I. Introduction—Osteoporosis and resulting hip fractures have a substantial economic and social impact. It is estimated that worldwide, 323 million people suffer from osteoporosis and that number is projected to be 1.55 billion by the year 2050. It has been predicted that the number of hip fractures in the year 2050 will be 6.3 million. Despite improvements in patient care and operative technique, hip fractures account for a significant amount of health care expenditure.
II. Femoral Neck Fractures
A. Overview—Femoral neck fractures are intracapsular fractures that occur in the region from just above the intertrochanteric region to just below the articular surface of the femoral head. There is a bimodal distribution of femoral neck fractures, with the majority occurring in the geriatric population from low energy falls, and a smaller number occurring in younger individuals from high-energy mechanisms. The approach to treatment is different in these two groups, in that an attempt is made to reduce and fix almost all femoral neck fractures in young adults, while most displaced fractures in elderly patients are treated with arthroplasty.
B. Evaluation
1. Physical examination—If a patient is suspected of having a femoral neck fracture, range of motion of the hip should be avoided until radiographs of the proximal femur have been obtained, to avoid displacement of the fracture. Patients who have a displaced femoral neck fracture will present with the affected leg in a shortened and externally rotated position. With nondisplaced fractures, the injured extremity lacks these obvious deformities.
• Elderly population—In elderly patients who have sustained a fall and resulting hip fracture, the cause of the fall should be elucidated. Nonmechanical reasons for falling such as syncope, presyncope, myocardial infarction, and stroke are all possible etiologies. The patient should be evaluated for other injuries. The distal radius and proximal humerus are regions commonly affected by osteoporosis, and should be evaluated for possible fracture.
• Younger population—Hip fractures in younger patients typically result from high-energy mechanisms. These patients require a complete primary and secondary survey with special attention paid to the ipsilateral femoral shaft. Approximately 2.5% of femoral shaft fractures are associated with an ipsilateral femoral neck fracture.
2. Radiographic evaluation—The standard radiographic evaluation for patients suspected to have a hip fracture includes an anteroposterior (AP) view of the pelvis and hip and a cross-table lateral view of the hip. The AP pelvis view allows for comparison with the contralateral hip; this comparison may reveal subtle impaction or fracture displacement. The cross-table lateral is preferred to the frog lateral, since the latter can result in increased pain and fracture displacement. Ideally, the AP hip view should be obtained with the hip in 15° of internal rotation to compensate for the anatomic anteversion of the femoral neck and provide an en face view of the proximal femur. This view can help diagnose nondisplaced fractures. If all radiographs appear normal but the clinical suspicion for hip fracture is high, a technetium bone scan or magnetic resonance image (MRI) should be obtained (Fig. 5-1). The MRI is sensitive for occult hip fracture within 24 hours, whereas the bone scan may take 48 to 72 hours to demonstrate the fracture.

FIGURE 5-1 T1-weighted MRI showing a nondisplaced femoral neck fracture.
C. Injury Classification—The Garden classification is commonly used and consists of four grades: Grade 1 is an incomplete or valgus impacted fracture, Grade 2 is a complete and nondisplaced fracture, Grade 3 is a partially displaced fracture, and a Grade 4 is completely displaced (Fig. 5-2). The risk of nonunion and osteonecrosis is substantially higher for Grades 3 and 4. The Pauwel classification is based on the angle formed by the fracture line and a horizontal line with simulated standing. Pauwel’s classification consists of three types: Type 1 has an angle less than 30°, Type 2 has an angle between 30° and 50°, and Type 3 has and angle greater than 50° (Fig. 5-3). The more vertical the fracture line is, the higher the Pauwel’s angle, and the higher the shear forces across the fracture.
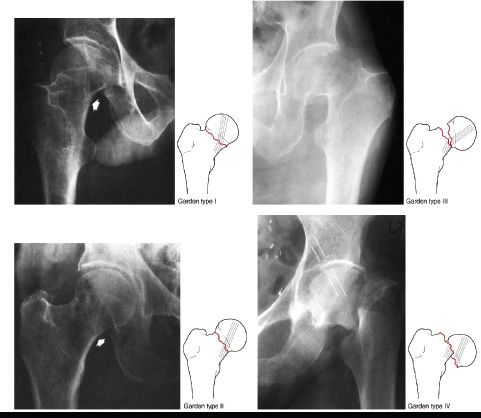
FIGURE 5-2 Garden’s classification of femoral neck fractures. (From Keating J. Femoral neck fractures. In: Bucholz RW, Heckman JD, Court-Brown C, et al., eds. Rockwood and Green’s Fractures in Adults. 7th ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2010, with permission.)
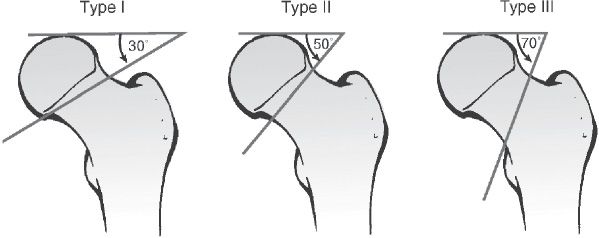
FIGURE 5-3 The Pauwel classification of femoral neck fractures is based on the angle the fracture forms with the horizontal plane. As fracture type progresses from Type 1 to Type 3, the obliquity of the fracture line increases and, theoretically, the shear forces at the fracture site also increase. (From Keating J. Femoral neck fractures. In: Bucholz, RW, Heckman JD, Court-Brown C, et al., eds. Rockwood and Green’s Fractures in Adults. 7th ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2010, with permission.)
1. Elderly population—In elderly patients a cerebral vascular accident or myocardial infarction may precipitate the fall resulting in fracture. Common associated injuries include distal radius and proximal humerus fractures. Closed head injury such as subdural hematoma can also result from a fall.
2. Younger population—In young patients the high-energy mechanisms can result in associated orthopaedic injuries of the ipsilateral tibia, femur, and pelvis/acetabulum. Injuries to the head, chest, and abdomen are also common.
E. Treatment Options and Rationale
1. Nonoperative treatment—Nonoperative treatment is generally limited to elderly nonambulators who are considered too high risk for surgery or who have minimal pain with mobilization. The goal for these patients should be early bed to chair mobilization in attempt to limit the complications of prolonged recumbence: atelectasis, thromboembolic disease, urinary tract infection, and decubitus ulcers.
2. Operative treatment
• Timing of surgery—Patients should undergo surgery as soon as they are deemed medically stable. In elderly patients, surgery may need to be delayed until fluid and electrolyte imbalances are corrected. Recent studies have shown some benefit to the model of orthopaedic and geriatric medicine cocare in reducing complications such as delirium and improving survival. In young patients, displaced femoral neck fractures are treated emergently with ORIF to help reduce the risk of osteonecrosis.
• Anesthetic considerations—For patients unable to undergo early surgery, femoral nerve block catheters should be considered to assist in pain control and limit narcotic use in the elderly. Studies have not shown a consistent difference in perioperative mortality with general versus regional anesthesia.
• Nondisplaced femoral neck fractures—Recommended treatment for nondisplaced femoral neck fractures consists of internal fixation with multiple lag screws placed in a parallel fashion. Either three or four screws should be used. If three screws are used, an inverted triangle pattern can be used with the inferior screw adjacent to the inferior neck and the posterior superior screw adjacent to the posterior femoral neck.
(a) Open capsulotomy—Some authors have recommended open capsulotomy for nondisplaced femoral neck fractures, with the theory that capsulotomy relieves pressure from the intracapsular hematoma and in turn reduces the risk of osteonecrosis. Controversy exists as to whether capsulotomy actually lowers the rate of osteonecrosis; however, it does have its advocates, especially for young patients. Prior to surgery, allowing the leg to assume a flexed, abducted, and externally rotated position has also been shown to decrease intracapsular pressure.
• Displaced femoral neck fractures—Treatment of displaced femoral neck fractures largely depends on the patient’s age and activity level. In younger patients, closed or open reduction is performed followed by internal fixation (Fig. 5-4). The goal is anatomic reduction and it may be necessary to perform either a Smith-Petersen or a Watson-Jones approach to ensure proper reduction. In older, less active patients, most authors recommend prosthetic replacement of the femoral head. Trials comparing ORIF to hemiarthroplasty for displaced femoral neck fractures in the elderly have consistently shown improved outcomes and lower reoperation rates for the arthroplasty group.

FIGURE 5-4 Preop and 3-month postop X-rays of a displaced femoral neck fracture in a 26-year-old man treated with open reduction and internal fixation.
(a) Internal fixation—When internal fixation is chosen, anatomic reduction is essential to try to minimize complications such as nonunion and osteonecrosis. If attempts at closed reduction do not clearly result in anatomic reduction, then open reduction should be performed and fixation achieved typically with multiple parallel screws. For basi-cervical fractures, fixation with a sliding hip screw is another alternative.
(b) Prosthetic replacement of the femoral head—Prosthetic replacement can take the form of either hemiarthroplasty with a monopolar or a bipolar prosthesis, or total hip arthroplasty. The bipolar prosthesis has a theoretic advantage over the unipolar, as the second articulation in the bipolar has been suggested to decrease acetabular wear. In practice, however, it has been shown that the second articulation in a bipolar often ceases to function and it essentially becomes a unipolar construct. Additionally, unlike the monopolar, the bipolar typically has a metal-polyethylene articulation, which, if it does function as designed, can lead to polyethylene wear and osteolysis. For most low-demand elderly patients, the unipolar replacement is the recommended prosthesis (Fig. 5-5).
(c) Total hip replacement—Patients with pre-existing degenerative disease of the hip (i.e., rheumatoid arthritis, Paget’s disease, osteoarthritis) and a femoral neck fracture should be considered for total hip arthroplasty. Some studies have suggested improved outcomes regarding pain and function for total hip arthroplasty compared with hemiarthroplasty even for elderly patients without arthritis. On the other hand, total hip replacement does have a higher dislocation rate and generally should be avoided in patients with dementia who are unable to comply with hip precautions. Patients with neurologic conditions such as Parkinson’s or paralysis from a prior cerebrovascular accident are also at increased risk of dislocation and generally should be treated with a hemiarthroplasty.


FIGURE 5-5 Preop and postop hip radiographs of an elderly patient with a displaced femoral neck fracture treated with hemiarthroplasty.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree






