CHAPTER 107 Functional Restoration
Spinal rehabilitation has long aspired to be the proverbial “backbone” of spine care around the world. Application of scientific method and acumen has played an important role in overcoming fears about rehabilitation and functional capacity/limitation after injury. Spine specialists recognize that minimizing bed rest1 and maximizing early activity return are not harmful and show improved functional outcomes over “restful waiting” in 90% of patients who suffer an acute episode of low back and/or leg pain. Moreover, aggressive, quota-based rehabilitation appears to improve symptoms more rapidly than natural history in placebo-controlled trials. Even without treatment, pain symptoms improve over 90 to 120 days.2,3 Despite advances, there is still a paucity of knowledge as to appropriate triage and disposition of the 10% of spine injuries who fail all single-provider interventions (including surgery) and absorb 80% to 90% of the money spent on spine care.4,5 Since the 1980s integrated, interdisciplinary, advanced spinal rehabilitation has been recognized as the “gold standard” of care for treating patients who do not improve with other interventions.
As with most professions, best-practice philosophies and actions in spine care vary with practitioner experience when data are lacking or idiosyncratically derived. Despite a body of evidence assessing the frame-of-reference skew, surgeons often see a disproportionate number of conservative care failures and nonsurgeons see the devastation of inappropriate or poorly performed surgery.6 In the end, surgical and nonsurgical spine physicians both rely excessively on empiric data that result in inversely skewed frames of reference, allowing a significant minority of patients to become disabled failures.7
This chapter seeks to address the most contentious and interesting patients—those who fail to improve within 90 days to any single-provider modality—and who receive increasingly aggressive and invasive interventions with variably poor functional outcomes. Creating a best-practice model for this population is further complicated by the fact that pain infrequently correlates to radiologic findings nor do outcomes correlate with radiologic criteria for success.8,9
The industrial population, which still remains an important plurality of the spine-care population, poses even greater challenges for discerning best-practice treatment. For various reasons, most industrial claim patients are an excluded population from the majority of spine literature. This aberration calls into question the generalizability of much of the spine surgical literature to the industrial injury or persistent pain populations. What is generally true for spine injury (where 90 days of conservative treatment allows for 90% of the population to recover) is often untrue in work-related spine injuries. Moreover, convincing data show that delay in care beyond 6 weeks in the industrial population is a strong predictor that impairment by injury may progress to a disability.10 The paradox of the refractory 10% of spine-injury patients is that their pain has a multifactorial origin, deeply submerged, inaccessible to visual inspection, and subject to diverse influences such as psychologic stress, coping failure, social-status forfeiture, and financial collapse.
Interdisciplinary experience is not usually part of physician training with the consequence of secondary phenomena remaining unrecognized by the physician or chiropractor who has no mechanism (or “second set of eyes”) available to negotiate the dissonance and contradictory feedback from the patient who is disabled by pain.7 Greater understanding of phasic care models has progressed over the past 2 decades documenting cost and outcome success from care that has been tiered into primary, secondary, and tertiary modes of treatment. Each mode brings with it greater expense but commensurate greater functional return in exchange for the increased cost. The concepts underlying the phasic care model are identified in consensus panel documents such as provided by the North American Spine Society.11 Briefly outlined, primary care refers to modalities applied during acute injury intended to modify symptoms. These including, but are not limited to, surgery, manual techniques, early single specialty mobilization, and educational programs such as so-called “passive modalities” (e.g., immobilization after surgery, electrical stimulation, temperature modulation, possibly traction). Treatment is customarily provided by a single professional, with a limited number of treatments applied to a large number of acute-phase patients who appear clinically and radiologically appropriate. Secondary care refers to therapy provided to a smaller number of patients not responding to initial symptom-modification treatment. The postacute or postoperative symptoms often require care plans focused on reactivation with programs generally adapted to combine quota-based exercise programs with education. Occasionally, additional passive modalities are employed for symptom modification. The primary aim is to prevent/reverse late phase deconditioning that is associated with the transition from functional impairment to disability. In some cases, secondary care may have a degree of programmatic consolidation (i.e., back-school), particularly toward the end of the postacute period, but it is not required to be on site, nor is it required in the majority of cases. The lead role in secondary care is usually performed by physical and occupational therapists, with physicians, psychologists, social workers, disability managers, and/or chiropractors acting as consultants to ensure progress back to maximal function.
Although specific programmatic terms are still in flux, the concept of levels of care is increasingly accepted in clinical referral patterns and local statute.12,13 Enforced by local rule/statute in a growing number of states, evidence-based program definitions allow greater hope of achieving the goal of quality of care. It is with the best evidence available that a specific program term, functional restoration, developed at the Productive Rehabilitation Institute of Dallas for Ergonomics (PRIDE), is discussed as an exemplar of the type of tertiary care model available at several centers of excellence around the country. Functional restoration is designed for individuals with chronic pain who are also disabled from performing many activities of daily living (ADL) or work functions. By its nature, functional restoration is especially suitable for work-related injury, workers’ compensation (WC) cases, or other types of compensation injuries (long-term disability, Social Security Disability, motor vehicle accidents). However, interdisciplinary, tertiary care also has demonstrated benefit in those who have suffered a disabling injury with or without the secondary gain of compensation.14 The goal of this chapter is primarily to provide the reader a direct understanding of how an interdisciplinary program improves health outcomes for both postsurgical and nonsurgical failures of lower-level care by dissecting out various program requisites and their respective structure including the roles of members of the interdisciplinary team within a tertiary care setting.15,16 Finally, the chapter demonstrates evidence for best-practice quantitative assessment that is vital to replacing subjective, unreliable pain scores with quantitative data to follow a particular patient’s progress toward functional goals.
Functional Restoration Phases and Personnel
As outlined earlier, the goal of tertiary-level functional restoration is to use the team model to overcome the multifactorial biopsychosocial barriers that prevented patients from succeeding at lower, less expensive levels of care. A concept repeated throughout this chapter is the paradox that makes this vastly expensive 10% of the musculoskeletal-injury population different. Namely, they are disabled by pain that is ultimately self-serving, nonquantifiable, and frustrating to family, friends, and care providers who try to ameliorate it, further isolating the patient from his or her normal social role and health homeostasis. Many complex patients, requiring tertiary-level care, are self-selecting experts able to transform any attempt at objective measurement to a discussion of their degree of suffering. The unique skill of this type of patient is precisely the reason an interdisciplinary team is crucial to changing the patient’s dysfunctional trajectory. Although the rest of the chapter is devoted to the precise tools at the team’s disposal, this section focuses on mapping the roles of the team and providing an overview of an appropriate progression through a validated, peer-reviewed, outcome-substantiated program. The example and outcomes data in Table 107–1 are from more than 25 years of experience at the Productive Rehabilitation Institute of Dallas for Ergonomics (PRIDE), but the roles, progression, and tools available in this chapter are validated, generalizable, and useful in many other contexts.
TABLE 107–1 One-Year Follow-up Outcome Goals for Functional Restoration
| Outcome | Results |
|---|---|
| 1. Return to work | >90% |
| 2. Work retention (1 year) | >80% |
| 3. Post-treatment surgeries | <4% |
| 4. Percentage unsettled claims | <15% |
| 5. Spine-related medical visits (except for functional restoration or referring physician visits) | <5 visits/yr |
| 6. Rate of recurrent injury claims (lost time) in patients returned to work | <2%/yr |
Initial Evaluation
The quantitative functional capacity evaluation (FCE) is the physical assessment portion of the visit. As discussed later in the quantitative evaluation of physical function portion of this chapter, in a tertiary setting, pain and hypo-mobility fail to be accurate guides anymore. The point of assessment for an interdisciplinary program is to gather quantitative information not necessarily seen with single-specialty qualitative analysis when lower levels of care have failed. In other words, this portion of the exam is intended to “set the speedometer” of the patient’s current functional state in several physical domains. Most important is the assessment of mobility and strength around the putative weak link or dysfunctional motion segment. Building on the initial physician assessment, both the physical and occupational therapists collaborate by evaluating first range of motion, then dynamic strength, and finally endurance of the functional unit, checking each against both an internal validation method, effort factor, and an external validation method, normative database, that is adjusted for age, weight, and gender (see “Isolated Trunk Strength Assessment” later). The next domain is a whole-body performance assessment, usually the province of the occupational therapist, to give information to the team about the degree of deconditioning in noninjured segments of the body and to look for paradoxical discrepancies that portend nonfunctional, compensatory injury behaviors. Finally, cardiovascular measures give important data on deconditioning, materials handling performance, positional tolerance, effort, and gym tolerance of the prospective patient. The complexities of performing an FCE on a chronic pain patient are discussed in greater detail in an American Medical Association publication.17 All of this information is collated into a form to be interpreted by the physician when formulating the comprehensive program.
The psychologic assessment comprises a complex interplay of tests administered with the help of a staff psychologist comparing self-report scores, functional questionnaires, and affective inventories to quantify objective levels of depression, anxiety, fear, inhibition, and occasionally antisocial or manipulative traits (see “Psychologic Assessment” later). These data are collated with the structured clinical interview (SCID) to assess for barriers to participation and, more importantly, barriers to eventual functional return. Like the physical and occupational therapist, the psychologist tallies the quantified data for the physician to assess the degree of psychologic intervention and possible need for pharmacologic adjuncts in determining program length.
Outcome Tracking Phase
This important program phase allows continued evaluation of long-term effectiveness of the program, both from the patient’s point of view and for the facility’s continuous quality improvement (CQI) initiative. A long-term care plan (LTCP) may be offered to the patient for quarterly visits to the supervising physician, who can provide medications to assist in meeting program goals (i.e., work return, home exercise, and decreased health utilization). The opportunity to return, as needed, for symptom exacerbation for focused interventions consistent with functional restoration philosophy is important for maintaining cost effectiveness. The patient is given the opportunity to consolidate gains, obtain feedback, and maintain his or her physical capacity plateau by repeated quantitative FCEs performed at regular prescribed intervals. A patient also has the opportunity to present himself or herself for team feedback at one full-team staffing after the intensive phase. Telephone outcome tracking is administered at 3-, 6-, and 12-month graduation anniversaries by the staff, with assistance sought from treating doctors, adjusters, and attorneys whenever needed if new problems arise (see Table 107–1). Effort is made during this phase to reinforce independence in the patient so that return visits are minimized to evaluations only, unless a new crisis requires a few “refresher sessions.” An added benefit for retaining contact is the willingness of team members to help with problems that arise after the program. Patient perception of an environment of care that extends beyond their graduation leads to a high rate of compliance in repeat testing and telephone tracking. This high contact rate, in turn, allows performance of 1- and 2-year follow-up studies such as has been performed at PRIDE.18–20
In addition to the Level II to III evidence for Therapeutic Studies cited earlier, many research publications of prognostic interest have been provided through the PRIDE Research Foundation. Since 1993, all entering and completing patients provide a large database of prospectively collected data on physical function, psychosocial function, occupational issues, and demographics. Data are updated through repeat tests/interviews on program completion and ultimately compared with the objective outcomes on work, health utilization, and recurrent injury status. To date, more than 5000 program completers and 2000 noncompleters have been studied and have become the focus of numerous prognostic cohort studies delivering Level I scientific evidence. These studies have examined the effect of demographic factors such as length of disability, age, or gender,21–23 as well as a comparison of patients with neck and upper extremity problems with those with lumbar injuries.24–26 They have also compared lumbar discectomy with fusion27 and investigated prerehabilitation psychologic status.28–31 Finally, the effect of program behaviors including final ratings of pain/disability and health utilization have provided Level I scientific evidence.32–37
Quantitative Evaluation of Physical and Functional Capacity
For this book’s audience, the main principle to understand in tertiary level, interdisciplinary, functional restoration is that the usual way we assess activity tolerance (namely by endurance and pain) is, in this self-selected population, unreliable and counterproductive to functional return. As such, validated, reproducible quantitative measures of physical and psychologic dysfunction, termed by the authors as weak links, must be employed to track functional gains. The FCE has become a popular term that subsumes such a variable set of methods and tests under its nominal rubric that it now has no specificity, potentially rendering a general FCE poorly diagnostic/prognostic for patients with impaired insight to their own function. Moreover, many of the developers of certification in this area engage in a speculative turf war by teaching and marketing opposing principles while simultaneously criticizing competitors as invalid. Additionally, few of the FCE methodologies use a quantitative approach but instead employ qualitative, observational methodology that is traditional in physical therapy. Key principles of quantification, using physics-based terminology, are poorly understood by most therapists and physicians. As stated earlier, functional restoration requires true quantification of function because the absence of numeric data leaves physically inhibited patients and their care team enslaved by the cliché, “If it hurts too much, don’t do it.” Greater understanding of accuracy, precision, and sources of error in any quantitative methodology is necessary.38 In the PRIDE model of functional restoration, physical capacity assessment implies the assessment of the injured musculoskeletal spinal region, generally involving quantification through reproducibility of mobility, strength, and endurance of a given functional unit or around a given joint. On the other hand, the term functional capacity assessment implies measurement of a functional unit’s change from a normative data curve in the context of whole-person performance—taking compensatory strategies into account in tasks that are specifically designed to stress the injured body part (e.g., weight lifted, running speed, sitting tolerance time). Recent literature has focused on prefunctional and postfunctional restoration longitudinal measurements of patients, as well as on development of specific normative databases.39–45 Aided by a new generation of quantitative tools and an evidence-based consensus on techniques for FCE, a reproducible, prognostic FCE is now possible, even for the difficult chronic pain patients.17,46 This innovation permits an individual patient’s comparison with both normative data and an absolute job requirement for materials handling and positional tolerances.
As implied earlier, the demonstrable success of a sports medicine approach to rehabilitation and reconditioning is not possible without specific quantification techniques. In the 65 years since Delorme’s groundbreaking work in 1945, we have learned much about the secondary physical changes accompanying immobilization and disuse in the spine and extremities.47,48 Spontaneous healing or physician intervention may produce maximum recovery of disrupted soft tissues (ligaments, tendons, joint capsules, muscles, and discs) or osseous tissue in a relatively short 6- to 12-week time period. In cases of severe injury, permanent tissue changes often remain after maximal recovery in the form of distorted bony structures, soft tissue defects, or scar, which may possess strong but more easily reaggravated fibrous properties. In the musculoskeletal system, these changes may create further biomechanical derangements of normal functioning through stress risers, instability, and degenerative joint changes. These problems are to some extent permanent derangements, and they can never be completely fixed. Efforts of acute conservative care, surgery, and manipulation may be directed toward correcting or ameliorating these derangements to the greatest extent possible. However, the province of the tertiary rehabilitation team is to instead tap the body’s inherent, evolutionarily engineered, redundancy; coaxing forth functional compensatory mechanisms in the face of permanent structural change.
Range-of-Motion Assessment
Trunk motion is a compound movement combining intersegmental spine and hip motion components. A patient with a completely fused spine can often bend forward to perform toe touches using hip motion alone. Although it is difficult to measure intersegmental motion nonradiologically, inclinometers may be used to separate the hip motion component from the lumbar spine motion component and derive valuable information.49,50 The basic information on inclinometry comes from British rheumatology, and the system has been used, in one form or another, in Europe for nearly 40 years.51 As in all physical capacity measures, range-of-motion information is only useful when compared with a normative database and contextualized by an identifiable effort factor. For lumbar range of motion, the effort factor is the comparison between the hip motion component and the spine straight leg raise test measurement.50,52 These measurements are isolated anatomic/physiologic physical capacity measurements, assessing the capabilities of a single functional unit of the body. It is these isolated functional unit measurements that ultimately supply context to general functional or whole body measurements taken when a synthetic task such as bending, climbing, or lifting is performed.
In addition to sagittal movement of the spine, coronal movement can be assessed by rotating the inclinometer 90 degrees in the axial plane. Rotation may also be assessed where it is important, namely in the cervical and thoracic spines, through relatively simple techniques.53 The greater the limitation of ROM in any given direction, the less reliable the test. However, if done in a standardized fashion with good effort, these quantitative measurement techniques are highly reproducible, giving both the patient and the interdisciplinary team insight into the weak link.
The multi-inclinometer measurement techniques can demonstrate the actual ROM in the T12-S1 segment in the sagittal and coronal planes, as well as the T1-T12 sagittal/torsional movement, or the occiput-T1 cervical movement in all three planes. Functional assessment aids the rehabilitation process, and in cases of arbitrating disputed compensation it can be used for impairment evaluation purposes. As stated earlier, these tests can also be performed at multiple time intervals to document progress. Suboptimal effort in this portion should lead to careful scrutiny of other components of the functional capacity test battery and trigger greater team involvement. However, even in the presence of poor effort, the determination of “normal” or “abnormal” motion can be made by comparing the spine and hip motion ratios. In the normally mobile lumbar spine the sequence of forward bending generally involves spinal flexion before initiation of the hip flexion component, which proceeds until the spine is “hanging on its ligaments.” At this point, hip motion increases while further spine motion is constrained.50 If, even in the presence of suboptimal effort, a normal spine/hip ratio exists, the clinician can usually conclude that normal spine mobility would have been present if the patient had provided sufficient effort. However, in the presence of an abnormal spine/hip ratio, with or without good effort, actual limitation of spine mobility is likely present (postfusion ankylosis or postoperative/disuse scarring or stiffness). The technique is also important in the work capacity evaluation whether or not the patient completes the interdisciplinary functional restoration program. ROM assessment is usually included as one part of the quantitative functional evaluation, a specific battery of quantitative, internally validated physiologic tests for mobility, strength, endurance, and synthetic task performance.20,52,54 There may be initial resistance to use of measurement techniques by the interdisciplinary team because of concerns about the testing being time consuming, equipment intensive, and cumbersome. With mechanical devices (such as inexpensive carpenter’s levels), two inclinometers must be used simultaneously and the calculations done by hand after measurements are taken. The advantage of versatility and internal calculation (at greater expense) is provided by computerized devices. Once mastered, both techniques are less time consuming than obtaining blood pressure but are far more useful in this population where physician measurements replace the overlimiting, dysfunctional, inhibitory belief that stems from the patient’s perception of pain. Many medical specialists will prefer to perform the tests themselves, though these measurements are often competently performed by well-trained therapists, nurses, or technicians.
As in all other physiologic measurements, there is variation within the asymptomatic population. Interestingly, our normative data show that mean true lumbar motion is almost the same in males and females, even though females tend to have greater hip and straight leg raising mobility components. Patient values are expressed as a “percent normal” as related to mean scores of the symptomatic subject population, normalized for variables like age, gender, and body weight (when applicable).41–43 The system allows the clinician to judge the significance of small variations from the anticipated value and, more importantly, to track the progress of the rehabilitation process between examinations.
Isolated Trunk Strength Assessment
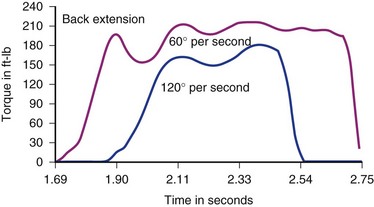
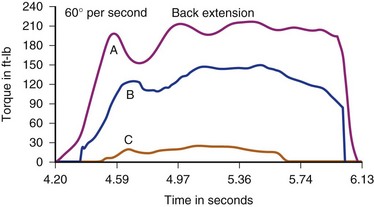
Several devices are commercially available for assessing isometric, isotonic, or isokinetic trunk strength in various planes of motion. Most involve some type of pelvic stabilization with application of force through a line projecting between sternum and scapulae and thus represent trunk strength as torque (torsional force) around a pelvic fulcrum with a lever arm individualized to a subject’s height. Cervical dynamic strength measurement devices have been seen in prototype form, but are not currently available, leaving isometrics as the only alternative. Isokinetic devices stabilize the variables of acceleration and velocity in order to provide torque as the primary independent variable. Isokinetic testing narrows the Gaussian distribution of values by limiting the number of independent variables, which, in our opinion, provides a more valid test. Other available devices may be purely isometric or isoinertial. For historic interest, isometric test models employing strain gauges have been used for more than 60 years. Though commercially available, dynamic, isokinetic trunk strength testing has only been available since 1985, there is abundant literature demonstrating efficacy in identifying isolated motion-segment dysfunction (differentiating weakness and/or decreased endurance) and quantifying outcome improvements. Only a few commercially available isometric or isokinetic devices still exist. PRIDE currently uses a dynamometer connected to a sagittal semi-seated torso testing device detailed in the latter half of Chapter 5 in which lumbar muscle anatomy and function are discussed (Fig. 107–1).
Results of normal subject testing have been compared with chronic spine disorder (CSD) patients, with and without prior surgery.42,43,55–58 Substantial differences have been shown between these groups, initially with incremental trunk strength improvement demonstrated during rehabilitation of chronically disabled spine pain patients (Figs. 107-2 and 107-3).18–2057 The intent of all of the devices is to isolate and challenge the trunk strength component of the thoracolumbar functional unit by stabilizing above and below the area to be tested. The isolation of the vulnerable “weak link” portion of the vertebral biomechanical chain linking the shoulder girdle to the pelvis is intended to assess muscle strength and endurance, just as measuring quadriceps and hamstrings is of prima facie importance to knee function. For any of the devices to be useful, the dynamometer must give accurate and reproducible measurements and the testing protocol must conform to the one employed when the normative database was created. Moreover, such a database must be available to express the individual’s results as a “percent of normal” and the clinician must have a method for assessing effort-validity of each test.
< div class='tao-gold-member'>
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree