Physical examination is pertinent for the presence of deformity and the amount of soft-tissue swelling.
Occasionally, injuries are open; these should clearly be noted and treated on priority.
Neurovascular status should likewise be noted, especially in the presence of dislocation that increases the likelihood of neurovascular compromise.
A standard radiographic series of the ankle, including an anteroposterior (AP), lateral, and mortise radiograph, is generally sufficient to classify these injuries and plan treatment.
Occasionally, if a patient has more proximal leg tenderness or medial clear space widening with no obvious fibular fracture, full-length radiographs of the tibia and fibula should be obtained to rule out the presence of a high fibular fracture as in the case of a Maisonneuve injury.
Initial treatment for all displaced ankle fractures is closed reduction and placement of a splint or cast.
If anatomic reduction of the joint is achieved the fracture can be treated closed, generally with 6 weeks in a short nonwalking cast followed by a variable period of protected weight bearing in a cast or removable boot.
Regular follow-up is necessary to rule out redisplacement of the fracture fragments during fracture healing
A special case exists with SER type II injuries in which there is no medial ankle injury. These are stable injuries and can be treated with weight bearing as tolerated throughout the course of treatment usually in a cast or boot, but some have advocated using just a stirrup brace for protection.
Persistent displacement after closed reduction of greater than 1 to 2 mm of the talus should be treated with operative reduction if there is no medical contraindication. Previous studies have demonstrated a significant increase in intra-articular contact stresses with minimal residual displacement of the talus. One study demonstrated that displacement of the fibula in a PER fracture model increases contact stresses most with shortening of the fibula, followed by lateral translation, and external rotation.
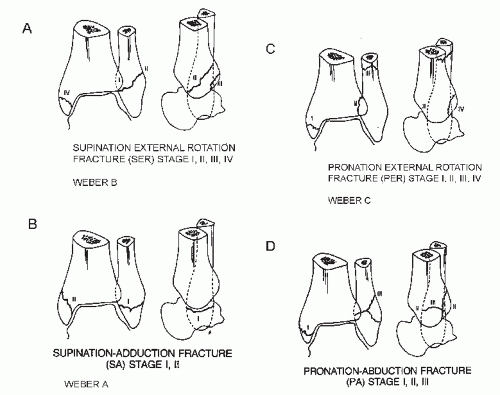
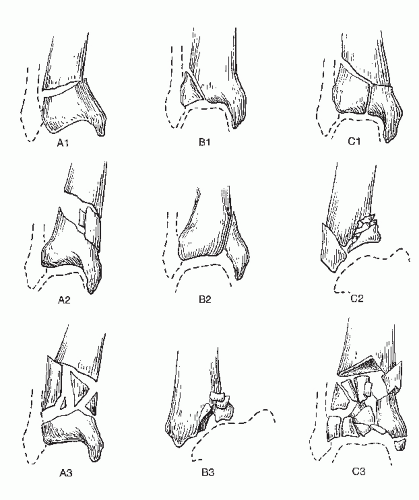
TABLE 14.1 THE DENNIS-WEBER CLASSIFICATION SYSTEM FOR ROTATIONAL ANKLE FRACTURES | ||||||||
|---|---|---|---|---|---|---|---|---|
|
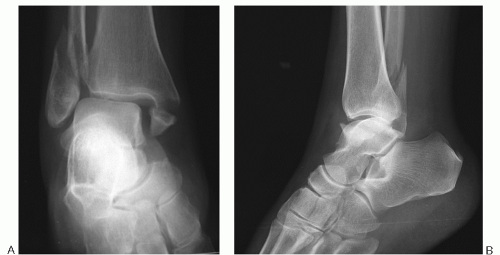
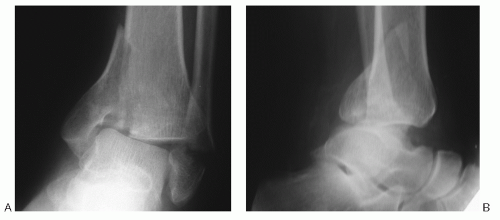 Figure 14.1 AP (A) and lateral (B) X-rays demonstrating Weber A fracture of the ankle. Note transverse fracture of fibula below the level of plafond and vertical fracture of the medial malleolus. |
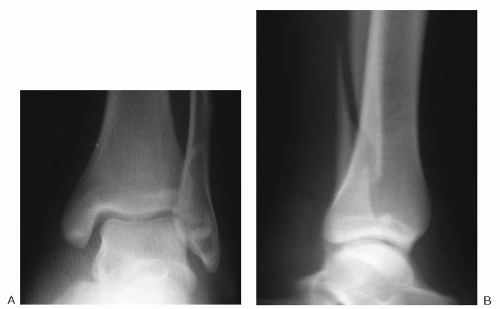 Figure 14.3 AP (A) and lateral (B) X-rays demonstrating Weber C ankle fracture. Note fibular fracture above the level of the plafond with intact medial malleolus in this case. |
injury have occurred (Fig. 14.6). Less stability is present in patients with deltoid ligament rupture rather than a medial malleolus fracture because internal fixation of the medial malleolar fragment does restore some degree of medial stability through the attached deltoid ligament. In cases of deltoid ligament rupture or higher fibular fracture, especially more than 4.5 cm above the joint, a greater degree of syndesmotic instability usually persists after fixation of the fibular fracture.
TABLE 14.2 LAUGE-HANSEN CLASSIFICATION SYSTEM FOR ROTATIONAL ANKLE FRACTURES | ||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
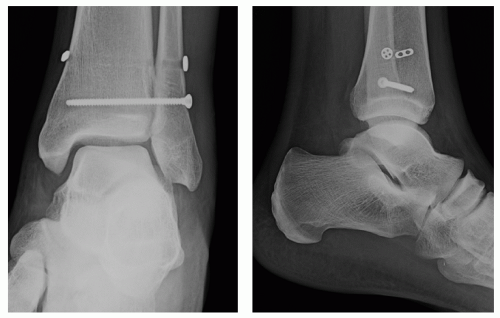
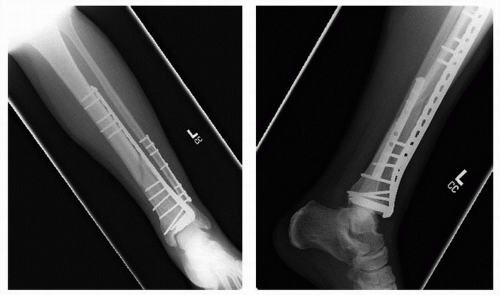
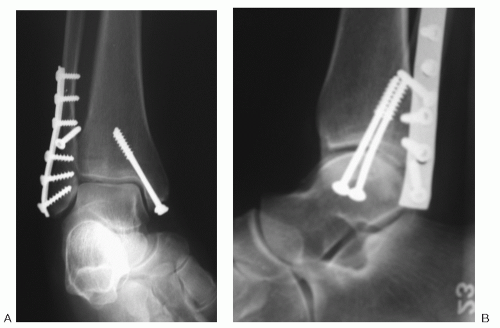 Figure 14.5 Postoperative AP (A) and lateral (B) X-rays demonstrating fixation of bimalleolar Weber B SER ankle fracture. |
require removal (Fig. 14.8). Controversy also exists over the necessity and timing for removal of syndesmotic screws; I prefer to leave syndesmotic screws in for 3 to 4 months following operative treatment of a fracture, but patients are allowed to begin weight bearing 6 weeks after operative fixation. Some surgeons routinely leave syndesmotic screws in place.
Most patients who have sustained a tibial pilon fracture present with a history of high-energy trauma to the lower extremity.
There is a relatively high incidence of associated musculoskeletal and other system trauma owing to the high-energy nature of this injury.
Occasionally, patients report a severe rotational injury, such as may occur while skiing, that can lead to a split rather than an axial load of the plafond with a better prognosis.
In addition to delineating the mechanism of injury, the history should evaluate associated medical conditions that may increase the risk of wound-healing problems, such as diabetes or peripheral vascular disease.
The use of tobacco, which leads to increased wound-healing problems and poorer bone healing, should also be evaluated.
Open injuries should be documented and urgently managed with surgical irrigation and debridement.
Otherwise, the magnitude of soft-tissue swelling and the presence of fracture blisters should be noted. Fracture blisters are of two types:
Clear fluid-filled blisters—cleavage injury at the dermal-epidermal junction with areas of retained epithelial cells leading to faster reepithelialization
Blood-filled blisters—more significant injury without areas of retained epithelial cells with higher rate of wound complications when surgery is performed through these areas
In general, blisters should be allowed to reepithelialize before an incision is made through these areas.
Standard AP and lateral radiographs of the ankle are mandatory in all of these patients to assess the degree of damage to the joint surface, fibula, and adjacent metaphyseal-diaphyseal bone.
Occasionally, oblique radiographs can be helpful to further delineate the fracture anatomy.
CT scanning is helpful for preoperative and intraoperative planning and treatment and to provide a more accurate prognosis regarding eventual surgical outcome by determining the degree of comminution of the articular surface.
type I Rüedi-Allgöwer fracture with no displacement, it can be treated with a short leg nonwalking cast for approximately 6 weeks before being advanced to weight-bearing protection.
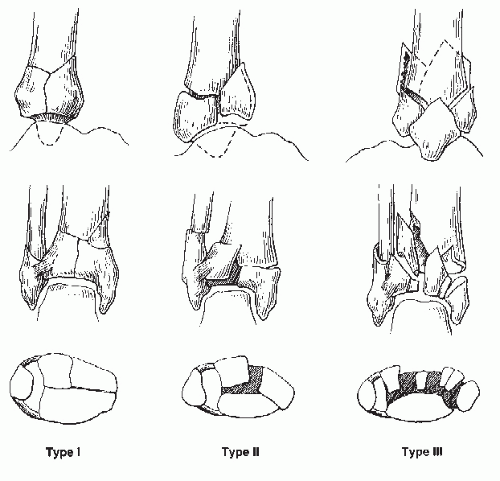
TABLE 14.3 RÜEDI-ALLGÖWER CLASSIFICATION OF TIBIAL PILON FRACTURES | ||||||||
|---|---|---|---|---|---|---|---|---|
|
TABLE 14.4 AO-OTA CLASSIFICATION OF TIBIAL PILON FRACTURES | ||||||||
|---|---|---|---|---|---|---|---|---|
|
Surgical incisions that allow adequate access to address the various fracture patterns are planned. An anterolateral approach has become the most common one used by many surgeons in the recent times (Fig. 14.11).
When more than one incision is used, as larger a skin bridge as is feasible is made to minimize the risk of skin necrosis.
Use of specialized low-profile, locking plates specifically designed for the tibial diaphysis, either anterolaterally or medially, have led to more stability, less soft-tissue tension, lower incidence of symptomatic hardware, and, combined with the aforementioned techniques, a lower wound complication rate (Fig. 14.12).
The joint surfaces are reconstructed from deep to superficial. As the reduction progresses, the deeper articular structures are no longer visible after the more superficial structures are reduced.
Preoperative CT scans help to localize the incisions directly over a fracture plane to minimize soft-tissue stripping necessary to mobilize the fragment (Fig. 14.13).
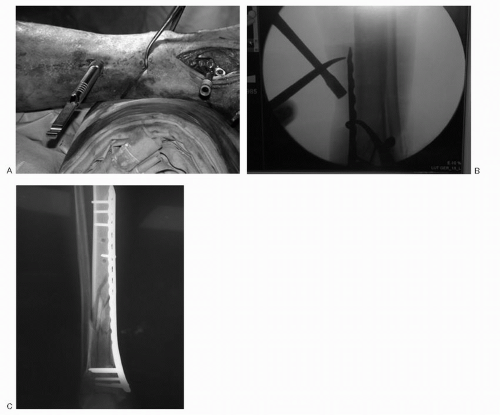
With a significant diaphyseal extension, subcutaneous plating methods wherein a small incision is made distally and a plate is slid along the subcutaneous border of the tibia with percutaneous screws placed into the plate proximally helps to minimize soft-tissue trauma (Fig. 14.14).
This technique is facilitated by having a high-quality fluoroscopy unit with laser-targeting of the proximal holes to help localize the stab incision sites for proximal screws.
 Figure 14.11 Photograph demonstrating anterolateral exposure with anterior locking plate. The superficial peroneal nerve can be seen coursing obliquely across the surgical wound proximally. |
Potentially catastrophic wound complications with subsequent infection and osteomyelitis can develop after treatment of pilon fractures when operating through the compromised soft-tissue envelope.
The most important concept with regard to wound complications is to avoid them by delaying surgery with a temporary external fixator until the soft-tissue envelope is healthier (blisters are healed and soft-tissue edema is improved), performing a tension-free closure at the time of surgery, and using meticulous soft-tissue technique during the procedure.
Superficial skin necrosis is treated with local wound care.
Full-thickness skin loss with exposure of underlying bone and hardware mandates aggressive treatment, most likely with free flap coverage.
Osteomyelitis generally develops only in patients with significant wound complications.
The best treatment is avoidance by prompt treatment of deep wound dehiscences with exposed bone and hardware.
Chronic osteomyelitis must be managed with aggressive debridement and bone grafting, which usually necessitates an ankle fusion in cases that are salvageable.
Below-knee amputation is often the best salvage option in patients with chronic osteomyelitis.
Stiffness after tibial pilon fracture is because of a varying amount of posttraumatic fibrosis and arthrosis.
Although anatomic reduction and stable fixation allows for early range of motion (ROM) to help minimize stiffness, this is still a relatively common complication. It is a particularly difficult problem to treat, short of fusing the ankle joint.
Nonunion of the metaphyseal-diaphyseal junction is not uncommon in patients with these complex, high-energy injuries.
If healing is not evident by 12 weeks, bone grafting of the fracture site should be considered (Fig. 14.15).
Malunions are relatively common and are best avoided by creating a stable fracture construct at the time of initial treatment.
Many studies have documented nearly all cases to have some degree of radiographic evidence of varying degrees of posttraumatic arthritis after pilon fractures. Some have shown a correlation between fracture type, incidence of posttraumatic arthritis, and poor results.
The quality of the fracture reduction in some studies has correlated with clinical results.
Generally, they are associated with high-energy trauma such as motor vehicle accidents or fall from a height. The theoretical mechanism is hyperdorsiflexion of the neck of the talus with impaction of the neck or body against the anterior lip of the tibia, although it is difficult to recreate this fracture in the laboratory with this mechanism.
Artery of the tarsal canal—a branch of the posterior tibial artery, supplies medial half to two-thirds of the body
Artery of the sinus tarsi—formed from a branch of the anterior tibial and peroneal arteries, forming an anastomotic sling with the artery of the tarsal canal under the talar neck
Deltoid arterial branches—branch of the arterial tarsal canal that enters medially with the deep deltoid ligament and may be the only remaining blood supply in displaced fractures of the neck or body of the talus
 Figure 14.15 Postoperative X-ray 4 months after surgery demonstrating nonunion of metaphyseal-diaphyseal portion of a plafond fracture. |
Patients report a high-energy trauma.
Many patients have associated musculoskeletal trauma resulting from the high-energy nature of this injury with medial malleolar fractures reported in 20% to 50% of these patients.
On examination, fracture displacement and possible dislocation of the talus can be masked by rapid onset of swelling.
The body of the talus can be palpable subcutaneously in the posteromedial ankle in severe cases.
Neurovascular structures are usually spared from serious injury.
There is a relatively high incidence of open injuries in these patients.
The fracture is usually readily apparent from AP and lateral radiographs of the talus.
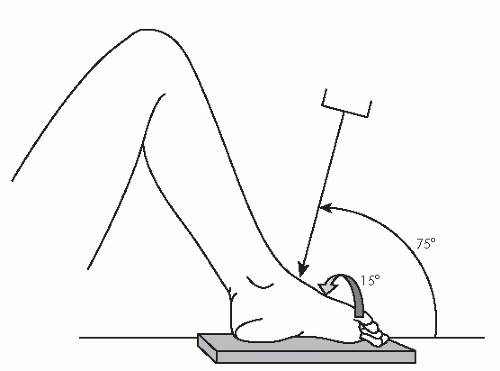
Varus or valgus displacement of the talar neck is best seen on a modified Canale view (Fig. 14.16).
In the Hawkins I fracture, the ankle can be placed in neutral position with no evidence of displacement.
On these rare occasions, patients can be kept in a cast for approximately 8 weeks followed by an additional month of protection with a controlled active motion walker. An apparent nondisplaced fracture that displaces with the ankle placed in neutral position is actually a Hawkins II fracture.
A Hawkins II fracture (Fig. 14.18) should be promptly treated with closed reduction.
Maximum plantarflexion and traction of the foot will usually realign the head with body fragment.
Varus or valgus stress realigns the neck in the transverse plane.
A near-anatomic reduction allows a delay in surgical treatment.
Hawkins III fractures with a dislocated body of the talus should be taken directly to surgery because the likelihood of successful closed reduction is negligible (Fig. 14.19).
Operative treatment of these fractures should use a combined anteromedial—anterolateral approach.
Anteromedial incision—anterior aspect of the medial malleolus, dorsal aspect of the navicular tuberosity, which exposes the medial neck.
Anterolateral incision—from anterior tip of the fibula to base of the fourth metatarsal, exposing the lateral neck of the talus and allowing access to the subtalar joint.
Fixation is generally with 3.5-mm fully threaded cortical screws for neutralization in contrast to lag fixation to prevent displacement into varus if medial comminution is present (Fig. 14.20).
Titanium screws allow for postoperative MRI (Fig. 14.21).
Although screws inserted from posterior lead to greater biomechanical stability, they necessitate a third incision (which is difficult with the patient in the supine position) as the two anterior incisions are necessary for reduction; in my opinion, this is not necessary.
Hawkins III fractures require a longer medial incision and generally require medial malleolar osteotomy to facilitate reduction if the malleolus has not been fractured.
A traction pin should be placed in the inferior aspect of the calcaneus to facilitate reduction of the body of the talus into the mortise.
With talar body fractures, medial malleolar osteotomies are often necessary to facilitate exposure and reduction of the body of the talus, because the malleoli preclude adequate visualization of the fracture (Fig. 14.22).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree