Femoral Revision
Uncemented Implants With Bioactive Coatings
Jean-Pierre Vidalain
Key Points
• Planning: careful preoperative templating
• Instruments: specific and complete instrumentation
• Implants: system of fully HA-coated stems
• Fixation: as proximal as possible
Introduction
If the choice of cementless versus cemented implants for mild and moderate bone stock loss is still a topic of controversy, cementless femoral revision surgery for cases of severe deficiency has increasingly gained acceptance over the past decade.1–8
Revision following major femoral component loosening can be difficult, both in terms of finding a means of stable fixation of the revision implant and in terms of finding viable bone stock. Adequate primary stability must be attained to allow restoration of badly damaged bone around the new implant and to ensure the sound and lasting osteointegration of the new device.9–13 Stability will be dependent on the preoperative condition of the femur (e.g., granuloma, osteolysis, fracture, implant breakage) and on what happens at revision surgery (e.g., inadvertent perforation, fracture, cortical window, extensive femoral osteotomy). Hydroxyapatite is a naturally occurring mineral form of calcium with the chemical composition Ca5(PO4)3(OH). The crystal form of the material is composed of two crystals, thus yielding the composition Ca10(PO8)6(OH)2. Its osteoconductive properties have made it an attractive material for coating both primary and revision total hip arthroplasty components. This has led to successful fixation of hydroxyapatite (HA)-coated implants in the presence of well-vascularized native bone.14–17
All these considerations mean that specially designed devices will be required so as to attain the necessary primary stability and to find a solution to the individual patient’s needs. A whole system (Fig. 97-1) adapted to the different situations encountered in revision surgery must be considered.18 Nevertheless, on the femoral side, to accomplish the objective of stable implant fixation, we follow a step-by-step strategy, which with appropriate planning and adequate instrumentation and implants can be summarized as “replacing the initial stem by another with fixation as proximal as possible and as distal as necessary.”19 Although numerous techniques have been described to successfully achieve adequate fixation of the femoral stem in revision total hip arthroplasty (these techniques are covered elsewhere in this book), our preferred techniques utilizes HA-coated implants. The purpose of this chapter is to discuss the use of such implants in revision of the femoral component in revision total hip arthroplasty.
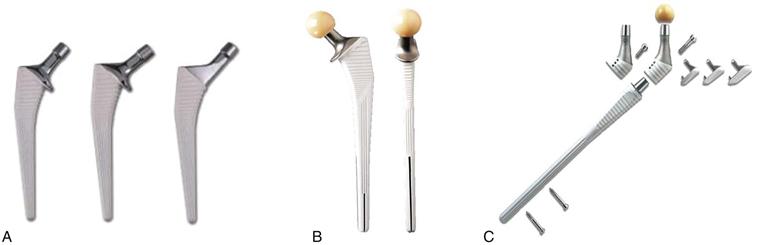
Figure 97-1 The CORAIL Hip System for revision surgery. A, The standard CORAIL series with different offset. B, The KAR implant with a collar support and two distal slots. C, The REEF prosthesis with different modular components and distal interlocking screws.
Indications and Choice of Implants
Implant stability is mandatory at the time of surgery: Successful femoral reconstruction with an uncemented stem requires immediate axial and rotational stability, and the implant must have intimate contact with the living host bone to promote osteointegration needed for definitive fixation. Stabilization depends on different bony lesions,20,21 but also on the shape of the distal femoral canal, where the bone of best quality is located. Three areas can be considered: the proximal part with its funnel-shaped cavity; the medial part with a canal that is more or less cylindrical; and the distal part characterized by gradual widening (Fig. 97-2).
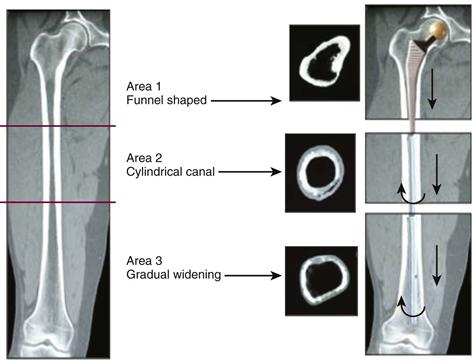
Figure 97-2 The choice of a revision implant according to the stability provided by remaining sound bone.
In area 1, a quadrangular implant with a double-tapered geometry will easily find its primary stability and will efficiently resist axial and rotational stresses. In Paprosky type 1 and 2A femurs, a stem designed for primary insertion provides reliable initial fixation. In such situations, our favorite implant is the CORAIL stem (DePuy, Johnson & Johnson, Warsaw, Ind), a grit-blasted straight device of quadrangular cross-section entirely plasma-sprayed with a 150-µm layer of pure HA (Fig. 97-1A). This stem has proved its value in primary hip arthroplasty.22–24
In area 2, even a strong diaphyseal fit provides only poor protection against the different forces. In patients with substantial bone loss (Paprosky types 2 and 3A), a longer revision stem, the KAR (DePuy), increases the bioactive area in contact with fresh bone, facilitating osteointegration (Fig. 97-1B). The KAR has the same proximally flared pattern as the CORAIL, but the stem is 25% longer to bridge bone defects or occasional windows. Two distal slots in the sagittal and coronal planes reduce global rigidity and prevent stress risers in the cortex at the tip of the stem.
In area 3, there is no possibility of finding effective mechanical stability through close contact between implant and bone. Interlocking screws must be used.25,26 The REEF (DePuy) is our dedicated implant for very severe deficiencies (Paprosky types 3B and 4) when very distal fixation is needed (Fig. 97-1C). The REEF is a modular device that is basically composed of two main elements. The first and more distal segment is a metaphyseo-diaphyseal element, conical in its proximal part and cylindrical in its diaphyseal part. The proximal zone is 100 mm high, with horizontal macrostructures to increase the surface of contact and to prevent subsidence. The distal zone, of variable length, has a slight bow to prevent anterior cortical contact, longitudinal grooves to enhance osteointegration, and several horizontal holes for locking with 5-mm diameter screws. The second and more proximal segment is a metaphyseal component fitted onto the stem with a Morse taper. This neck unit allows the surgeon to fine-tune anteversion within the confines of the existing metaphyseal bone and to restore leg lengths. In addition, this segment has an optional trochanteric claw that can be fixed to stabilize the greater trochanter and to improve the lever arm of the gluteal muscles if required.
The diagnoses that can lead to the use of HA-coated revision implants are not limited to aseptic loosening of different grades (Fig. 97-3); other possible indications are pertrochanteric fracture with cerclage of the greater trochanter, periprosthetic fracture, tumor resection, extensive osteolysis, and reimplantation in one- or two-stage exchange arthroplasty for the treatment of chronic infection at the site of total hip arthroplasty.27,28 Revision of implants for pain and severe stress shielding has also been discussed by some authors.18
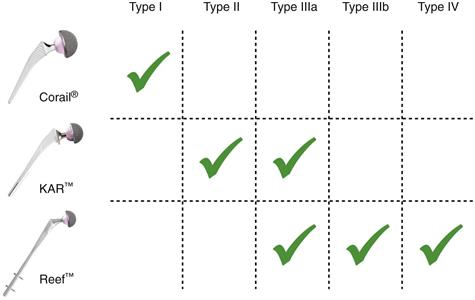
Figure 97-3 Indications algorithm according to types of femoral bone deficiency (Paprosky classification).
Preoperative Planning
Preoperative planning is essential to determine the appropriate size and alignment of the new implant and the length of the femoral neck component. For thorough preoperative planning, the surgeon will need a full set of revision implant templates and the following radiographs: an anteroposterior (AP) film of the entire pelvis and AP and lateral films of the affected femur. Considering the affected femur with its failed implant, successive templates are laid on the AP x-ray of the joint until optimal filling of the medullary canal is achieved and the new stem extends distally beyond damaged femoral bone and at least 2 cortical diameters distal to any osteotomy that is required to remove existing implants. This step determines the type and the size of the implant to be used. Although this is less reliable than in the primary situation, preoperative planning also enables the surgeon to identify any weak zones that will need to be bridged and to assess the quality of diaphyseal filling. Where necessary, the appropriate degree of calcar bone grafting should be established. The level of insertion of the new implant, with the greater or the lesser trochanter as reference, and the calcar height can be determined to ensure equal leg length. If a modular stem seems to be the appropriate implant, templating should assess the combination of components needed to achieve stability of the implant and to restore leg lengths. The location of eventual interlocking screws is also determined, keeping in mind that a minimum distance of 3 cm is needed between the distal extent of damaged bone and the first locking screw.
Technique
The surgical approach selected is mainly dependent on the surgeon’s preference and experience, keeping in mind that in the great majority of challenging situations, extraction of the failed prosthesis and reconstruction of extensive bone defects are often easier using a posterior approach, which is more extensile and more easily amenable than other approaches to the addition of femoral osteotomies.29
The acetabular surgery is usually carried out first, with replacement of the acetabular insert alone or of the entire cup system (the trial implants may be left in position or the final cup may be installed).
The femoral stage of surgery consists of several steps, as described in the following paragraphs.
Removal of the Failed Femoral Stem
This is generally easy if the stem is cemented, or if it is loose and uncemented, but may be more difficult if a well-fixed uncemented implant is in place.30 The best strategy should allow removal of the stem, cement, membrane, and debris, with minimal additional sacrifice of bone stock. Specific techniques for implant removal are described in detail elsewhere in this book.
Femoral Preparation
In cases of moderate bone loss, with an intact isthmus, the diaphyseal zone is prepared using rigid reamers of increasing diameter to create a femoral canal lumen of at least 11 mm (the distal diameter of all KAR stems). The metaphyseal zone must be reshaped to restore the quadrangular shape that guarantees the rotational stability of the CORAIL or the KAR stem. This is achieved by broaching the sclerotic bone with specific and progressively larger rasps (Fig. 97-4A). In addition, this aggressive broaching exposes more normal bone for osteointegration. The final broach must be longitudinally and rotationally stable in the femoral canal and corresponds to the size of the definitive CORAIL or KAR stem to be implanted. Anteversion must be carefully maintained during this phase to achieve stability of the implant. In case of bone loss distal to the femoral isthmus, or in case of an extended femoral osteotomy, once the bony flap has been opened, the failed implant and the surrounding cement, fibrous tissue, and debris may be removed. The intramedullary canal is cleared and curetted down to healthy bone. The diaphysis may have to be reamed sparingly to ensure that it is of the same diameter as the distal section of the stem chosen during templating. Accurate assessment of defects can now be established. The examination should focus on the condition of the cortices, the actual loss of bone stock, the presence of fractures, and any need for grafting. Decisions made during preoperative planning may be confirmed or altered.
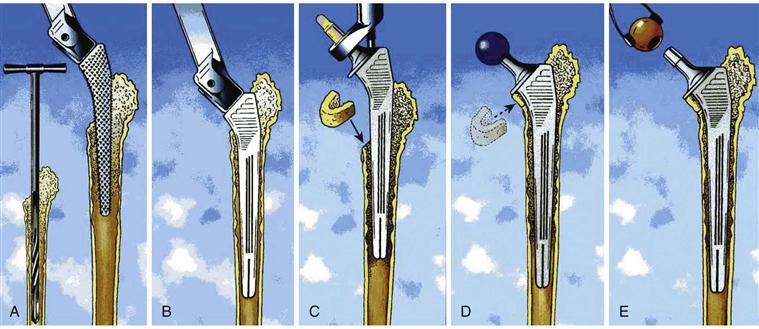
Figure 97-4 Surgical technique for a KAR implantation. A, Femoral preparation with rigid reamers and aggressive broaches. B, Insertion of the trial stem. C, Femoral component insertion. D, Calcar allograft stabilized by the collar of the stem and trial reduction. E, Definitive head impaction.
Insertion of the Trial Stem
With the CORAIL or the KAR option, the trial stem of the same size is introduced into the canal with the same anteversion. Similar to the final broach, the trial stem must be axially and rotationally stable (Fig. 97-4B). It should be positioned at the level decided during preoperative planning, relative to the greater or lesser trochanter. If the stem subsides, the femur should be examined for a perforation or a fracture, and if none is found, a larger trial stem should be used. If the stem remains proud of the planned implantation level, it must not be forced in. The trial stem must be removed and the femur broached again, with the final broach size keeping the same anteversion. If a window or a short femoral osteotomy has been made, this can be repaired using two or three cerclage wires before the trial stem is introduced into the femur. With the REEF option, the trial stem is introduced into the medullary canal at the depth estimated during templating (Fig. 97-5C). Stability within the remaining canal is not always perfectly achieved, even with a strong cortical press-fit. Ultimate rotational stability will be achieved after distal interlocking of the definitive implant. Nevertheless, with the stem in place, the chosen trochanteric component is fixed onto the cone of the femoral shaft, and one of three marks on this component is used to set anteversion.
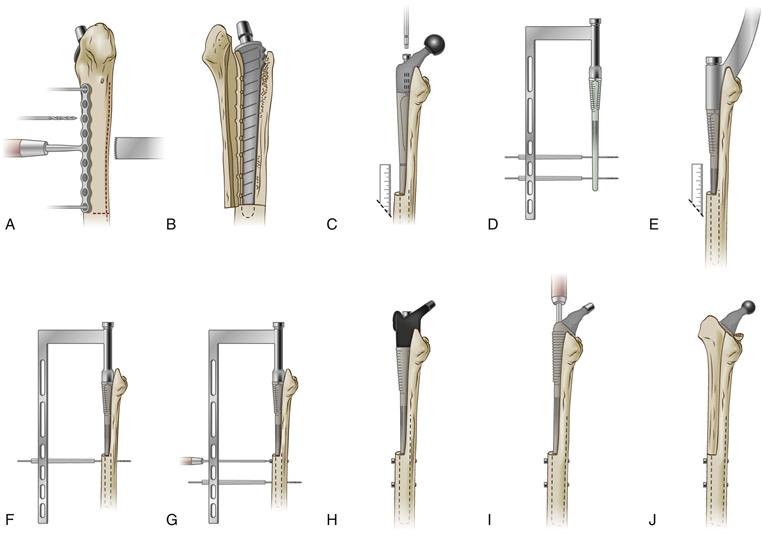
Figure 97-5 Surgical technique for a REEF implantation. A, The transfemoral osteotomy combines a posterior saw-cut, a transversal hemisection, and an anterior osteoclasis using a drilling template. B, The bony flap is gently opened. C, The trial stem is introduced to the depth predetermined during templating. D, Alignment of the interlocking holes is checked. E, Insertion of the definitive stem at the correct level, and (F and G) distal screw placement. H, Confirmation of the choice of metaphyseal segment. I, The definitive proximal body is impacted and fixed onto the stem cone. J, Reconstruction of the femoral shaft around the prosthesis.
Mobility and Stability Tests
Then, whatever the implant chosen, a trial head of a diameter matching the acetabular cup liner and a neck length selected during preoperative planning should be fitted on the taper, and a trial reduction carried out. The prosthetic construct is then tested for range of motion, stability of the joint, and tension of the gluteal muscles.
HA-Coated Implants and Bone Grafting
When a femoral revision is performed with HA-coated implants, bone grafting is not essential because the femur has the ability to heal and remodel itself.31 However, if the surgeon opts for grafting, autografts are preferred to allografts whenever possible,32 as long as their use does not cause additional morbidity. It must be noted that such grafts should never be used to stabilize the implant33 but only to fill in gaps around a stable stem and, more specifically, to seal the neck section to prevent the ingress of debris. At the calcar level, the main roles of a horseshoe-shaped cortical graft are to protect all HA coating that remains uncovered by the native bone, and to reduce the risk of HA particle migration into the vicinity of the joint space. Moreover, integration of this graft must not be underevaluated; very often, effective incorporation leads to restoration of normal or near-normal femoral bone stock. The KAR prosthesis is available only with a collar that contributes to stabilization of such a graft (Fig. 97-6). For similar reasons, a collared metaphyseal segment can be used with the REEF stem. To achieve osteointegration of bioactive implants, the coating of the stem must be in contact with reactive and living bone.34 Therefore, the CORAIL or the KAR must not be implanted using bone compaction techniques that require the use of compacted allograft. In the case of metaphyseal expansion, it is better to perform a longitudinal reduction osteotomy to move the remaining cortices closer onto the implant surface using cerclage wires, then to fill in the gap with allografts.
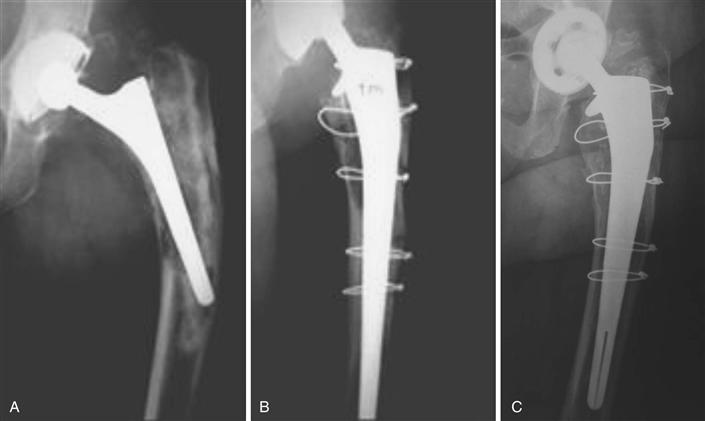
Figure 97-6 A, Revision with KAR prosthesis of an aseptic loosening, type 3A, of a cemented stem, associated with a periprosthetic fracture. B, Postoperative control; a horseshoe-shaped graft has been positioned under the collar, but no bone graft augmentation has been used to fill in the other defects. C, The last control at 12 years confirms the quality of the reconstruction with normal bone trophicity.
Implantation of the Definitive Stem
Once mobility and stability tests have been performed satisfactorily, final implants are confirmed and inserted to replace trial components. The trial stem is replaced with the final implant, which is introduced into the clean femoral cavity. It is important not to irrigate the medullary canal before inserting the definitive device to keep bone fragments in place and to preserve all osteoinductive cells. The CORAIL or the KAR is first introduced by hand, and then is progressively and gently impacted using a stem holder, which controls anteversion as the stem enters the femur. Before final impaction, it may be necessary to reconstruct the calcar using a crescent-shaped graft (see Fig. 97-4C through E). The collar of the prosthesis is designed to stabilize such grafts; this guarantees the correct impaction level of the stem and contributes to primary vertical stability until osteointegration occurs. If the modular interlocked stem (REEF) is used, distal screw placement is the critical step (see Fig. 97-5D through G). After impaction of the definitive diaphyseal component at the level of reference measured during trial reduction, the targeting device is firmly fitted onto the taper of the stem; this reliable instrumentation allows drilling and positioning of at least two interlocking screws with precision and safety. At that time, trial trochanteric components and trial heads can be used once again to confirm limb length, stability, and version (see Fig. 97-5H). Finally, the definitive proximal body is attached to the stem with the appropriate prosthetic head (see Fig. 97-5I). The final reduction is performed, and reconstruction of the femoral shaft around the prosthetic stem can be undertaken. Reattachment of the flap is achieved by means of cerclage cables (see Fig. 97-5J). As was already mentioned, grafting is not mandatory but may be desirable to rebuild the calcar or to fill cortical defects, and morselized cancellous bone should fill in any remaining cavities. However, it is recommended that the entire HA-coated area of the implant should be covered by native or grafted bone.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








