Femoroacetabular Impingement: Overview
Jeffrey J. Nepple
John C. Clohisy
“Impingement of the femoral neck on the anterior acetabulum … such impingement would result in ‘traumatic arthritis’ with characteristic changes of the joint surfaces.”
“Sufficient time has not elapsed to obtain true end results, but the author feels justified … because the method is non-destructive and seems effective in relieving pain in conditions for which there is no other adequate treatment.”
Marius Nygaard Smith-Petersen, MD, 1936
Introduction
Ganz et al. (1) refined the concept of femoroacetabular impingement (FAI) in the late 1990s. Their understanding of FAI was founded in their experience with the development of the Bernese periacetabular osteotomy (PAO) and the surgical technique for safe surgical dislocation of the hip. After PAO, excessive acetabular overcorrection was thought to result in FAI due to the creation of acetabular deformity (2). Through their experience with surgical dislocation and direct visualization of hip pathomechanics, they refined the concept of how subtle morphologic abnormalities of the proximal femur and acetabulum could result in FAI in the native hip. Yet, the recognition that subtle abnormalities in hip anatomy are linked to osteoarthritis was not new. In fact, the treatment of these deformities dated back to the 1930s. The refined understanding of the underlying mechanism of FAI revived concepts from decades earlier that were for the most part forgotten. The recognition of FAI and its fundamental role in the pathogenesis of hip osteoarthritis (3,4,5) led to a tremendous surge of research on the topic and treatment advances that continue today.
The Femoroacetabular Concept
FAI results from repetitive abutment of the proximal femur and acetabular rim at terminal hip range of motion that leads to progressive joint damage. FAI may result from primary deformity of the proximal femur (cam type), acetabulum (pincer type), or both (combined cam and pincer type). In cam-type FAI (Fig. 19.1), the proximal femoral pathoanatomy leads to a cam effect where the eccentric femoral head is forced into the smaller acetabular opening during terminal hip flexion and combined flexion/internal rotation. Repetitive abutment results in an outside-in abrasion to the labrochondral junction, most commonly in the anterosuperior quadrant. Labrochondral damage leads to detachment of the labrum from its cartilaginous attachment, and with more advanced disease may lead to articular cartilage flap formation (Fig. 19.2). In early stages, the labrum is generally detached from the adjacent cartilage but otherwise “uninvolved” (1,6). Pincer-type FAI results in a less focal region of impingement caused by the relative prominence of the acetabular rim. During terminal hip motion, an area of linear contact between the acetabulum and the proximal femur occurs. With repetitive impact, the labrum is repetitively damaged. This can result in significant degeneration of the labrum that may be accompanied by bone apposition of the acetabular rim. This has traditionally been described as labral ossification, but recent histologic studies by Ganz et al. demonstrated findings consistent with bony apposition (7). Appositional bone growth at the acetabular rim leads to earlier bony contact with the hip and subsequently worsens the impingement. This bony apposition further displaces the acetabular labrum causing even earlier impingement. In advanced cases of pincer-type FAI, the entire labrum may be absent and replaced by bony appositional tissue. Articular cartilage damage in pincer-type FAI is generally limited to the peripheral rim, with less destructive articular cartilage disease than that generally seen with cam-type FAI. Additionally, anterior bony impingement in pincer-type FAI can cause a “contre-coup” lesion of the posterior–inferior acetabulum due to levering out of the femoral head posteriorly.
FAI can present as isolated cam or pincer type but is most commonly a combined morphology with either the cam or pincer component being dominant. The radiographic criteria of the diagnosis for cam- and pincer-type deformities remain somewhat controversial. In cam-type FAI, the proximal femoral morphology includes asphericity of the femoral head or decreased head–neck junction offset. The location of the cam deformity is generally anterolateral but can involve more
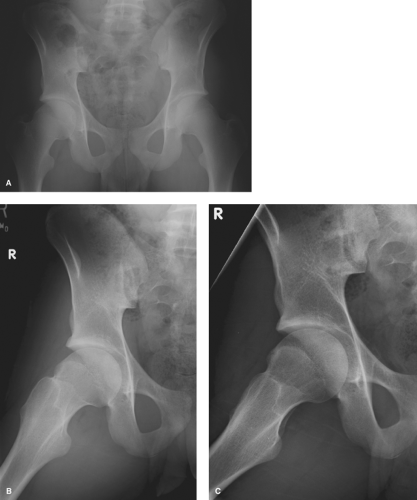
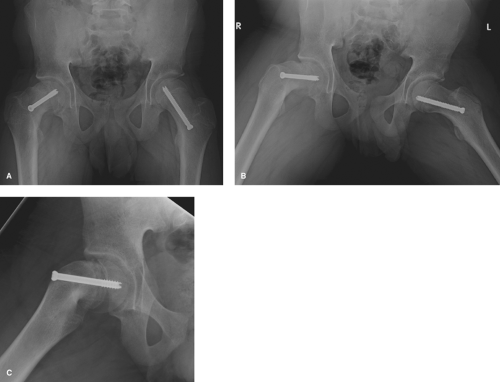
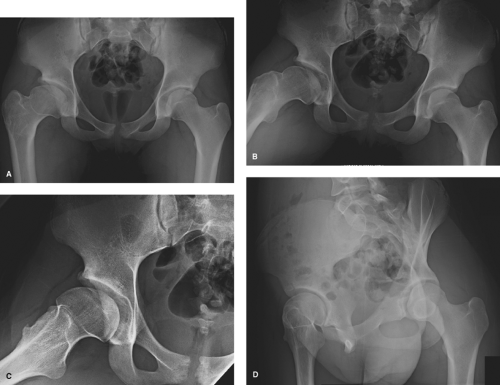
anterior or lateral portions of the head–neck junction in some cases (8,9). The etiology of cam-type morphology continues to be debated, but some cases may be because of childhood hip disease including slipped capital femoral epiphysis (SCFE) (Fig. 19.3) or Legg–Calvé–Perthes disease (Fig. 19.4). Recently, an association between the development of cam-type deformity and early aggressive sporting activities in adolescence has been suggested (10,11). In pincer-type FAI, acetabular deformity may be secondary to acetabular retroversion, focal anterosuperior rim prominence, or global overcoverage (Fig. 19.5). Acetabular retroversion is commonly due to deformity of the cranial aspect of the acetabulum (Fig. 19.6). Cranial retroversion causes relative prominence of the anterolateral acetabular rim leading to impingement. Acetabular retroversion is often a component of significant deformity of the entire hemipelvis, as suggested by protrusion of the ischial spine into the pelvic outlet (12) (Fig. 19.6). With global overcoverage, a generalized prominence of the
acetabular rim may lead to bony impingement in various positions, including hip flexion and internal rotation.
anterior or lateral portions of the head–neck junction in some cases (8,9). The etiology of cam-type morphology continues to be debated, but some cases may be because of childhood hip disease including slipped capital femoral epiphysis (SCFE) (Fig. 19.3) or Legg–Calvé–Perthes disease (Fig. 19.4). Recently, an association between the development of cam-type deformity and early aggressive sporting activities in adolescence has been suggested (10,11). In pincer-type FAI, acetabular deformity may be secondary to acetabular retroversion, focal anterosuperior rim prominence, or global overcoverage (Fig. 19.5). Acetabular retroversion is commonly due to deformity of the cranial aspect of the acetabulum (Fig. 19.6). Cranial retroversion causes relative prominence of the anterolateral acetabular rim leading to impingement. Acetabular retroversion is often a component of significant deformity of the entire hemipelvis, as suggested by protrusion of the ischial spine into the pelvic outlet (12) (Fig. 19.6). With global overcoverage, a generalized prominence of the
acetabular rim may lead to bony impingement in various positions, including hip flexion and internal rotation.
Symptomatic FAI requires a combination of underlying deformity that puts the hip “at-risk” and activities that require repetitive hip motion that produces impingement. Even in early descriptions, Ganz and colleagues acknowledged that FAI may occur in a patient with normal anatomy if the hip is subjected to extremes of motion. This situation is relatively uncommon and present only in the patient with activities that require extreme hip range of motion (such as ballet dancing) (1,13).
The History of Impingement
While Ganz et al. (1) elucidated the mechanism behind FAI, recognition of the association between subtle morphologic abnormalities in the proximal femur and the development of osteoarthritis is not new. Several authors have previously noted an association between subtle morphologic variations seen on radiographs and the development of osteoarthritis, and even suggested treatment strategies (14). The terms “tilt deformity” and “pistol-grip deformity” were given to deformities of the proximal femur, similar to those associated with FAI. While lacking a thorough understanding of the
mechanism linking these radiographic findings and osteoarthritis, many of the early ideas on the topic still hold true and some of the questions posed at that time remain unanswered.
mechanism linking these radiographic findings and osteoarthritis, many of the early ideas on the topic still hold true and some of the questions posed at that time remain unanswered.
Although acetabular dysplasia has been well established as a cause of hip osteoarthritis for some time, a large proportion of osteoarthritic hips have been traditionally classified as idiopathic. In 1933, Law noted “quite a number of cases placed in the primary osteoarthritis group are really the result of slight degree of slipping of the upper femoral epiphysis, which did not cause symptoms or signs during adolescence.” He later stated “this growth disturbance results in the femoral head becoming slightly distorted and the joint therefore mechanically imperfect—hence the occurrence of the wear and tear changes at a relatively early age such as the late 40s or early 50s.” In 1933, Elmslie noted the relationship between pre-existing hip deformity, including “the neck of the femur may be shortened and abnormally thick,” and the development of osteoarthritis.
In 1936, Smith-Petersen reported on the treatment of several patients with “impingement.” He describes a patient with acetabular protrusion who had pain from “impingement of the femoral neck on the anterior acetabulum … such impingement would result in ‘traumatic arthritis’ with characteristic changes of the joint surfaces” (14). He even describes treatment strategies that mirror those described many decades later. “If we could eliminate impingement, we should be able to eliminate the resultant reactions and, therefore, pain. To eliminate impingement two regions may be attacked, the neck of the femur and the anterior margin of the acetabulum.” The patients he treated primarily with “acetabuloplasty” as “to eliminate impingement by a plastic procedure on the neck of the femur would be impossible, since this would sacrifice too
large a portion of the neck.” Yet in two patients, he describes “a plastic procedure has been performed on the anterior femoral head and neck, when they have been the seat of advanced proliferative changes.” With acetubuloplasty, he felt that “by sacrificing a small portion” of the anterior wall of the acetabulum “a wide range of motion could be gained.” He additionally describes the use of acetabuloplasty in two patients with “old slipped upper femoral epiphysis.” He additionally treated eight patients with degenerative hip osteoarthritis acknowledging “if it is proved that this procedure does not give permanent relief, it may at least be useful in producing temporary relief and improved function over an important period of time.” He suggested application to “Legg–Calvé–Perthes disease” and “fracture of the neck of the femur with malposition” that mirror studies decades later. Regarding the outcomes of the patients he treated he stated “Sufficient time has not elapsed to obtain true end results, but the author feels justified … because the method is nondestructive and seems effective in relieving pain in conditions for which there is no other adequate treatment.”
large a portion of the neck.” Yet in two patients, he describes “a plastic procedure has been performed on the anterior femoral head and neck, when they have been the seat of advanced proliferative changes.” With acetubuloplasty, he felt that “by sacrificing a small portion” of the anterior wall of the acetabulum “a wide range of motion could be gained.” He additionally describes the use of acetabuloplasty in two patients with “old slipped upper femoral epiphysis.” He additionally treated eight patients with degenerative hip osteoarthritis acknowledging “if it is proved that this procedure does not give permanent relief, it may at least be useful in producing temporary relief and improved function over an important period of time.” He suggested application to “Legg–Calvé–Perthes disease” and “fracture of the neck of the femur with malposition” that mirror studies decades later. Regarding the outcomes of the patients he treated he stated “Sufficient time has not elapsed to obtain true end results, but the author feels justified … because the method is nondestructive and seems effective in relieving pain in conditions for which there is no other adequate treatment.”
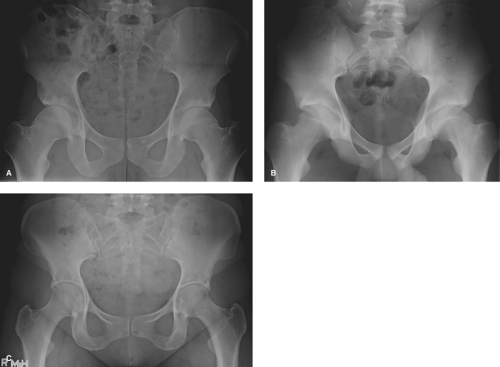 Figure 19.5. Pincer-type FAI variants. Three variance of pincer-type FAI are shown in this figure. An AP pelvis of a 23-year-old male (A) demonstrates a crossover sign with anterior superior acetabular overcoverage and associated femoral head–neck offset deformities. An AP pelvis of an 18-year-old male (B)
Get Clinical Tree app for offline access
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree


|