INTRODUCTION
Foot pain and problems are common among people of all ages. The prevalence has been reported as 15% to 40%, depending on the demographic distribution of the patient population (
1,
2,
3). Foot disorders in the younger age group are frequently the result of trauma or congenital anomalies, and require a different approach to management than the elderly adult. The published literature on foot pain in the adult/aged population is quite extensive and indicates that it affects between 20% and 30% of community-dwelling elders (
4). Some studies have shown that foot pain is associated with decreased ability to perform activities of daily living (
5), problems with balance and gait (
6,
7,
8) and increased risk of falls. Others have not found that to be the case (
9).
In fact, they reported that while there are a significant number of foot problems facing the elderly, only plantar fasciitis and a pes cavus foot profile are associated with functional foot problems. Another study has shown that elders with rheumatoid arthritis and who have significant foot pain are more likely to report back, hip, hand, and wrist pain. They also have pes planus and loss of motion in the ankle joint (
10).
While it is useful to understand the issues of prevalence of foot pain and problems, and their associations with function, these must be understood within the context of the specific population (e.g., diagnostic group, age, etc.) of interest.
ANATOMY
Examination of the foot is challenging because of its complex anatomy, its biomechanical properties, and its function. This section attempts to describe important anatomic information that will enable the clinician to understand the affected anatomic site, but the reader is referred to books on anatomy, which present a more in-depth review (
11,
12,
13).
Each foot is composed of 26 bones and 55 joints with muscle attachments that have their origin either within the foot or from the anatomical structures above the ankle. It is easier, therefore, to divide the foot into sections: the forefoot, midfoot, and rearfoot-ankle complex. This simplifies the examination process and provides the foundation necessary to understand biomechanical principles. The forefoot consists of 5 metatarsals and 14 phalanges constituting the five digits. The midfoot includes three cuneiform, cuboid, and navicular. The rearfoot-ankle complex is composed of the talus, calcaneus, and distal ends of the tibia and fibula (
Fig. 38-1). These three divisions form a tenuous interrelationship that can easily be disrupted, resulting in dysfunction and pathology.
The hallux contains two phalanges, and the remaining four digits contain three each. The hallux has one joint: the interphalangeal joint. The lesser digits form the proximal and distal interphalangeal joints. There is a tendency for the intermediate and distal phalanges of the fifth toe to be fused together. The first metatarsal head distally articulates on the plantar surface with the tibial and fibula sesamoid bones, which are within the flexor hallucis brevis tendon. There are three cuneiforms that articulate with the base of metatarsals one through three. The cuboid articulates with the fourth and fifth metatarsal bases. The five metatarsals, along with the three cuneiforms and cuboid, form Lisfranc’s joint. Injury to this joint often is missed at initial presentation with significant associated morbidity. The keystone of this joint is the second metatarsal cuneiform articulation. The base of the fifth metatarsal, along with the lateral styloid process, serves as the insertion site of the peroneal brevis tendon. Injuries to the base of the fifth metatarsal and the styloid process are common, especially after inversion injuries of the ankle. The configuration of the articulation between the metatarsals, cuneiforms, and cuboid helps form the transverse metatarsal arch. Proximally, the cuneiforms articulate with the navicular, and laterally, the cuboid articulates with the navicular and lateral cuneiform. Medially, on the navicular, there is an enlarged tuberosity that serves as part of the insertion points of the tibialis posterior tendon. The navicular and cuboid proximally articulate with the talus and calcaneus, respectively, forming the midtarsal joint. The calcaneus is the largest bone of the foot. It functions as a major weight-bearing bone and serves as the insertion site posteriorly for the Achilles tendon. Many of the intrinsic muscles
arise from its plantar tubercles. The calcaneus is composed primarily of cancellous bone. Its dorsal surface articulates with the talus through three articulating surfaces—anterior, middle, and posterior—called facets. This forms the subtalar joint. A tunnel forms across the middle facet that begins laterally as the sinus tarsi and ends medially as the tarsal canal. Medially, the calcaneus forms a projection called the
sustentaculum tali that provides a groove for the flexor hallucis longus tendon. The talus acts as a torque converter that connects the leg to the foot. It is almost completely covered with cartilage and has no muscular or tendinous attachments. Anatomically, it is divided into the head, neck, and body. The body, through its superior trochlear surface, the talar dome, forms the ankle joint with the distal extensions of the fibula and tibia, termed
malleoli. The trochlear surface is wider anteriorly, which provides increased stability of the ankle in dorsiflexion. Plantar flexion of the ankle results in articulation, with the narrower portion of the posterior trochlear surface, resulting in intrinsic instability associated with the common ankle sprain. Fractures of the talus at its neck are associated with increased frequency of avascular necrosis owing to its tenuous but generous blood supply. Fractures of the talar body often result in posttraumatic arthritis. Posteriorly, the talus forms two tubercles—medial and lateral. The lateral tubercle has been called
Steida’s process. Sometimes, the lateral tubercle fails to ossify completely; it is then termed the
os trigonum.Blood supply to the foot is the result of branches from the popliteal artery. The popliteal artery divides into the anterior tibial, posterior tibial, and peroneal arteries. The branches of these arteries are noted in
Table 38-1. The venous drainage system of the foot is divided into deep and superficial segments. The lesser saphenous and greater saphenous veins form the superficial system, whereas the deep venous arch provides the deep drainage.
Motor and sensory nerves to the foot arise from branches of the sciatic nerve. The sciatic nerve divides into the tibial nerve, common peroneal nerve, and sural nerve. The common peroneal nerve divides into the superficial and deep peroneal nerves. They provide sensory input to the dorsal aspect of the foot and digits. The sural nerve innervates the lateral aspect of the foot. The saphenous nerve innervates the medial aspect of the foot and is a branch of the femoral nerve. The motor component of the peroneal nerve innervates the peroneus longus, peroneus brevis, extensor hallucis longus, extensor digitorum longus and brevis, tibialis anterior, and peroneus tertius. The tibial nerve divides into the medial and lateral plantar nerves. They provide sensory and motor innervation to the plantar aspect of the foot.
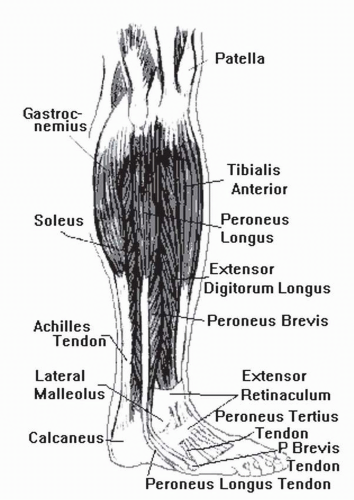
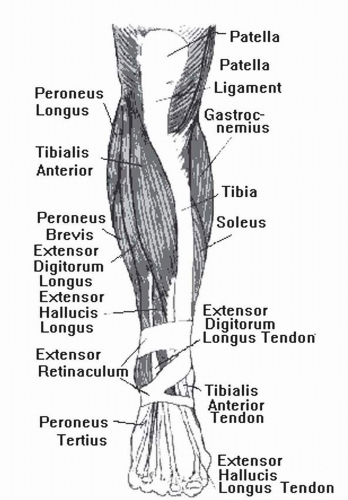
The muscles of the foot are divided into extrinsic and intrinsic groups (
Figs. 38-2 and
38-3). The extrinsic muscles arise in the leg and insert into the foot and are held in place by various retinacula as they enter the foot. They are divided into four compartments: superficial posterior, deep posterior, lateral, and anterior (
Table 38-2). The intrinsic muscles of the foot are divided into dorsal and plantar groups. The plantar muscles are divided into four layers, with the first layer being the most posterior or superficial and the fourth layer the most anterior or deep (
Table 38-3).
Functional Anatomy
The foot is divided into three functional units or parts: the hindfoot (talus and calcaneus and its attachments) provides the foot with stability; the midfoot (navicular, cuboid, cuneiforms, Lisfranc’s and Chopart’s joints) provides both sagittal and frontal plane motion; and the forefoot (metatarsals and phalanges) permits push-off. The ligamentous structures establish and preserve the longitudinal arch, the intermetatarsal transverse arch, the position of the sesamoids, and stability of the ankle mortise.
The subtalar joint is composed of the talus and calcaneus. The bones articulate at the posterior, middle, and anterior facets. The joint is responsible for triplane motion, primarily pronation and supination. There is 20 degrees of inversion to 10 degrees of eversion to the subtalar joint. In closed kinetic chain pronation, the calcaneus everts, with adduction
and plantar flexion of the talus. The opposite is true for closed kinetic supination (
Fig. 38-4).
The position of the subtalar joint dictates the position of the midtarsal joint. When the subtalar joint supinates, the arch raises the forefoot, and the foot becomes more rigid. The midtarsal joint “locks.” When there is subtalar joint pronation, the midtarsal “unlocks” and becomes less rigid. The foot becomes a mobile adaptor, allowing for increased motion to take place to accommodate for varying terrain.
The midtarsal joint is made up of the calcaneocuboid and talonavicular joints. The midtarsal joint has two axes of motion: the longitudinal and oblique axes. The longitudinal axis inverts and everts the forefoot while pronation or supination occurs. The oblique axis allows for adduction, abduction, plantar flexion, and dorsiflexion of the foot.
Physical Examination of the Foot
ROM assessment of the lower extremity is important because absence of normal range has functionally important sequelae. For example, a tight Achilles tendon, which limits ankle dorsiflexion, creates a force anterior to the axis of the ankle, which results in pronation, or collapse of the medial column. Limitation of hallux dorsiflexion to less than 25 degrees creates an impediment to forefoot push-off.
When testing ROM for the ankle, there should be at least 10 degrees of dorsiflexion with 45 degrees of plantar flexion. When testing the range of dorsiflexion, the examiner should hold the foot medially. This keeps the midtarsal joint locked, and a more accurate measurement can be achieved. Dorsiflexion is measured with the knee extended and flexed. When the knee is flexed, there is more dorsiflexion of the ankle because of the “unlocking” of the gastrocsoleus complex. The ankle motion should be smooth and unrestricted. The subtalar joint should measure 20 degrees of inversion and 10 degrees of eversion. This can be measured with the patient in the prone position. The heel is bisected in half, and the examiner can then use a tractograph and invert and evert the foot for the measurement. The metatarsophalangeal joints, the distal and proximal interphalangeal joints of the lesser toes, and the interphalangeal joint of the hallux should have smooth and unrestricted dorsiflexion and plantar flexion.
Muscle strength testing provides important information about whether the foot is likely to be supported in stance (static) and dynamic phases of gait.
Support of the foot in stance comes from the ligaments and plantar fascia, which stabilize the longitudinal arch and the intrinsic muscles of the foot. The creation and establishment of the longitudinal arch in the dynamic phase depend on the posterior tibialis and intrinsic and extrinsic muscles of the foot. The gastrocsoleus provides propulsion through sagittal plane motion at the ankle. Weakness in these structures may help explain an apropulsive gait or instability during stance.
Determination of static alignment of the foot provides important information about how the foot will contact the ground. The preferred position is that the foot should be parallel to the floor. If ligamentous structures are intact, ROM abnormality or muscle imbalance is likely to explain alignment problems. Examination demonstrates possible forefoot varus or valgus deformity. This is performed with the patient in the prone position with the subtalar joint neutral.
The feet should be evaluated in the standing position, and the arch height is evaluated as flat, low, normal, or high, based on the navicular position. The angle of the talus measured radiographically may be used to assess arch height. Bisecting the Achilles tendon will demonstrate whether the calcaneus is everted or inverted with respect to the midline. A varus rearfoot generally causes pressure to the posterosuperior lateral aspect of the calcaneus. A bone spur can develop in this area and cause pain. This is known as a Haglund’s deformity. Severe calcaneoeversion can cause a lateral impingement and pain to palpation below the lateral malleolus.
The vascular exam will evaluate peripheral pulses in the foot. Dorsally, there is a dorsalis pedis pulse, and medially a posterior tibial pulse. If one cannot feel a pulse and there is questionable vascular compromise, the physician can order further vascular testing such as noninvasive arterial Doppler. This exam would be beneficial when dealing with lower extremity ulcerations. Capillary filling time is tested and should be within 2 seconds. Press the distal tip of the digit and determine how fast the digit fills up with blood. Another area of testing would be for dependent rubor. Dangle the foot off the examining table and see if the foot becomes more red or purple. If this occurs, there may be pathology to the venous system of the lower extremity. Any varicosities should also be noted to the lower extremities, as well as chronic swelling. Patients with brawny edema from venous stasis disease may develop ulcerations to the medial lower leg or ankle.
The neurological exam will test deep tendon reflexes, ankle clonus, Babinski’s sign, sharp and dull discrimination, as well as vibratory sense and proprioception. Patients who are neuropathic have diminished sensation, vibratory sense,
and lack of proprioception. It is useful to test for protective sensation using Semmes-Weinstein filaments. Those who cannot feel the touch of a nylon filament 5 mm in diameter are at significant risk for ulceration. They are at risk for ulcerations because they lack sensation to the foot and do not feel the pressure caused by a foreign body, minor cut, abrasions from poorly fitted shoes, or thickened calluses.
Examination of the skin indicates where pressure points are. Callosities are in areas of high pressure and often need to be relieved.
BIOMECHANICS
Foot motion depends on intrinsic and extrinsic muscles that are divided into four compartments (see
Table 38-2). These muscles produce sagittal, frontal, and transverse plane motion.
To understand foot biomechanics, the physician must be proficient in the terms used to describe the motion and position of the foot. A list of terms commonly used follows:
Abduction: movement of the foot away from the midline of the body
Adduction: movement of the foot toward the midline of the body
Eversion: turning inward of the feet with the soles pointing away from each other
Inversion: turning inward of the feet with the soles pointing toward each other
Dorsiflexion: motion whereby the distal end of the foot moves toward the tibia
Plantar flexion: motion occurring to the foot whereby the distal end of the foot moves away from the tibia
Pronation: triplane motion of the foot in the direction of abduction, eversion, and dorsiflexion
Supination: triplane motion of the foot in the direction of adduction, inversion, and plantar flexion
Subtalar joint: point at which the normal foot is neither inverted nor everted
Neutral position: from the floor during stance; clinically, whereby the posterior aspect of the calcaneus lines up with the lower one third of the leg
Forefoot varus: inversion to the plantar surface of the forefoot with the subtalar joint neutral and the midtarsal joint pronated; this is a congenital bony deformity
Forefoot valgus: eversion to the plantar surface of the forefoot when the subtalar joint is neutral and the midtarsal joint is pronated; the plane of the metatarsals are everted with the first metatarsal lower than the fifth metatarsal; the first metatarsal may be flexible or rigid; this is a congenital bony deformity
Rearfoot varus: inverted position of the sagittal plane and the plantar surface of the calcaneus to the weight-bearing surface with the subtalar joint in the neutral position and the body standing in normal base of gait (10 degrees to 15 degrees of abduction)
Rearfoot valgus: the sagittal plane of the posterior and plantar surface of the calcaneus are everted to the weight-bearing surface when the subtalar joint is in neutral position while the body is standing in base of gait
Often, with increased subtalar joint pronation, the foot becomes hypermobile, and increased stress and strain are placed on the lower extremities. A functional valgus occurs at the knee, causing increased stress to the medial aspect of the knee. Hyperpronation causes increased strain on the plantar fascia, causing a pull on the origin of the fascia of the calcaneus. Patients are predisposed to bunions, hammertoes, and postural fatigue with increased subtalar joint pronation. Posterior tibial and Achilles tendinitis can occur with a hypermobile foot because of the increased stretching to the tendon.
A supinated foot or high-arched foot is much more rigid. This type of foot structure predisposes the patient to lateral ankle sprains, lateral Achilles tendinitis, claw toes (flexion deformity at the proximal and distal interphalangeal joints), increased incidence of avulsion fractures to the base of the fifth metatarsal, peroneal subluxation, metatarsalgia, and sesamoid pain or fractures.