CHAPTER 74 Fixed Sagittal Imbalance
Fixed sagittal imbalance is a condition that occurs as a result of the loss of the normal lumbar lordosis or an increase in thoracic kyphosis, or both, resulting in the forward displacement of the head relative to the sacrum and pelvis. This “pitched forward” posture can lead to a number of debilitating consequences including difficulties with forward gaze, compensatory hip and knee flexion contractures, and loss of physiologic endurance as a result of increased energy expenditure.1 A number of etiologies of fixed sagittal imbalance are discussed in this chapter. The treatment of symptomatic sagittal imbalance is potentially complex, requiring correction, often with one or more osteotomies, and spinal instrumentation and arthrodesis.
Sagittal Alignment
An understanding of normal sagittal parameters is helpful in assessing patients with sagittal imbalance. Numerous authors have reported on ranges of sagittal alignment in asymptomatic volunteers. Bernhart and Bridwell2 studied 102 asymptomatic adolescent volunteers and described wide ranges of thoracic kyphosis (9 to 53 degrees, SD ± 10 degrees) and lumbar lordosis (−14 to −69 degrees, SD ± 12 degrees). The average age of patients in this study was 12.8 years. Stagnara and colleagues3 reported similar measurements in a group of 100 French volunteers aged 20 to 29 years. One hundred asymptomatic subjects and 100 patients with mechanical low back pain of slightly older age (mean age 39 years) were compared by Jackson and McManus.4 The differences were statistically significant as a result of the large study size; the absolute numbers were similar. The total lordosis averaged 60.9 degrees in the asymptomatic group versus 56.3 degrees in the symptomatic group. The authors reported that patients who were symptomatic were able to compensate for distal lumbar hypolordosis with exaggerated lordosis in the proximal lumbar spine. In general, all studies noted that approximately two thirds of the total lumbar lordosis is attained distally between L4 and the sacrum.
Standing sagittal alignment is typically measured from the middle of the C7 vertebral body on a 36-inch-long cassette radiograph. The spine is considered to be in neutral sagittal alignment when a gravity plumb line extending from the center of the C7 vertebral body bisects the S1 endplate. When the C7 plumb line passes anteriorly to the sacrum, the sagittal balance is considered positive; sagittal balance is negative when the C7 plumb line falls posteriorly to the sacrum.5 Recent studies have demonstrated that the C7 plumb line migrates more anteriorly with advancing age.6 This is due in large part to the loss of lumbar lordosis that occurs with disc degeneration.7 Pelvic parameters such as pelvic tilt and pelvic incidence and the relationship between the gravity line and heel position are additional methods to further the understanding of sagittal alignment and relationships with age.8,9
Etiology
Sagittal imbalance can have a variety of causes. One of the most common causes is the prior placement of Harrington distraction instrumentation for the treatment of scoliosis.10–12 A typical example would be a patient with a double major curve type pattern treated in the 1970s or 1980s with Harrington instrumentation extending from T4 to L3 or L4. If the spine was fused in proximal lumbar hypolordosis, maintenance of normal overall lumbar lordosis was often achieved with increased lordosis of the remaining normal discs—L3-4, L4-5, and L5-S1. If, over time, these discs degenerate, the patient will develop the progressive inability to compensate for the prior hypolordotic fusion and will develop sagittal imbalance. Moe and Denis13 have demonstrated the loss of lumbar lordosis after these procedures that results in the forward tilting of the spine. Patients who underwent these procedures 20 to 40 years ago are now becoming symptomatic.14
A second common scenario is termed degenerative sagittal imbalance.15 In this case, an adult patient has had numerous lumbar spinal fusion procedures, each with subsequent loss of lower lumbar lordosis. The incremental segmental changes gradually result in the patient’s inability to stand erect.
Another scenario involves the post-traumatic patient. An injury, typically a fracture at or around the thoracolumbar junction that heals in kyphosis, may present with a sharp, angular deformity.16 These deformities may be the sequelae of either operatively or nonoperatively treated unstable injuries. The patient typically complains of pain around the kyphos, as well as cephalad or caudad to the apex of the deformity. Compensation for the angular kyphotic deformity occurs at the suprajacent and subjacent disc spaces. With time, the discs can degenerate and lead to worsening of the deformity and increasing pain.
A fourth condition is the patient with ankylosing spondylitis. These patients will present with a lumbar hypolordosis and thoracolumbar kyphosis or cervicothoracic kyphosis.17 Patients with ankylosing spondylitis often have a stiff deformity and, as a result, are unable to compensate for it, leading to difficulties with forward gaze and mobility. Osteotomies in the lumbar spine or at the cervicothoracic junction are often necessary to correct the deformity.18,19
Patient Evaluation
History
Another essential aspect of the patient evaluation includes medical comorbidities, specifically diabetes, cardiac disease, and osteoporosis. Dual-energy x-ray absorptiometry (DEXA) is helpful in identifying patients with osteopenia and osteoporosis. These patients may benefit from preoperative pharmacologic treatment to improve bone mineral density. Patients who smoke are at significant risk of developing pseudarthrosis if spinal fusion is considered and may reasonably be required to cease smoking before surgery.20 All of these elements contribute to a thorough evaluation of the history of a patient with sagittal imbalance.
Physical Examination
The second aspect of the patient evaluation is the physical examination. Particular attention is paid to standing balance and gait. The overall postural balance in the coronal and sagittal planes and the pattern of gait should be examined. A patient with sagittal imbalance may often appear to have normal balance, only for the examiner to find that he or she is compensating with knee flexion. The apparent hip flexion is also often seen—in fact, femoral angulation relative to the vertical axis due to continued pelvic retroversion despite maximal hip extension. Lagrone and colleagues21 reported that almost 95% of patients with sagittal imbalance are unable to stand erect; nearly 90% had back pain with prolonged activity, and 27% had to flex their knees to stand erect. It is important to examine patients standing normally and with legs as straight as possible at the knee. The abdomen and back should be examined specifically for prior surgical incisions and postural creases and for a rotational deformity indicating a coronal spinal deformity. Examination of the patient in the supine and prone positions also helps to determine the flexibility of any spinal deformity, as evidenced by whether or not the kyphosis corrects with recumbent positioning. The supine position also eliminates the contributions of hip and knee flexion contractures to sagittal imbalance. Finally, a thorough neurologic examination is critical in all patients, but especially those who report deficits after prior surgery or whom upon history have suggestion of possible spinal cord level stenosis.
Radiographic Evaluation
Once the history and physical are complete, an assessment of the radiographic imaging is the next step in evaluation. Standing long cassette radiographs (14″ × 36″) are taken to include the entire spine from the base of the occiput to the distal sacrum and the femoral heads. The global spinal sagittal balance is determined using the C7 plumb line dropped vertically from the center of the body of C7. This may also be referred to as the sagittal vertical axis (SVA). The Scoliosis Research Society defines positive sagittal balance as the SVA passing anterior to the L5-S1 disc on the standing long cassette film. In general, any deviation of the SVA greater than 5 cm anterior to the normal position of the C7 plumb line is considered positive sagittal imbalance.14 Significant positive sagittal imbalance is defined as the C7 sagittal plumb line falling anterior to the femoral heads.
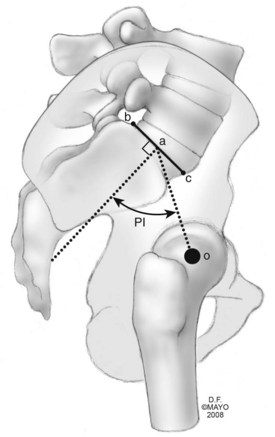
Other parameters that assist in the radiographic evaluation of these patients include measurements of the regional thoracic kyphosis (Cobb angle measured from T5-T12 on the lateral radiograph), lumbar lordosis (sagittal Cobb angle measured from the inferior endplate of T12 to the superior endplate of S1), thoracolumbar alignment (sagittal Cobb angle from T10-L2), and the pelvic incidence. The pelvic incidence assesses the relationship of the distal lumbar spine and sacrum to the pelvis and hip joints. The measurement is defined by the angle between the perpendicular to the sacral endplate and its midpoint and the line connecting this L point to the midpoint of a line connecting the femoral heads (Fig. 74–1).22,23
In addition to the long cassette standing radiographs, the authors routinely obtain focused studies of the lumbar and/or thoracic region. This helps in better defining local anatomy in a “coned-down” manner. Other useful studies include recumbent long cassette radiographs, either supine or prone. These radiographs help to elucidate the degree of flexibility within a deformity. The prone lateral view is similar to, but not exactly like, what the patient’s spine may look like on the operating table. Another useful radiograph is the supine hyperextension lateral, in which a bolster is placed under the apex of a kyphosis and, after some relaxation, a radiograph is taken to determine flexibility.24
Surgical Decision Making
For those patients with debilitating symptoms due to significant sagittal imbalance, surgical management generally involves spinal instrumentation and fusion in combination with an osteotomy or osteotomies to allow the surgeon to restore a more normal spinal alignment. The types of osteotomies include the Smith-Petersen osteotomy (SPO), the pedicle subtraction osteotomy (PSO), and the vertebral column resection (VCR).25,26 The key criterion for determining the necessity of an osteotomy is a partially or completely fixed deformity based on the physical examination and radiographic evaluation.27 Spinal malalignment that corrects entirely with prone positioning (seen on the recumbent lateral radiograph) is flexible; in this case, osteotomies for spinal realignment are unnecessary.
Sagittal imbalance may be divided into two types, I and II.25 Type I refers to a patient with a segmental problem, usually hyperkyphosis or limited lordosis. The segments above and below the problem can compensate for the local deformity, though, thus maintaining normal global sagittal spinal alignment. One example of a type I sagittal deformity is a patient with a post-traumatic kyphosis at the thoracolumbar junction with hyperlordosis of lumbar spine. Another example is a patient with Scheuermann kyphosis. Although the magnitude of the thoracic or thoracolumbar kyphosis can vary, and may be more than 100 degrees, the C7 plumb line remains normal.
Smith-Petersen Osteotomy
The original description of the SPO was given by Smith-Petersen and colleagues28 in 1945. It was described as a posterior wedge resection of the spine through the region of the facet joints in patients with ankylosing spondylitis with a subsequent controlled fracture of the ossified anterior longitudinal ligament. The ideal candidate for an SPO has a long, rounded kyphosis over multiple segments (e.g., a patient with Scheuermann kyphosis). The resection typically achieves about 10 degrees of correction per level, roughly correlating to one degree of lordosis for each millimeter of bone resection.29 The osteotomy requires removal of the interspinous ligaments, the ligamentum flavum, and the superior and inferior articular processes bilaterally. One of the requirements for an SPO is a mobile disc anteriorly because this osteotomy involves resection of posterior elements only, followed by compression posteriorly (Fig. 74–2). Compression of the remaining posterior elements can be achieved through gravity from appropriate intraoperative positioning, hinging of the operating table, or gentle compression against pedicle screw fixation, although the latter is not advisable in osteoporotic patients.30
< div class='tao-gold-member'>
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


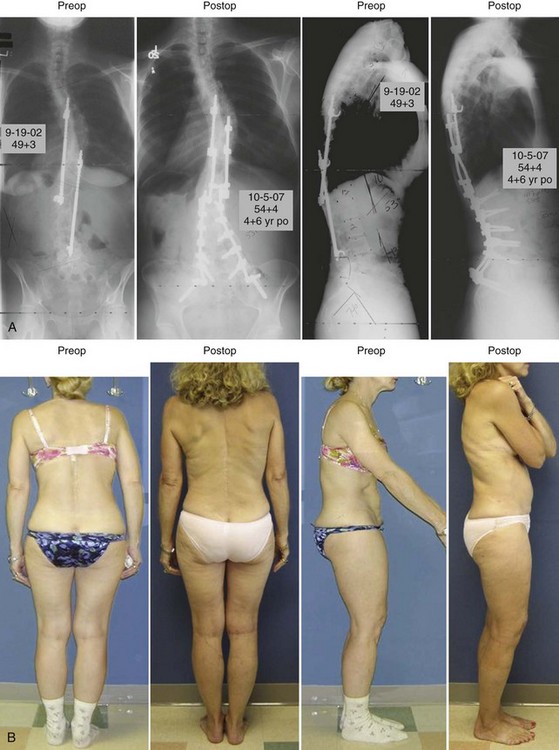
 -year postoperative coronal and sagittal radiographs of a 49-year-old female patient who presented having had Harrington fusion from T4 to L4 as an adolescent. She has now developed severe disc degeneration and spinal stenosis at L4-L5 and L5-S1. She has a mild to moderate sagittal imbalance. She was treated with decompression at L4-L5 and L5-S1 and extension of fusion to the sacrum. To restore sagittal balance, she also had two Smith-Petersen osteotomies (SPOs) performed through the prior fusion mass at L2-L3 and L3-L4 with local bone graft and biologics. B, Standing preoperative and
-year postoperative coronal and sagittal radiographs of a 49-year-old female patient who presented having had Harrington fusion from T4 to L4 as an adolescent. She has now developed severe disc degeneration and spinal stenosis at L4-L5 and L5-S1. She has a mild to moderate sagittal imbalance. She was treated with decompression at L4-L5 and L5-S1 and extension of fusion to the sacrum. To restore sagittal balance, she also had two Smith-Petersen osteotomies (SPOs) performed through the prior fusion mass at L2-L3 and L3-L4 with local bone graft and biologics. B, Standing preoperative and  -year postoperative coronal and sagittal clinical photos of the patient.
-year postoperative coronal and sagittal clinical photos of the patient.





