Chapter
7
Foot and Ankle Malunions
Foot and ankle malunions are unique!
Three major differences are seen in foot and ankle malunion in comparison to malunion elsewhere.
1.Secondary arthritis of adjoining joints is quick and inevitable:
Structurally, foot and ankle have multiple small bones having many articulations with each other. Movements are coupled and interlocked. Malposition of one bone thereby would affect many joints located proximally, distally, and sideward, leading to fast and inevitable arthritis of these joints (Figs. 7.1 and 7.2).

Fig. 7.1 X-ray picture showing malunion of cuboid while navicular fracture was only treated.

Fig. 7.2 Malunion of navicular leading to arthritis of adjoining joints.
2.Pressure effects over surrounding muscles, tendons, fascia, and nerves:
Malunion of calcaneus may give pressure effect on plantar fascia, peronei, calcaneofibular ligament, tendon of tendo-Achilles and flexor hallucis longus, sural and posterior tibial nerves. Lisfranc and midfoot bone malunions can give pressure over dorsal cutaneous nerves and tendon of tibialis anterior and long extensors (Figs. 7.3 and 7.4). Forefoot malunion will give pressure effect on plantar skin, leading to formation of corns and callosities (Fig. 7.5).
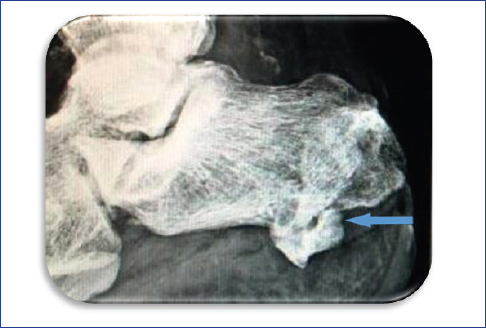
Fig. 7.3 Malunited calcaneal fracture giving plantar pressure and pain.
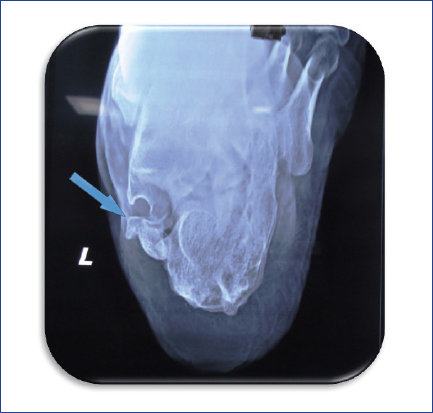
Fig. 7.4 Malunited calcaneus giving pressure medially on flexor hallucis longus tendon and posterior tibial nerve, leading to tendinitis of flexor hallucis longus tendon and secondary tarsal tunnel syndrome.
3.Difficulty in gait and footwear utilization:
Increased foot size following malunion poses difficulty in wearing standard footwear. Gait would be altered due to secondary deformities and pain due to the same (Fig. 7.6).

Fig. 7.6 Calcaneus malunion on right side giving rise to broadening and shortening of heel making it difficult for the standard shoe to fit.
Assessment of Delayed Presentation and Malunion
Malunion could be assessed by taking into account the following points:
♦ Chief complaints and duration of the same
♦ Treatment taken
♦ Shape of foot
♦ Examination of arches
♦ Neurological examination
♦ Assessment of individual muscles
♦ Assessment of movements of all joints
♦ Gait examination
♦ Footwear evaluation
♦ Foot and ankle series X-rays
♦ Standing radiography
♦ Comparative radiographic evaluation
♦ CT scan and MRI, if needed
Differential injectioning technique to diagnose various pain generators forms the most important part of examination.
Management
Management of malunions varies from that of the original fractures. The points of difference are enumerated in Box 7.1.
Box 7.1 How does management differ?
♦ Revision fixation works well even for malunion of longer duration.
♦ Oftentimes, fusion has to be preceded by fixation to avoid pressure effects as well as to restore biomechanics. Combinations of both work well.
♦ Excision of exostosis or bony bumps forms the mainstay of treatment to decompress pressure effects over tendons, muscles, and nerves.
♦ Replacement arthroplasty has yet to establish its place.
♦ External fixation is required more often than elsewhere because of poor soft tissue envelope.
♦ Fusion overplays replacement in comorbid conditions.
♦ Excision arthroplasty is most commonly used for malunion affecting metatarsophalangeal, proximal interphalangeal, distal interphalangeal, and fourth and fifth tarsometatarsal joints.
Tips and Tricks
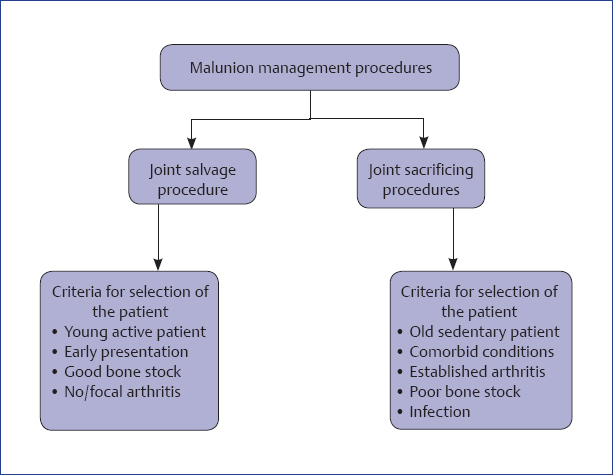
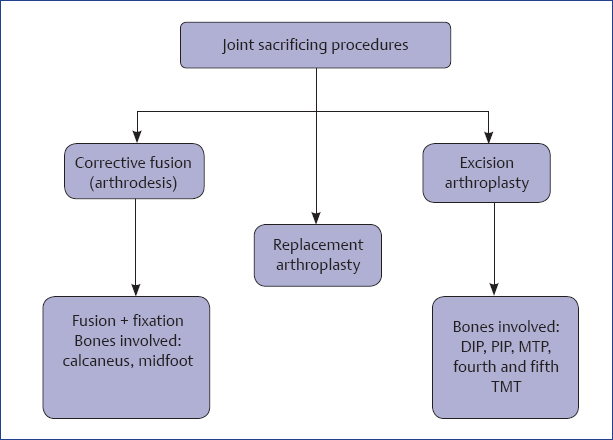
♦ Two basic sets of procedures are adopted: joint salvage and joint sacrificing (Flowcharts 7.1–7.3).
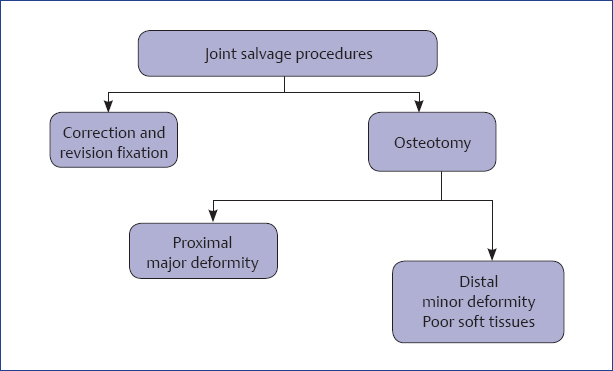
Flowchart 7.2 Treatment plan of joint salvage procedures.
♦ For young active patients with good bone stock, joint salvage procedures are reserved.
♦ For old sedentary patients with comorbid conditions and poor bone stock, joint sacrificing procedures are undertaken.
♦ Joint salvage procedures are correction with revision fixation provided arthritis has not set in.
♦ With focal or no arthritis in the presence of a deformity, osteotomy to correct the deformity is done. For a smaller deformity, distal corrective osteotomy would work, while proximal corrective osteotomy is preferred for better correction of axis in a case with major deformity.
♦ Arthrodesis, excision arthroplasty, and replacement arthroplasty are options for joint sacrificing procedures.
♦ Arthrodesis with fixation is carried out in calcaneal and midfoot malunions.
♦ Arthrodesis is the most preferred method, except for fourth and fifth tarsometatarsal joints, distal and proximal interphalangeal joints, and lesser metatarsophalangeal joints where excision arthroplasty is preferred.
♦ Arthroplasty is in consideration for ankle joint in patients with minimal deformity and good bone stock with good vascularity without the presence of any neuropathy or infection.
Decision Making
Decision making depends on various factors as shown in Fig. 7.7.
♦ Duration of malunion: Longer the duration, the more difficult is to do revision fixation through the original fracture site. Also, there are more chances of setting of arthritis in the adjoining joints making revision fixation more difficult.
♦ Age and activity level of patient: Arthrodesis may be reserved for old sedentary patients with comorbid conditions as a single-stage gold standard procedure. Heavy laborers may as well be treated with arthrodesis. Corrective revision fixation would be a procedure of choice in most others.
♦ Presence of arthritis: Arthritis warrants fusion over fixation. Cases with focal arthritis may be treated with corrective osteotomy in major joints like ankle.
♦ Presence of deformity: Deformity must be minimal for replacement surgery to be carried out and it must be corrected before final surgery. At arthrodesis also in situ fusion is avoided. Corrective osteotomy must precede removal of articular cartilage.
♦ Presence of infection: Infected cases are best fused than revised. Cases with active infection would favor use of external fixation devices for fusion.
♦ Vascular status of the limb: Evaluation of the vascular status of the limb plays most important role in decision making. With poor vascularity, healing is doubtful. Amputation may be a choice in such vascularity-deficient limbs.
♦ Neurological status of the limb: Neuropathy would dictate longer, stronger, and combination of implants for arthrodesis where adjoining joints are also spanned to get better stability. Failure rates are high.
♦ Condition of skin at operative site: Skin condition or scarring would force a surgeon to modify surgical approach and use of implants.
Management of Specific Malunions
Various specific malunions are listed in Box 7.2. Tips and tricks for the management of these specific malunions are explained as follows.
Box 7.2 Specific malunions
♦ Pilon malunion
♦ Ankle malunion
♦ Calcaneal malunion
♦ Talar malunion
♦ Midfoot malunion
♦ Forefoot malunion
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree