Femoroacetabular Impingement: Arthroscopic Management of the Acetabulum
Lisa M. Tibor
Jon K. Sekiya
Introduction and Definitions of Femoroacetabular Impingement
Surgical treatment for femoroacetabular impingement (FAI) is based on the idea that abnormal bony anatomy of the femoral head or acetabulum causes labral and/or cartilage injury with hip motion (1). This is in contrast to hip dysplasia where there is decreased contact area because of the maloriented articular surface of the acetabulum. As a result, the cartilage at the anterosuperior aspect of the femur and acetabulum is eccentrically loaded, exceeding the mechanical capacity of the cartilage, and ultimately causing early osteoarthritis (1).
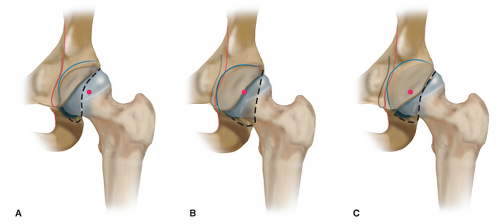
Cam impingement (Fig. 45.1) occurs when an aspherical portion of the femoral head, a “bony bump,” jams into the acetabulum during hip flexion. The shear force can result in abrasion of the acetabular cartilage or the labrum (1,2). Pincer impingement (Fig. 45.1) results from either focal or global overcoverage of the acetabular socket. During hip flexion there is linear contact between the labrum and the femoral head–neck junction, which causes a crush injury to the labrum.
Pincer Impingement: Global and Focal Overcoverage
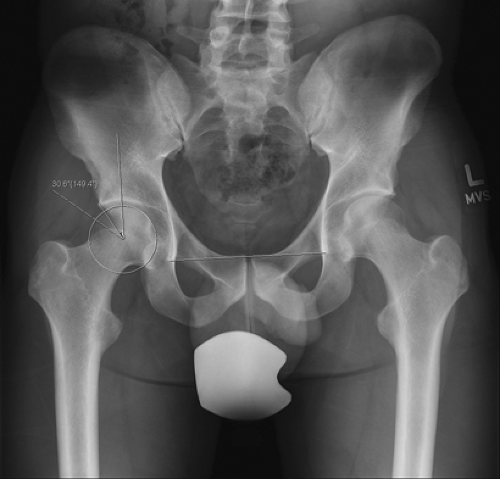
Center-edge angle (CEA) is a useful measure for defining both acetabular dysplasia (undercoverage) and global acetabular overcoverage causing pincer impingement (Fig. 45.2) (3). The CEA is defined as an angle formed by a perpendicular to the interteardrop line and the line passing from the center of the femoral head to the lateral edge of the acetabulum (4). An acetabulum with a CEA <20 degrees is considered to be dysplastic, with insufficient coverage and a risk of subluxation (3). An overcovered acetabulum has a CEA >35 degrees, which can cause pincer impingement between a normal femoral neck and the extended acetabulum with hip motion (3,5). Coxa profunda and protrusio acetabuli are two other terms that describe acetabular depth. These are defined based on the depth of the acetabular fossa on an AP pelvis x-ray relative to the pelvic ring. On the x-ray of a normal hip, the acetabular fossa lies lateral to the ilioischial line (Fig. 45.3) (6). In coxa profunda, the acetabular
fossa is deeper and touches or crosses the ilioischial line (Fig. 45.3) (6,8). However, several articles have shown that the depth of the acetabulum is not specific for the amount of acetabular overcoverage (5,9,10). As a result, CEA is now considered to be the more accurate determinant of global overcoverage. The deepest acetabular fossa occurs in protrusio acetabuli (Fig. 45.3) and occurs much more rarely than coxa profunda or global overcoverage. In a protrusio hip, the femoral head lies at or medial to the ilioischial line and the acetabular roof has a negative tilt. In addition, the center of the femoral head is medial to both the anterior and posterior acetabular walls (Fig. 45.3) (6,8).
fossa is deeper and touches or crosses the ilioischial line (Fig. 45.3) (6,8). However, several articles have shown that the depth of the acetabulum is not specific for the amount of acetabular overcoverage (5,9,10). As a result, CEA is now considered to be the more accurate determinant of global overcoverage. The deepest acetabular fossa occurs in protrusio acetabuli (Fig. 45.3) and occurs much more rarely than coxa profunda or global overcoverage. In a protrusio hip, the femoral head lies at or medial to the ilioischial line and the acetabular roof has a negative tilt. In addition, the center of the femoral head is medial to both the anterior and posterior acetabular walls (Fig. 45.3) (6,8).
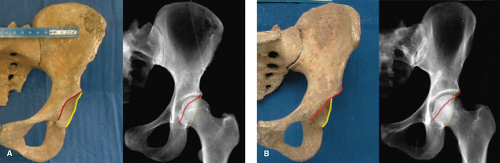
Focally increased acetabular overcoverage occurs as a result of acetabular retroversion. In a normal hip, the acetabular opening is anteverted (Fig. 45.4). When the acetabulum is retroverted, the anterior edge of the acetabulum is more lateral and the posterior edge is more medial (Fig. 45.4) (11). As a result, the relatively more lateral edge of the anterior acetabulum can cause pincer impingement when the hip is flexed (12). Acetabular retroversion can be either focal (also described as cranial) and due to relative overcoverage of the anterior–superior acetabular rim or global and due to rotation of the entire hemipelvis (13,14,15,16). This is a relevant question because it influences the recommended surgical procedure—for example, is the posterior coverage sufficient enough for arthroscopic anterior rim trimming or should the patient undergo an anteverting periacetabular osteotomy to improve posterior coverage and stability? Retroversion can also coexist with acetabular dysplasia (17,18) and in the dysplastic hip, retroversion was associated with the earlier onset of symptoms as compared to patients with dysplasia and a normally anteverted hip (17).
Radiographic Findings of Pincer Impingement
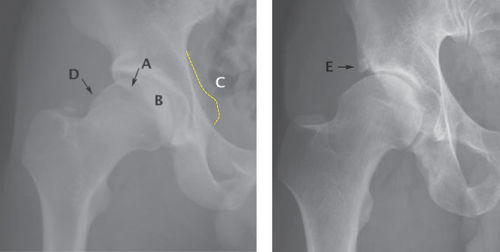
There are several radiographic findings that are indicative of probable retroversion and pincer impingement (Fig. 45.5).
Crossover sign: On the AP pelvis x-ray of a normally anteverted hip, the anterior wall of the acetabulum is medial to the posterior wall. In acetabular retroversion, the anterior
wall is lateral to the posterior wall at the superior aspect of the hip. The crossover sign occurs where the anterior line crosses over the posterior line (11,20).
Posterior wall sign: On the AP pelvis x-ray of an anteverted hip, the visible edge of the posterior wall is lateral to the center of the femoral head. In a globally retroverted acetabulum, the posterior wall is medial to the center of the femoral head (11).
Ischial spine sign: The ischial spine is the attachment of the sacrospinous ligament. It is more prominent on the AP pelvis x-ray and visible in the pelvic ring in patients with global acetabular retroversion. The ischial spine is
generally not visible in patients with normally anteverted acetabuli (21) or focal retroversion.
Acetabular rim fracture: Some patients with combined impingement can develop an acetabular rim stress fracture from the shear stress of the cam lesion impinging on the acetabulum (22,23,24).
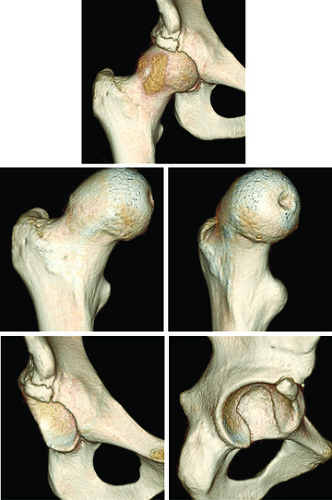
CT findings: A three-dimensional CT scan can be helpful for preoperative planning and better delineation of the bony anatomy associated with FAI (Fig. 45.6) (2,25). In particular, preoperative CT scanning can help determine if retroversion is cranial or central (26). A CT may also show fragmentation of a retroverted anterior wall or a cam lesion that was not visible on the AP pelvis x-ray (11,26).
Demographics
Isolated pincer impingement occurs predominantly in females (1). In Ganz’s original cohort of FAI patients, pincer impingement was more common in middle-aged women whereas young adult males were more likely to have cam impingement (1). Pincer impingement may, however, become symptomatic in adolescent patients who participate in sports or activities requiring an extreme range of motion (ROM), for example, dance or gymnastics (27). Combined cam and pincer impingement seems to occur with similar frequency in both males and females, generally making up slightly more than 40% of most cohorts (28,29). There may be an evolutionary reason for these demographic patterns. Examination of other mammal pelves reveals that cam morphology—a nonspherical femoral head on a short femoral neck—is common to mammals classified as “runners” and “jumpers” that require a sturdy hip but do not require much ROM (30). Conversely, mammals classified as “swimmers” or “climbers” and that require greater lower extremity ROM have rounder femoral heads. Because humans evolved from “climbers,” one hypothesis is that the “default femoral head” is rounder and that cam morphology in the human hip may be an adaptation in the evolution of humans as “running apes.” It has also been hypothesized that the increasing size of the human brain selected for pelvic width in females. A wider pelvis places the acetabuli farther apart and increases the abductor force necessary to maintain a level pelvis. If the acetabuli move relatively medial, the lever arm of the body weight shortens and reduces the required abductor force (30). This more medial position of the acetabulum results in coxa profunda (30).
The incidence of cam or pincer morphology appears to be quite high; in one asymptomatic cohort, nearly one-third of females and half of males had at least one predisposing factor for FAI (31). In addition, the majority of the findings were bilateral: 66% to 100%, depending on the specific morphology (31). The incidence of bilateral symptomatic FAI may be lower, on the order of 20% in some series (32).
Intra-Articular Pathology
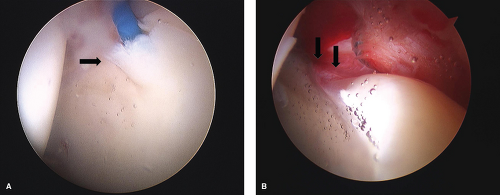
Because of the biomechanics of FAI and hip motion, the pattern of labral and/or cartilage damage seen arthroscopically is usually reflective of the underlying bony morphology. Cam and pincer impingement both have characteristic patterns of intra-articular damage and the arthroscopic findings should confirm the planned bony procedure to address the FAI. Cam lesions cause acetabular cartilage delamination in about two-thirds of patients, (Fig. 45.7) due to the shear force of the bony bump against the cartilage. The cartilage lesion is typically at the anterior or anterosuperior rim of the acetabulum, and is located posteriorly less often (32,33,34,35). Patients with isolated pincer lesions tend to have more circumferential labral damage consistent with a crush-type injury (Fig. 45.7) (32). They are less likely to have anterosuperior acetabular cartilage delamination (33,36). Acetabular overcoverage appears to be slightly protective for patients with combined cam and pincer impingement because the overcoverage may limit the entrance of the cam deformity into the acetabulum (33,37). If the cam lesion is not identified or addressed at the time of surgery, isolated acetabular rim trimming has the potential to accelerate degenerative changes by improving hip motion. Labral calcification is thought to be common in pincer impingement; however, it appears that the labral crush injury results in callus formation and reparative tissue at the acetabular rim. Histologic examination of tissue taken during open acetabular rim trimming showed bony apposition pushing the labrum away from the acetabular rim (38,34). This is seen
most often in coxa profunda and results in a “double line” or recess that can be seen on the plain radiographs. Evidence of new bone formation at the acetabular rim can also be seen on an MRI of the hip (34,38). Patients with pincer impingement may also have secondary posterior impingement as they lever against the anterior rim to gain ROM, sustaining a contrecoup injury to the cartilage (1). This may occur more frequently in patients with protrusio acetabuli given the bony constraints to hip motion (19).
most often in coxa profunda and results in a “double line” or recess that can be seen on the plain radiographs. Evidence of new bone formation at the acetabular rim can also be seen on an MRI of the hip (34,38). Patients with pincer impingement may also have secondary posterior impingement as they lever against the anterior rim to gain ROM, sustaining a contrecoup injury to the cartilage (1). This may occur more frequently in patients with protrusio acetabuli given the bony constraints to hip motion (19).
Goals and Indications for Surgical Treatment of the Acetabular Rim
The goals of surgical treatment for the acetabulum in FAI are to treat a painful labral or cartilage injury and address the underlying bony pathology. Surgical treatment is generally indicated after patients have failed to respond to 6 weeks to 3 months of nonoperative management. Patients with symptomatic FAI have significant muscular weakness around the involved hip (39), which may explain why some patients are less symptomatic than others. Although the results of nonoperative management have not been published, a course of physical therapy for core and hip strengthening, activity modification, and gentle ROM exercises may improve preoperative pain and function (8,40).
Experienced hip surgeons generally use some combination of ROM testing including internal and external rotation in flexion, passive supine external rotation, gait, single leg stance, straight leg raise, and special tests for impingement (41,42). The “impingement test” involves placing the hip in flexion, adduction, and internal rotation (FADDIR). This was the most commonly used diagnostic maneuver among examiners, but there was only about 60% agreement between the surgeons as to which patients had symptomatic FAI (41,42




Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree