Kilcoyne and Matsen61 and Kleinman and colleagues62 used pneumotomography to demonstrate injury to the glenoid labrum and the joint capsule. In a report on 33 cases, they reported good correlation between the tomogram and the surgical findings.
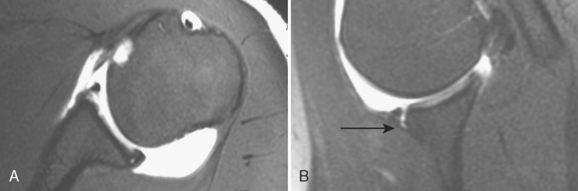
The CT scan, combined with arthrography, can further define the condition of the anterior and anteroinferior labrum. Shuman and coworkers63 used double-contrast CT to study the glenoid labrum with a high degree of accuracy (Fig. 5-18). Various authors54,56,64–66 have shown CT arthrography to be sensitive for imaging the anterior-inferior labrum; however, the presence of anatomic variations has affected its accuracy and reliability.67,68
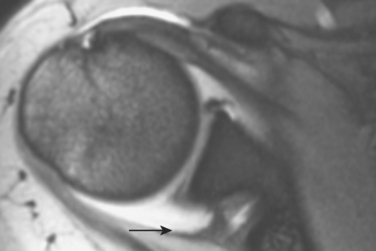
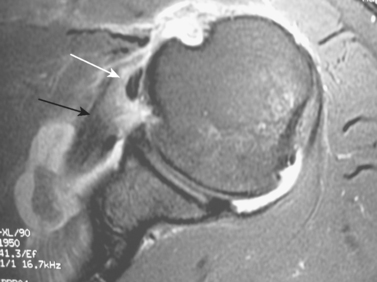
The MRI has become popular for imaging a suspected labral and capsular abnormality associated with ante-rior or posterior instability because it provides anatomic images, is noninvasive, and does not use ionizing radiation. MRI without intra-articular contrast provides limited specific information regarding glenohumeral instability, and a study that is interpreted as normal does not rule out symptomatic glenohumeral instability. Authors have reported the sensitivities of MRI without intra-articular contrast to detect anterior labral tearing to range from 44% to 100%69–73 and the specificities to range from 68% to 95%.68,70,71,73–76 Posterior labral abnormalities have been detected with a reported 74% sensitivity and 95% spec-ificity.71 Superior labral tearing was reported with an 86% sensitivity and a 100% specificity.77 Capsular laxity and capsular insertion sites cannot be assessed by MRI without intra-articular contrast (Figs. 5-19 and 5-20). The high cost of the MRI and the variability in accuracy of the interpretation of the images should negate its routine use in instability imaging.
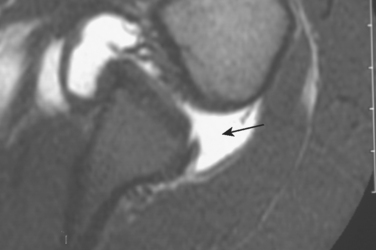
FIGURE 5-20 Posterior labral detachment demonstrated on an axial MRI with intra-articular gadolinium (arrow).
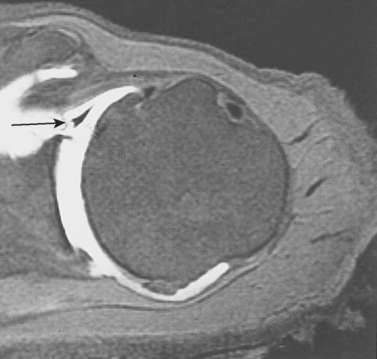
MRI combined with intra-articular gadolinium67 or saline78 provides images that accurately identify labral and glenohumeral ligament anatomy and injury, as well as associated rotator tendon tearing (Figs. 5-21 and 5-22). Intra-articular injection of gadolinium-DTPA (diethylenetriamine pentaacetate) at 2 mmol/L has been shown to have complete passive diffusion from the joint within 6 to 24 hours, and rapid renal elimination has led to almost no systemic side effects.79 A study evaluating MR arthrography of normal shoulders accurately revealed anatomic variations concerning anterior labral signal intensity, form, and size, and the authors concluded that only major tears or detachments of the labrum should be diagnosed.80
In a prospective study of 30 patients, surgical correlation was used to show MR arthrography to be superior to CT arthrography in detecting anterior labral pathology.67 MR arthrography is also useful in evaluating failed anterior instability surgery with a reported 100% sensitivity and 60% specificity in detecting recurrent anterior labral tears.81 The addition of the abduction and external rotation (ABER) position has been shown to increase the sensitivity of MR arthrography in revealing tears of the anterior glenoid labrum (Fig. 5-23). Cvitanic and colleagues compared conventional axial MR arthrograms to oblique axial MR arthrograms in the ABER position and found the latter to be significantly more sensitive in revealing anterior glenoid labral tears (P = .005).82
Capsular laxity remains problematic. In one study of 121 patients undergoing surgery for anterior instability, capsular laxity was missed in all shoulders and capsular insertion sites were found to have no role in predicting clinical shoulder instability.83 In another retrospective review following arthroscopic correlation, MRI and MR arthrography were found by the authors to be limited in providing diagnostic information important to the patient’s surgical management.84 Therefore, routine use of MR arthrography in the diagnosis of glenohumeral instability is not recommended and should be relegated for use as an adjunctive study for special cases. An MR arthrogram study that is perceived as a negative study does not rule out symptomatic clinical glenohumeral instability.
Imaging of the superior labrum may be difficult. However, on coronal fat-suppressed proton-density-weighted MRI, a hyperintense linear fluid signal within the superior labrum creating a 5-mm superior shift of labrum indicates a superior labral tear. Surgical confirmation has shown that MR arthrography reliably and accurately reveals superior labral tears. Sensitivities of 84% to 92% and specificities of 82% to 91% along with substantial interobserver agreement make MR arthrography the gold standard for radiographically evaluating superior labral tears.85,86
GLENOHUMERAL ARTHRITIS
Recommended Views
Loss of articular cartilage leads to the shoulder pain of glenohumeral arthritis. The radiographic views that demonstrate joint space narrowing or articular cartilage loss are the true anteroposterior, the axillary lateral, and the apical oblique (Fig. 5-24). Osteophyte formation and humeral head deformity are revealed by internal and external rotation anteroposterior radiographs of the shoulder. Posterior glenoid erosion and posterior humeral head subluxation can also be shown by the axillary lateral radiograph and apical oblique. However, we do not rely upon the axillary lateral to determine glenoid version because Galinat87 determined that up to 27 degrees of variation exists, depending on the angle of the x-ray beam and scapular rotation.
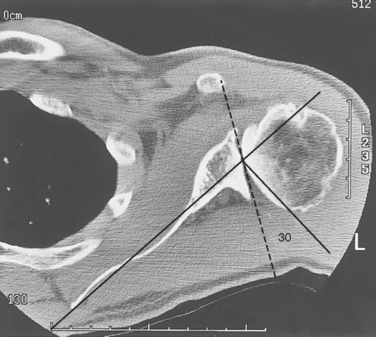
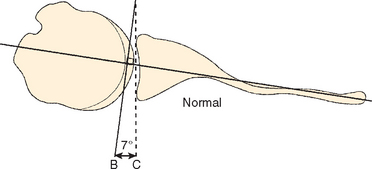
Glenohumeral arthritis may be accompanied by various patterns of glenoid erosion (e.g., central or posterior). CT of the glenohumeral joint has been shown to be accurate and reliable in assessing glenoid morphology and version (Fig. 5-25).88,89 A limited CT scan of both shoulders should be performed, beginning just inferior to the coracoid process (Box 5-1) to determine the glenoid version (Fig. 5-26). The glenoid version is the angle formed by a line between the anterior and posterior rims of the glenoid and a line perpendicular to the axis of the scapular body. The normal glenoid version varies from 0 to 7 degrees of retroversion. The version increases when posterior glenoid erosion is present (Fig. 5-27).88,90,91
BOX 5-1 Technique for Limited Computed Tomography Scans of the Shoulders
Scout Scans
Bilateral shoulders in a straight line, symmetrically placed across the top of each acromion
A preoperative shoulder CT scan to assess glenoid version has been shown to avoid shoulder arthroplasty component malposition and subsequent failure due to unrecognized posterior glenoid wear.90 A CT scan is recommended before shoulder arthroplasty if the patient has less than 0 degrees of glenohumeral external rotation, has had a previous anterior reconstructive procedure, or has questionable radiographic posterior glenoid erosion or posterior humeral head subluxation. Preoperative three-dimensional CT scans have also been shown to accurately reflect the glenoid vault and surface.92 This information may be useful in preoperatively evaluating shoulder arthroplasty patients who have significant glenoid bone loss.
GLENOHUMERAL ARTHROPLASTY
Evaluation
The routine radiographic evaluation of a glenohumeral arthroplasty should consist of the recommended views to evaluate component position and glenoid articulation. Humeral stem lucencies or migration and humeral head height with respect to the greater tuberosity can easily be followed with anteroposterior views in internal and external rotation.93 The axillary lateral and apical oblique views can reveal cartilage wear of the glenoid or instability of the humeral component.
Radiographic evaluation of the glenoid component should routinely consist of a true anteroposterior view of the glenohumeral joint, an axillary lateral, or an apical oblique. The presence of lucent lines about a keeled or pegged component should be noted at the first postoperative visit as well as the seating of the component on the native glenoid.94 Fluoroscopic positioning of radiographs has been shown to be a more accurate method of identifying glenoid component radiolucent lines,95 but it exposes the patient to a large amount of radiation and is time consuming for the patient.
The painful shoulder arthroplasty radiographic evaluation should consist of the recommended views to assess component fixation, position, and stability. Occasionally a limited CT scan provides useful information regarding glenoid wear or humeral component malposition. CT of a cemented pegged polyethylene glenoid component has been shown to be more sensitive than radiography in identifying the size and number of peg lucencies.96 MRI97 and ultrasonography98,99 have been reported as useful for identifying rotator cuff tendon tears in the painful shoulder arthroplasty.
CLAVICLE
Recommended views are an anteroposterior radiograph in the plane of the thorax, a 30-degree cephalic tilt radiograph, a 30-degree caudal tilt radiograph, and occasionally a tomogram or CT scan. These three radiographs are useful for delineating the characteristics of an acute fracture (Fig 5-28) and are even more helpful in monitoring progress of the fracture toward union. Tomograms or CT scans are required to assess fracture healing and evaluate fractures of the medial portions of the clavicle.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree