Chapter 9 Femoral Neck Fractures
Treatment of Nonunion
Nonunion is a relatively common complication of femoral neck fracture resulting from poor mechanical alignment of the fracture, failure of internal fixation, poor biologic factors, or infection. The precarious blood supply to the femoral neck and head may be the underlying reason for the poor healing potential of this fracture. Avascular necrosis of the femoral head is the other common and devastating orthopaedic complication associated with this fracture. These fractures have long been believed to represent an orthopaedic emergency requiring immediate intervention to prevent these complications. Displaced femoral neck fractures occur infrequently (only 3% of all hip fractures) in the young adult (i.e., <60 years of age); therefore, it is difficult to obtain adequate power to conduct a study to determine whether timing of intervention actually affects the rate of complications.1,2
This fracture occurs much more frequently in elderly patients; however, epidemiology, mechanism of injury, rates of complications, and treatment options are different for this age group. The incidence of nonunion of femoral neck fracture is approximately 18.5% for elderly patients and 8% for young patients.3,4 A meta-analysis by Bhandari et al (level I evidence) showed that arthroplasty for displaced femoral neck fractures in elderly patients was associated with a significantly lower rate of revision surgery as compared with reduction with internal fixation.3 However, arthroplasty was associated with longer operative times, greater blood loss, higher infection rates, and possibly higher early mortality rates (≤4 months following surgery). Despite controversies regarding the early management of these fractures, it is generally agreed that femoral neck nonunions in young patients should be treated with attempted salvage, whereas this complication in elderly patients should be treated with total hip arthroplasty.
Diagnosis and Preoperative Considerations
Factors that contribute to femoral neck fracture nonunions include vascular insufficiency, failure to obtain adequate fracture reduction (i.e., persisting coxa vara), posterior femoral neck fracture comminution, and inadequate internal fixation.5–7 In general, increasing patient age and fracture displacement correlate with increased risk of nonunion.8 Investigators have also suggested that vertical orientation of the femoral neck fracture leads to shear forces at the fracture site that, in turn, result in a greater rate of nonunion. The Pauwels classification is based on this principle; for example, type 3 fractures have a fracture line oriented more than 70 degrees to the horizontal.9 One study found that patients with Pauwels type 3 fractures treated with cannulated screws had higher rates of nonunion (19%) than did those treated with a fixed angle device (8%).10 This finding suggests that such fractures are inherently unstable and require very rigid internal fixation.
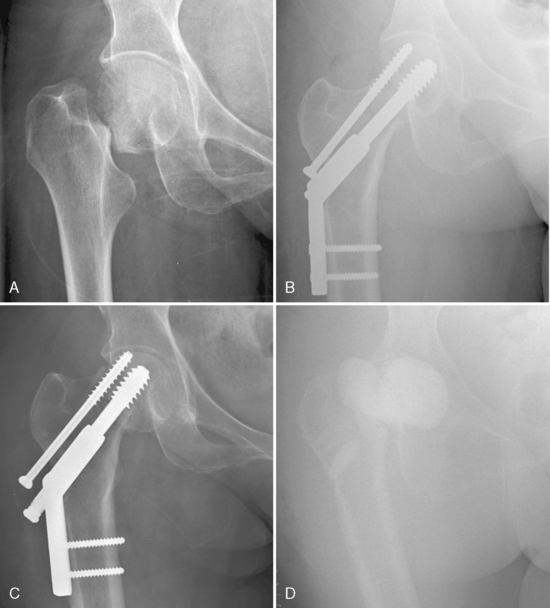
Avascular necrosis of the femoral head as a complication of femoral neck fracture seems to occur at a slightly greater rate than nonunion. Avascular necrosis also appears to be more common in young patients (≈ 25%) than in elderly patients (≈ 10%).1,3,4 This finding may reflect that fact that these are high-energy injuries in young patients and therefore involve significant soft tissue injury and disruption of the blood supply to the femoral head. One must always be careful to differentiate nonunion from avascular necrosis. Pain from femoral neck fracture nonunion occurs within several months after fracture, whereas pain from avascular necrosis manifests 1 to 2 years after fracture. Radiographs are useful in distinguishing between the two diagnoses. Alho et al11 suggested four radiographic signs, present at 3 months, that indicate femoral neck fracture nonunion: (1) change in fracture position by 10 mm, (2) change in screw position by 5%, (3) backing out of the screws by 20 mm, and (4) perforation of the screws into the femoral head. These four radiographic signs are illustrated by a case of septic nonunion shown in Figure 9-1. Computed tomography (CT) scan provides the best assessment of fracture union.
Radiographic changes are often absent in patients with avascular necrosis until the disease has reached an advanced stage. Bone scan and magnetic resonance imaging (MRI) have been investigated as methods of assessing femoral head viability after femoral neck fracture fixation. Bone scan has not been shown to predict the onset of avascular necrosis reliably within 1 year after fracture fixation.12 MRI may be an accurate method for diagnosing avascular necrosis in its early stages.13 However, the common application of stainless steel internal fixation precludes the use of MRI for diagnosis of avascular necrosis. When one is uncertain whether pain is the result of nonunion or avascular necrosis, it is best to obtain a CT scan to rule out nonunion. If nonunion is suspected, then a hip salvage procedure, such as a valgus osteotomy, should be performed. Avascular necrosis occasionally manifests after the hip salvage procedure, and, in this situation, the patient will require total hip arthroplasty.
Infection should always be considered as a potential cause of femoral neck fracture nonunion (see Fig. 9-1). The patient should be questioned regarding any constitutional symptoms, and the skin incision should be inspected for any signs of infection. Preoperative evaluation must include white blood cell count, erythrocyte sedimentation rate, C-reactive protein, and hip aspiration.14 Intraoperative tissue samples from the nonunion site should be obtained for frozen section at the time of any surgical intervention. If infection is suspected, then all hardware should be removed along with any necrotic bone or tissue. In most cases, the femoral head is necrotic and requires resection. A Girdlestone procedure is performed, and an antibiotic spacer is inserted as the first stage of a two-stage revision arthroplasty for infection (see Fig. 9-1D). The patient is given intravenous antibiotics chosen according to culture sensitivities for at least 6 weeks. Results of blood tests, including white blood cell count, erythrocyte sedimentation rate, and C-reactive protein, should normalize before the second stage of the revision is contemplated.
Salvage Procedures
The femoral neck also has a very challenging biologic environment. The femoral neck is an intracapsular structure contained within the hip joint; therefore, it does not have a direct blood supply from surrounding muscle tissue as does the femoral shaft. Cadaveric injection studies and radioisotope scans of the femoral head have shown that both intraosseous and extraosseous vessels supply the femoral head and neck.15,16 The major extraosseous blood supply to the femoral head comes from the medial femoral circumflex artery and its retinacular branches (inferior, posterior, and superior). The artery of the ligamentum teres supplies a negligible volume of the femoral head in most of the population. In displaced femoral neck fractures, blood supply to the femoral head and neck depends mainly on the extraosseous retinacular branches of the medial femoral circumflex. Certain surgical procedures have been designed to provide bone grafts to the area of a femoral neck nonunion to improve this biologic environment.
Proximal Femoral Valgus Osteotomy for Femoral Head Preservation
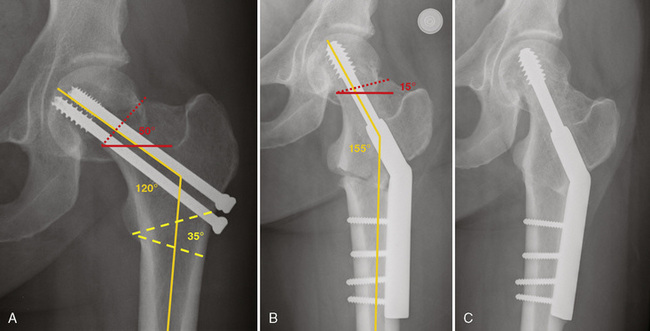
Young patients with femoral neck nonunion are candidates for valgus osteotomy. The objective of this operation is to improve the biomechanics at the fracture site by orienting the fracture line so that it is perpendicular to the force acting across the fracture site. Pauwels showed that the resultant force acting across the hip joint (i.e., the summation of gravity and hip abductor force vectors) is a force vector approximately 16 degrees from the vertical.17 For the femoral neck fracture to be oriented perpendicular to this resultant force vector, the femoral neck fracture line should be approximately 16 degrees from the horizontal. In clinical practice, planning the osteotomy so that the femoral neck fracture line is 30 degrees or less from the horizontal has resulted in high rates of union.18
The following description of a valgus intertrochanteric osteotomy involves the use of a dynamic hip screw for fixation of the osteotomy instead of a blade plate. Use of a dynamic hip screw for this purpose is well established in the literature.19–21 The dynamic hip screw device is very commonly used for trauma and is perhaps more familiar to most surgeons than the blade plate.
Planning the valgus osteotomy requires careful templating of an appropriate hip anteroposterior radiograph. The femoral neck-shaft angle must be determined (orange line in Fig. 9-2A), and the angle of the fracture line to the horizontal plane should be measured (red dotted line in Fig. 9-2A). As seen in Figure 9-2A, the femoral neck-shaft angle is 120 degrees, and the fracture line is 50 degrees to the horizontal. A laterally based wedge of 35 degrees (yellow dashed line in Fig. 9-2A) provides correction of the fracture line to 15 degrees from the horizontal. The apex of this wedge should be located at the distal aspect of the lesser trochanter. This ensures that the osteotomy is made proximal enough to be within metaphyseal bone (for improved healing) and distal enough to provide a large proximal fragment for fixation with a dynamic hip screw device. The osteotomy in Figure 9-1A was planned such that the proximal osteotomy exited the lateral cortex at the level of the previous cannulated screws.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree