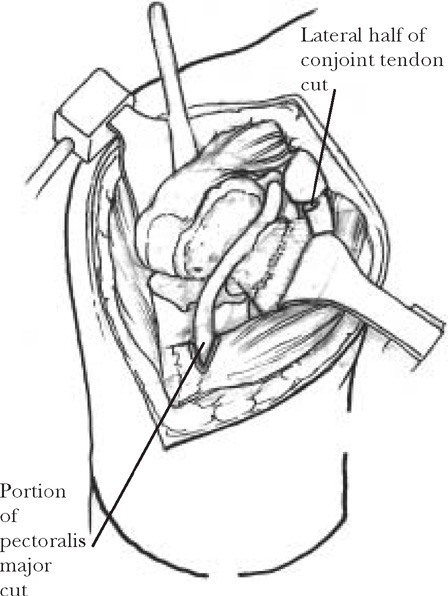
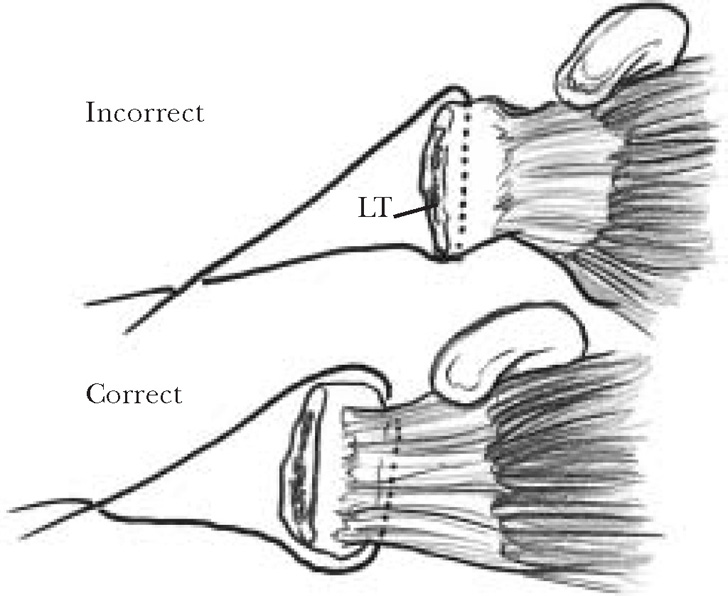
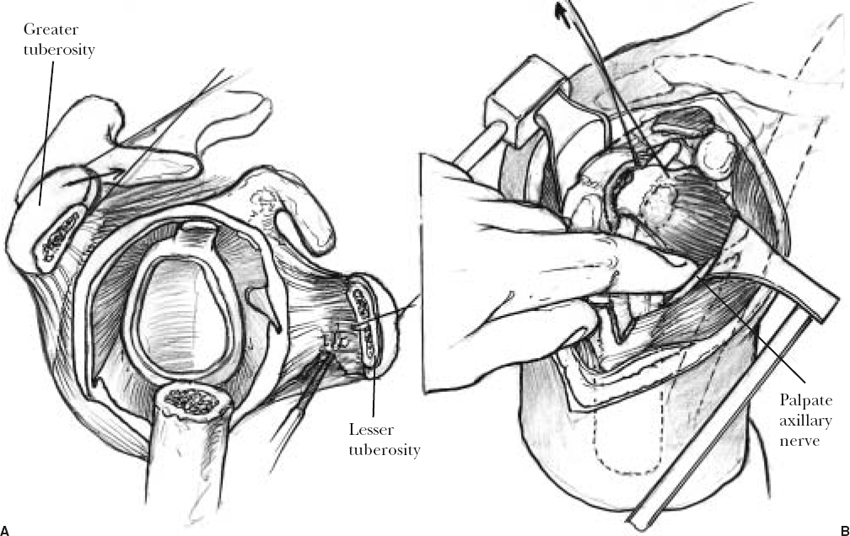
14 The successful management of four-part proximal humeral fractures with prosthetic replacement requires the orthopedic surgeon to identify those patients who meet the criteria for surgery, to perform a technically demanding surgery, and to carefully monitor and guide the postoperative rehabilitation. Failure in any of the above clinical duties may result in a poor clinical outcome following hemiarthroplasty performed for a four-part proximal humerus fracture. This chapter details the indications and contraindications for surgical treatment, provides a step-by-step guide for the surgeon to a correctly sized and positioned hemiarthroplasty, and outlines an effective postoperative rehabilitative protocol. Proximal humerus fractures represent 4 to 7% of all fractures. In 1970, Neer1,2 did not report the incidence of four-part fractures in his large series of proximal humerus fractures; however, 63 of the 300 (21%) cases that required surgical intervention underwent prosthetic replacement. More recently, Robinson et al3 reported that 163 of 3463 (4.7%) proximal humerus fractures required humeral head replacement. The most common mechanism is a fall on an outstretched hand or elbow, although a direct fall on the shoulder may also create a four-part proximal humerus fracture. When considering surgical treatment of a displaced four-part proximal humerus fracture, the patient’s age, lifestyle, bone quality, and coexisting medical comorbidities should be considered. Chronic alcohol abuse and psychiatric illness that is not closely monitored should be considered relative contraindications to hemiarthroplasty. Closed treatment of four-part proximal humerus fractures has resulted in a high incidence of poor outcomes secondary to avascular necrosis, stiffness, and malunion with subsequent poor function.1,4 Open reduction internal fixation of displaced four-part proximal humerus fractures has equally disappointing results, primarily because of the relatively high incidence of avascular necrosis. The vascular anatomy supplying the proximal humerus has been well delineated.5,6 The major blood supply is from the anterior humeral circumflex artery, which flows into its ascending branch and then to the arcuate artery. The posterior humeral circumflex provides a significant blood supply to the medial neck and calcar region as well as a small portion of the posterior inferior articular surface. The incidence of a displaced four-part proximal humerus fracture developing avascular necrosis ranges in the literature from 20 to 100%. Undoubtedly, this range of avascular necrosis results from the varying fracture patterns, amount of part displacement, and subsequent vessel disruption. The development of osteonecrosis is not necessarily a failed outcome. Gerber et al7 noted those patients who develop osteonecrosis often have good function and minimal pain. A functioning shoulder with osteonecrosis may provide a younger patient with a satisfactory outcome for years. However, the results of conversion to a hemiarthroplasty after a failed closed treatment or failed open reduction and internal fixation has been shown to be significantly inferior to that of immediate arthroplasty for four-part fractures.8,9 It is recommended that displaced four-part fractures and fracture dislocations of the proximal humerus in elderly patients be treated with a hemiarthroplasty. If the quality of bone is questionable in a patient in the transition years (50–60 years of age), then a CT scan may provide information regarding bone quality and help avoid failure of open reduction and internal fixation. Hemiarthroplasty is also recommended as the primary surgical treatment in patients with head split fractures and fracture dislocations that have greater that 40% of the articular surface irreversibly damaged. The surgical technique of hemiarthroplasty for a comminuted proximal humerus fracture requires that the appropriately sized humeral component be placed in the correct position and that the tuberosities are securely fixated to one another and to the shaft of the humerus. Nonunion or malunion of the tuberosities results in poor clinical results.10 It is necessary to understand that the tuberosities will not heal to methylmethacrylate or to the implant and that methylmethacrylate should not be placed between the tuberosities. Instead, the area between the tuberosities and shaft should be bone grafted to improve the chances of fracture healing. The technique is broken down into a step-by-step process to avoid technical error in implant positioning and tuberosity repair. The patient is positioned in the semi-reclined position and moved laterally to allow the shoulder to be extended. The neck and the head are well supported and protected by a headrest, and a padded post is placed along the chest wall to maintain the patient on the table. The anterior aspect of the glenohumeral joint is exposed through an extended deltopectoral approach, the incision beginning at the clavicle and extending toward the insertion of the deltoid. The deltoid should not be detached from its origin on the clavicle, as this will weaken it and affect postoperative function. The cephalic vein is identified, preserved, and retracted laterally with the deltoid muscle. The deltopectoral groove is developed bluntly from the clavicle to insertion of the deltoid, and crossover veins are sacrificed. The clavi-pectoral fascia forms the anterior wall of the underlying fracture hematoma. Identification of the lateral border of the conjoined tendon will provide the landmark for incision into the fracture hematoma. Following hematoma evacuation, the clavipectoral fascia is incised longitudinally and superiorly to the coracoacromial ligament, which is identified and preserved. The upper 1 or 2 cm of the tendinous insertion of the pectoralis major is released to improve exposure to the inferior aspect of the joint. The long head of the biceps serves as an important landmark and is identified next. Occasionally, it may be torn or impaled within the fracture site. The tendon is freed and followed into the groove. The roof of the biceps groove is then incised from inferior to superior through the transverse ligament and into the rotator interval using blunt Mayo scissors with the curvature turned toward the coracoid process (Figure 14-1). Two number 2 nonabsorbable simple sutures are then placed, one into the upper border of the subscapularis tendon and an adjacent one into the anterior border of the supraspinatus tendon approximately 1 cm apart. These two sutures will be used to close the rotator interval at the time of tuberosity repair and ensure the preservation of the anatomic relationship of the lesser and greater tuberosities. The glenohumeral joint is then entered and evacuated of hematoma. The fracture pattern is analyzed, and tuberosity position and comminution are identified. Greater tuberosity fracture lines are very helpful in positioning the prosthesis at the correct height, and the anatomic position of the tuberosity is noted. FIGURE 14-1. Opening the rotator interval with scissor tips pointed medially. The interval relationship is maintained by placing two sutures, one into the subscapularis and one into the supraspinatus. Tuberosity fixation is a critical aspect of prosthetic replacement in three- or four-part fractures. Tuberosities are to be handled with care to avoid further comminution. Nonabsorbable braided sutures, such as 1 mm wide Dacron tapes (Deknatel, Fall River, MA), or number 2 Fiberwire (Synthes, Naples, NL) are used to suture the tuberosities to each other, to the component, and to the shaft of the humerus. Place a single suture through the tendon of the subscapularis at the point where the tendon inserts into the bone to isolate the lesser tuberosity. One or two other sutures are then placed from superior to inferior at 1 cm intervals along the infraspinatus tendon insertion to the greater tuberosity. These sutures are used to control the tuberosities, allowing exposure, and are used later for tuberosity fixation. Sutures placed through the tuberosities are at risk for failure because of the osteoporotic nature of the bone; thus, tendon sutures are recommended (Figure 14-2). The greater and lesser tuberosities need to be mobilized from adhesions and scarring that form within 8 hours of injury. The lesser tuberosity is freed from adhesions to the overlying conjoined tendon and the underlying soft tissues (Figure 14-3A). The axillary nerve is identified and protected while mobilizing the tuberosity and the attached subscapularis musculotendinous unit (Figure 14-3B). The greater tuberosity is freed in a likewise fashion, with digital disruption of adhesions to the overlying deltoid and coracoacromial arch. The goal of the tuberosity mobilization is to allow the tuberosities to be mobilized adequately so that they can be reattached to one another and to the humeral shaft. FIGURE 14-2. Suture technique for grasping tuberosities without causing comminution of osteoporotic bone, passing the suture through the adjacent tendon. The humeral head should be removed carefully and employed as a direct template for the humeral head size that will be used. If a head split fracture is present, then the head size can usually be determined from the largest fragment then extrapolated. Several systems have templates for determining head size. The two variables to be determined are head thickness and circumference; if the size of these two variables falls between two different sizes, then the smaller of the two should be chosen to maximize motion.11,12 Head thickness is determined by calculating the distance from the anatomic neck to the apex of the head. This can be done by using calipers or a template or by comparing the removed humeral head to the various available prosthetic heads. The correct head thickness should allow the hand to fall easily to the abdomen or internally rotate to 50 to 60 degrees with the shoulder in 90 degrees of abduction when performing the trial reduction. Using a template or comparing the removed humeral head to available prosthetic trial humeral heads can determine humeral head circumference. The correct head circumference should allow approximately 40 to 50% posterior humeral head translation on the glenoid surface. After the humeral head has been sized, the cancellous bone from the humeral head is removed using a rongeur on the back table. This grafted bone will be used later to promote tuberosity healing to one another and the humeral shaft. The proximal humeral shaft is delivered through the incision by extending the arm. The proximal shaft is then trimmed of sharp bony spicules, and the canal is cleared of bone fragments and blood clots. The humeral canal is lightly reamed with the provided intramedullary reamers. If the system does not have reamers to size the canal, then place the smallest trial humeral component in the intramedullary canal and proceed to the next largest until the right fit is achieved. The appropriate size is the largest size that allows the component to achieve the correct overall head height. (Too large a component will not allow the component to sit down, in the shaft and the component will be placed too high.)
Four-Part Proximal Humerus Fractures Treated with Hemiarthroplasty
Incidence and Mechanism of Injury
Treatment
Indications for Surgery
Surgical Technique
Positioning
Surgical Approach
Tuberosity Isolation
Tuberosity Mobilization
Humeral Head Sizing
Humeral Component Positioning
Shaft Preparation
Humeral Component Size
Four-Part Proximal Humerus Fractures Treated with Hemiarthroplasty
Only gold members can continue reading. Log In or Register to continue

Full access? Get Clinical Tree








