Fig. 2.1
(a) Motor area, (b) sensory area; 1 palm, 2 small finger, 3 ring finger, 4 long finger, 5 index finger, 6 thumb, 7 head, 8 eye, 9 face, 10 tongue, 11 lip, 12 neck, 13 arm, 14 lower leg, 15 genitals, 16 upper leg, 17 foot, 18 toes, 19 eyebrow, 20 eyelid/eyeball, 21 jaw, 22 wrist, 23 hand, 24 arm, 25 body, 26 ankle, 27 foot (G. Chick © 2012, all rights reserved)

Fig. 2.2
Large, oval objects as handballs are held by both extrinsic and intrinsic muscle groups

Fig. 2.3
Grasping the light ping-pong ball without squeezing it shows perfect interaction of skin mechanoreceptors, brain, nerves, and muscles of the hand
This chapter deals with understanding the mechanisms of how the hand and the digits work together in order to be able to create a picture of a hand as a whole and in specific its role as a most creative part of a locomotor apparatus of the human body. The chapter is divided to different sections: the section of osseous anatomy, the section of anatomy of finger joints, muscle, and tendons section, and the section of nerves and arteries of the hand.
2.1.2 Osseous Anatomy of the Long Fingers and the Thumb
The hand and wrist contain 27 bones: 14 phalanges, 5 metacarpals, and 8 carpal bones [2]. Every long finger has three phalanges: the proximal, the middle, and the distal phalanx. The thumb has only two phalanges: the proximal and the distal. Besides, there is a pair of the sesamoid bones, most commonly placed on the volar part of the thumb by the first metacarpophalangeal joint (MCP 1) and on the volar part of small finger by the fifth metacarpophalangeal joint (MCP 5). Every phalangeal bone is built according to principles of the long bones: the diaphysis in the middle, the proximal and distal metaphysis, and the proximal and distal epiphysis (Fig. 2.4). Every proximal and middle phalanx, as well as metacarpal bone, has a basis, a shaft, and a condylar part, while a distal phalanx has a basis, a shaft, and a relatively broad ungual process which sustains a good bed for the matrix of the nail on its dorsal side. The nail has a keratin structure and gives a good protection to the fingertip. Condylar part of the proximal and distal phalanges is different compared to metacarpals: they have radial and ulnar condyle; the metacarpal has just one condyle, also called a head of the metacarpal bone. Both the volar and the dorsal surfaces of the phalanges and metacarpal bones are hollowed or humpy in order to sustain the soft tissue in its very nearness. The bony structures of the hand primarily support the flexor and extensor tendons on their way, give an origin to intrinsic muscles of the hand, and form joints in order to give motion and stability and to contribute to strength of the entire hand.
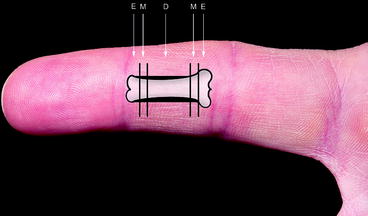
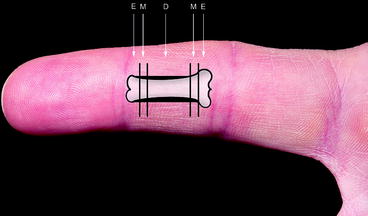
Fig. 2.4
E epiphysis, M metaphysis, D diaphysis
The carpal bones are placed in the two different rows: the distal row which articulates with metacarpals and the proximal row which articulates with the radius and ulna and the distal radioulnar joint. The distal row, from radial to ulnar, contains the trapezium, trapezoid, capitate, and hamate. The proximal row includes the scaphoid, lunate, triquetrum, and the pisiform (Fig. 2.5).


Fig. 2.5
X-ray (P-A) of the bones of the hand and the wrist: Tm trapezium, Td trapezoid, C capitate, H hamate, S scaphoid, L lunate, Tri triquetrum, P pisiform
2.1.3 Anatomy of the Finger Joints
Between bony structures of the hand, there are finger joints that look like any other joint with a cartilage cover of the bony ends and joint capsule both on the volar and the dorsal sides, together with ligament structures which are necessary to obtain stability and strength of the joint structures.
Starting with carpometacarpal joints (CMC joints), they all correspond the specific distal carpal row bone as explained previously. The CMC 1 joint is a joint bearing the thumb with all its uniqueness. The first metacarpal is in pronation compared with other metacarpals, and the CMC 1 joint corresponds to the trapezium which has a saddle-formed shape. This permits abduction of the thumb (normal range 0–60°), volar abduction (normal range 0–60°), extension (normal range 0–50°) and adduction which means return of the thumb from abduction back along the palm [3]. The CMC 1 joint is the most mobile CMC joint and it allows both pinch and the key grips of the thumb. There are many ligament structures in this joint, the strongest placed on the volar side of the joint. The CMC 2 joint articulates to the ulnar facet of the trapezium, trapezoid, and the radial facet of the CMC 3 joint. The CMC 3 joint articulates at the bottom with the capitate and at sides with corresponding metacarpals. The range of motion of the CMC 2 and CMC 3 is limited by strong intrinsic ligament structures and stiffed joint capsule. Both the CMC 4 and CMC 5 articulate with underlying hamate and with each other and for the case of the CMC 4 with the ulnar facet of the CMC 3. The range of motion is greater here, and 5–10º of flexion is possible at CMC 4 and 15–20º at CMC 5.
At the level of the metacarpophalangeal joints (MCP joints), a strong fibrous volar-placed accessory ligament (volar plate) is the most stabilizing factor together with a collateral ligament structures on both radial and ulnar sides (Fig. 2.6). Besides, there are transverse volar ligament structures connecting all MCP joints from MCP 2 to MCP 5. The range of motion here is from 0º to approximately 55º for the thumb and from 0º to approx. 90º for the rest of the MCP joints. The MCP joints can be passively extended by up to 45º. Intrinsic muscles of the hand are contributing to stability of the MCP joints.
Fig. 2.6
MCP joint: Transverse section. 1 Extensor tendon, 2 metacarpal bone, 3 collateral ligament, 4, 5, and 6 dorsal and palmar interossei, 7 volar plate, 8 and 9 transverse volar ligaments, 10 lumbrical muscle, 11 annular pulley, 12 superficial flexor tendon, 13 deep flexor tendon (G. Chick © 2012, all rights reserved)
As concerns proximal interphalangeal joints (PIP joints), they are also stabilized by the strong volar plates and collateral ligaments on each side. The normal range of motion in the PIP joints is 0–100º of flexion. Distal interphalangeal joints (DIP joints) have a similar ligamentous anatomy as the PIP joints, but the range of motion is lesser (approximately 0–80º of flexion). The interphalangeal joint of the thumb (IP joint) can normally be flexed 80º and extended 20º.
There are other ligament structures which do not belong to joints alone and which have location in the soft tissues of the finger. Such examples are the Grayson’s ligament, the Cleland’s ligament, and the septa of the fingertip. The Grayson’s ligament originates at the flexor tendon sheet and inserts into the skin, anterior to the neurovascular bundle. Cleland’s ligament goes from the finger bone to the skin dorsal to the neurovascular bundle and is located only between the middle phalanx and the DIP joint. The fibrous septa of the fingertip are connections between ungual processes of the distal phalanx and the skin creating a stronger fingertip, more useful in the activity of grasping, touching, pushing, etc. (Fig. 2.7).
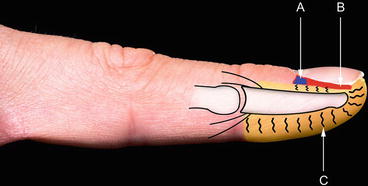
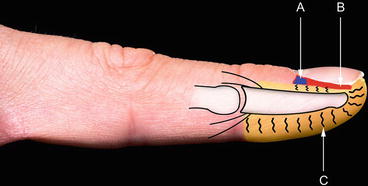
Fig. 2.7
(A) Nail matrix, (B) nail bed, and (C) fibrous septa between fat tissue and skin mechanoreceptors
2.1.4 Tendons and Muscles of the Hand
Muscles of the hand are situated either in the hand itself (intrinsic muscles) or in the forearm with their tendons going distally to the hand (extrinsic muscles).
The extrinsic muscles of the hand divide into two major groups: flexors and extensors.
Flexors muscles are situated on the volar side of the forearm, while extensors lie on the dorsal side. Both groups of muscles become tendons at the level of the wrist and distally. All flexors together with median nerve pass the wrist through a bony canal which is covered by a hard top – carpal transverse ligament forming a carpal tunnel. Some of the flexor tendons don’t go through the carpal tunnel: flexor carpi radialis (FCR) inserts on the volar aspect of the second metacarpal base. FCR flexes the wrist in volar and radial direction. Flexor carpi ulnaris (FCU) surrounds the pisiform bone, flexing the wrist in volar and ulnar direction. Palmaris longus muscle (PL), which lacks in some people, makes broad palmar aponeurosis and contributes in the flexion function of the wrist and grasping strength of the hand (Fig. 2.8).
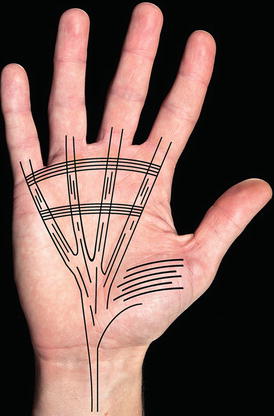
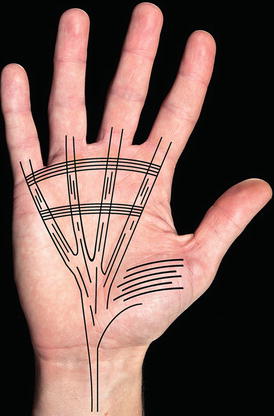
Fig. 2.8
Palmaris longus muscle is a part of palmar aponeurosis
From the carpal tunnel, all the other flexor tendons go to the respective fingers, starting from radial with flexor pollicis longus (FPL) going to the distal phalanx attaching to its volar base, flexing the IP joint of the thumb. Flexor digitorum profundus tendons (FDP) go to the respective ulnar fingers crossing the chiasm at the level of MCP joints where they come up aside of, and finally volar to the flexor digitorum superficialis tendons (FDS) inserting the distal phalanx and flexing the DIP joint. The superficial flexor digitorum tendon ends with two snips on the middle phalanx and flexing the PIP joint. Some 30 % of the population lacks the FDS tendon of the fifth digit. Five annular and three cruciate pulleys (fibrous bands) hold the flexor tendons forming the synovial sheath (Fig. 2.9). Annular pulleys are stronger and play the role in preventing the bowstringing of the fingers, while cruciate pulleys are weaker and permit the fingers to bend. The annular pulleys are named A1 to A5 going from proximal to distal and cruciate pulleys – C1 to C3. The most important pulleys for finger function are A2 and A4. The thumb has only two annular pulleys A1 and A2 and an oblique pulley (O) which is the most important. The flexor tendons get their vascularization partly by structure of vincula, which are some folds of mesotenon, leading vascular perfusion from the bone to the tendons, partly from diffusion of the synovial fluid from the tendon sheet. All flexor tendons are divided on the palmar surface into 6 zones as shown on the Fig. 2.10. Zone 2 is also called a “no man’s land,” meaning that repair of tendons in this zone needs more surgical expertise and meticulous operative technique.
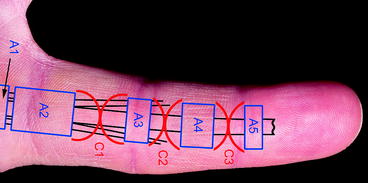
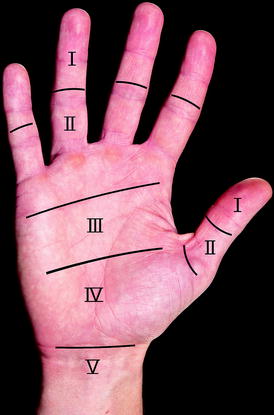
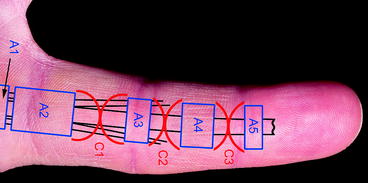
Fig. 2.9
A annular pulleys, C cruciate pulleys
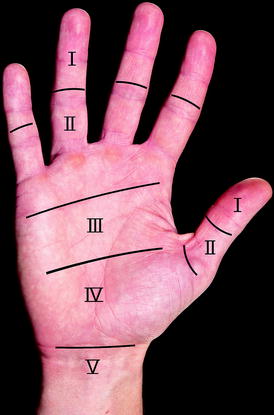
Fig. 2.10
Sixth flexor tendon zone is situated further proximally; the thumb has only two zones
The extensor tendons of the hand pass the wrist on the dorsal side protected by an extensor aponeurosis [4]. They divide in the six compartments containing isolated tendons or tendons in pair or a group of several tendons as described here from radial to ulnar (Fig. 2.11):
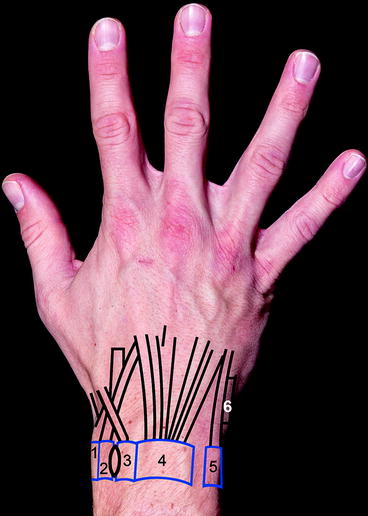
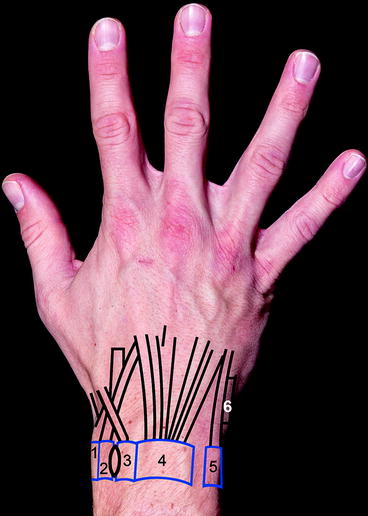
Fig. 2.11
Six extensor tendon compartments
1.
Abductor pollicis longus (APL), Extensor pollicis brevis (EPB)
2.
Extensor carpi radialis longus (ECRL), Extensor carpi radialis brevis (ECRB)
3.
Extensor pollicis longus (EPL)
4.
Extensor digitorum communis (EDC), Extensor indicis proprius (EIP)
5.
Extensor digiti minimi (EDM)
6.
Extensor carpi ulnaris (ECU)
By the level of the dorsum of the hand, the extensor tendons are being held together with transverse tendon structures responsible for their gliding function over the central portion of the MCP joints. By the level of the MCP joints, the extensor tendons form extensor aponeurosis, a broadening expansion of the tendon fibers towards the metacarpal sides together with intrinsic muscles of the dorsal interosseous muscle. Going further distally, it forms a sagittal band between tendon and lumbrical muscles (Fig. 2.12). Central slip of the extensor tendon has its insertion to the middle phalanx at its dorsal basal slip, extending the PIP joint, while two lateral bands go further distally inserting the dorsal portion of the distal phalanx, extending the DIP joint. The extensor tendons of the hand are more exposed to injuries than flexor tendons partly because of their close relation to the skin and bone, partly because of their lesser thickness.
Fig. 2.12
1 Distal phalanx, 2 lateral bands, 3 dorsal digital expansion, 4 central slip of EDC tendon, 5 sagittal bands, 6 extensor aponeurosis, 7 transverse volar ligaments, 8 and 10 dorsal interossei, 9 lumbrical muscle (G. Chick © 2012, all rights reserved)
The intrinsic muscles of the hand contain the muscles of the thenar, the hypothenar, the interosseous muscles, and the lumbricals (Figs. 2.13 and 2.14).
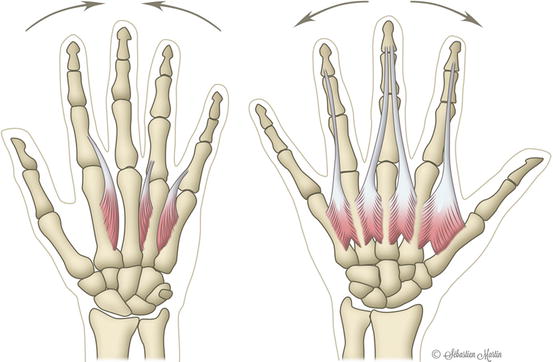
Fig. 2.13
1 M. adductor pollicis (AP), 2 M. flexor pollicis brevis (FPB-superficial head), 3 M. opponens pollicis (OP), 4 M. abductor pollicis brevis (APB), 5 M. flexor digiti minimi, 6 M. abductor digiti minimi, 7 M. opponens digiti minimi, 8 M. flexor carpi ulnaris (G. Chick © 2012, all rights reserved)
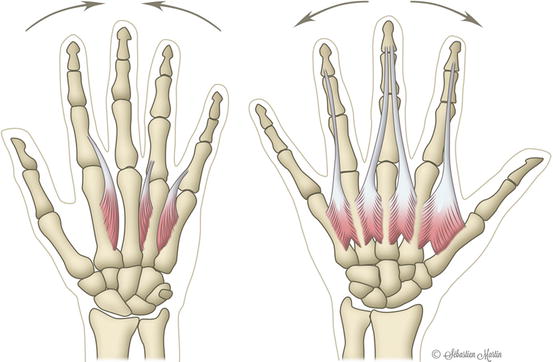
Fig. 2.14
Palmar interossei gather the fingers, and dorsal interossei spreads the fingers (G. Chick © 2012, all rights reserved)
Going from radial to ulnar, the muscles of thenar are as follows: M. opponens pollicis (OP), M. abductor pollicis brevis (APB), M. flexor pollicis brevis (FPB)-superficial head, M. flexor pollicis brevis (FPB)-deep head, and M. adductor pollicis (AP). Their origin is on the volar sides of the carpal bones, and its insertion is mostly the volar and radial portions of the MCP 1 joint. These muscles are responsible for the movement of the thumb in the direction of their respective names.
The lumbrical muscles (four muscles) originate on the radial side of the FDP tendon and insert on the radial lateral band of the extensor aponeurosis. The lumbricals flex the MCP joint and extend the PIP joint. The dorsal interossei originate on the side of the metacarpal shaft and insert as tendinous slips at different levels of the fingers. The four of dorsal muscles are responsible for abduction of the index, middle, and ring fingers, while the three palmar interossei adduct the index, ring, and small fingers together with assisting the MCP joint flexion and PIP and DIP joint extension. There are three muscles of hypothenar: M. abductor digiti minimi with its origin from pisiform bone, M. opponens digiti minimi, and M. flexor digiti minimi.
2.1.5 Arteries and Nerves of the Digit and Hand
The hand vascularity is supplied by radial and ulnar arteries and their anastomosis which represents the deep and the superficial palmar arches. The deep palmar arch lays approximately 1 cm proximal to the superficial palmar arch (Fig. 2.15). The deep palmar arch is the predominant supplier of the blood to the thumb and radial aspects of the index finger, while the superficial palmar arch supplies the rest of the digits making three common digital arteries. The vessels of these arches supply both the volar and the dorsal aspects of the hand. The dorsal side is thought supplied furthermore by some vessels from the A. interossea. Arteries on the dorsum of the hand are metacarpal arteries which can play important role in the treatment of eventual skin defects and defect covering by island flaps.
Fig. 2.15
1 Cubital arterial branches, 2 A. interossea communis, 3 A. ulnaris, 4 A. radialis, 5 A. interossea anterio, 6 superficial arterial branch, 7 deep arterial branch, 8 thumb artery, 9 index artery, 10 deep palmar arch, 11 superficial palmar arch, 12 common digital artery, 13 digital artery (G. Chick © 2012, all rights reserved)
Stereognosy is the process responsible for gathering and conducting the tactile information from the skin of the digits and the palm. Fingertips and a skin of the entire hand are supplied by many mechanoreceptors. The skin mechanoreceptors are crucial for the tactile function of the hand and are divided in “fast-adapting” and “slowly adapting” receptors (Fig. 2.16). The “fast-adapting” receptors are reacting on dynamic pressure changes from the skin such as vibration and skin friction (the bodies of Meissner and Pacini). The “slowly adapting” receptor reacts on static load such as contact with angle contours (the bodies of Merkel and Ruffini). The sensory receptors are conducting the impulses to the nerves of the digits and hand in order to regulate the exact amount of the gripping force. The signals are conducted to the spinal cord and the brain where processing occurs resulting in sending back signals to the spinal cord and to the motor neurons. This leads to explanation that the nerve system is divided in sensory and motor divisions. The sensory division contains the sensory nerve fibers responsible for conduction of the impulses from the receptors to the central nervous system (CNS) and the motor division containing motor nerve fibers responsible for the conduction of the impulses in the opposite direction – from the CNS to the effectors (the muscles and the glands).