Chapter 19 Functional bracing of selected upper limb fractures
Functional fracture bracing is a philosophy of fracture care predicated on the premise that rigid immobilization of fractured limbs is unphysiologic and detrimental to fracture healing and that physiologically induced motion at the fracture site enhances osteogenesis.6,21,25
After extensive human and animal experimentation,10,16,19,20–22,25 we concluded that, contrary to popular belief, closed fractures in the two segments of the body with two long bones experience the maximum and final shortening at the time of injury.21,22,25,26 For example, a closed fracture of the tibia and fibula or of both bones of the forearm that demonstrates an initial shortening of 0.5 cm does not shorten any further after introduction of graduated weight-bearing ambulation or active use of the injured extremity. This fact contradicts the long-held perception that weight bearing on a fractured extremity causes additional and progressive shortening.
Functional bracing is predicated on the premise that physiologically induced motion at the fracture site is conducive to osteogenesis; therefore, immobilization of joints adjacent to the fracture and rigid fixation of fragments are detrimental to fracture healing.6,26 It also is based on the realization that anatomical restoration of alignment is not necessary in the management of most diaphyseal fractures. Minor shortening, angulation, and rotation are not functional complications but simply inconsequential deviations from normal.
Functional bracing of diaphyseal humeral fractures
Rationale
The most widely accepted treatment of the majority of humeral fractures is functional bracing.1,3–5,7,17,23,28,30–32
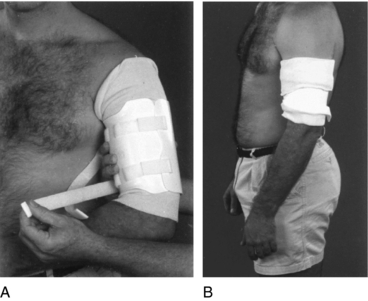
In order for a patient with a humeral fracture to truly benefit from bracing, he or she must be able to assume the erect position, cooperate with the physician, and be capable of adjusting the brace or have someone available who can provide that service on a regular basis. These are requirements because dependency of the extremity is necessary for restoration of adequate alignment of the fragments (Fig. 19-1) and because, during the early days, the brace must be adjusted several times daily as swelling decreases and muscle atrophy takes place.
Management
Open fractures associated with major soft-tissue damage and significant displacement between the fragments require surgical debridement of the wound and some type of stabilization. In these instances, external fixation or plating often is the treatment of choice. Many prefer plating when the fracture is associated with a proven laceration of a major nerve or artery injury. Intramedullary nailing also may be an appropriate treatment under those circumstances, although the complication rate from nailing is high. However, if the soft-tissue damage is not major and there is no vertical distraction between the main fragments, functional bracing can be used effectively.
Manipulation of a diaphyseal fracture of the humerus is strongly criticized because of the danger of producing nerve damage. Most angular deformities correct spontaneously as the brace compresses the soft tissues and the weight of the arm assists in improving alignment (Fig. 19-1). Most angular deformities are physiologically and cosmetically tolerated. In rare cases when an unacceptable deformity persists, a surgical intervention is required.
Brace application
Whenever possible, the cast should be removed with the patient sitting on a high table. The brace is applied in the same position. After the arm is cleansed, a layer of stockinette is carefully rolled over the extremity, extending from just below the elbow to the level of the acromion process (Fig. 19-1). The appropriate size of brace is selected by measuring the length of the upper arm from approximately 1 inch below the axilla to 1 inch above the lateral condyle of the humerus.
The collar and cuff are applied holding the elbow at 90 degrees. Exercises similar to those carried out during the cast immobilization period should continue. At first, the exercises should be passively assisted with the opposite hand. As soon as the patient realizes that the passive motion of the shoulder is not associated with pain, he or she should begin to combine the passive motion with active contraction of the biceps and triceps. The contraction of the flexors and extensors of the elbow assists in the correction of rotary deformities. This is possible because the two muscle groups have attachments to the proximal and distal fragments of the fracture. The malrotation of the bones at the time of the injury is accompanied by a parallel coiling of the muscles. Once they contract, they correct the rotary bony deformity.21
Patient instructions
The exercises of the extremity should not be limited to the shoulder and elbow; they should include the hand and wrist. In this manner swelling is decreased. The arm must hang loosely at the side of the body so that gravity forces can assist in correcting the angular deformities. Leaning on the elbow should be strongly discouraged because it produces angular deformities. This may occur during the initial period of cast immobilization but more likely after application of the brace.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree