Femoral Head Osteonecrosis—Proximal Femoral Osteotomy and Open Bone Grafting Procedures
Harpal P. Khanuja
Michael A. Mont
Aaron J. Johnson
Joshua E. Drumm
Samik Banerjee
Patient Case: Introduction and Radiographs
JN is a morbidly obese 38-year-old African-American male who presented with a 2-year history of chronic left hip pain. He describes it as a deep, intermittent throbbing pain not related to activity, and most localized to his groin. He drinks two to three alcoholic beverages nightly and smokes one pack of cigarettes per day. He denies any past surgical history. Physical examination reveals pain with active and passive range of motion of the left hip, particularly with internal rotation. The right hip was asymptomatic on examination. On further questioning, the patient also noted some pain in his right shoulder, as well as his left wrist, of similar nature to his hip pain.
Low anteroposterior pelvic (Fig. 57.1) and frog-leg lateral (Fig. 57.2) radiographs of both hips, as well as the right shoulder and left wrist, were obtained. On these radiographic views, the left hip demonstrated marked subchondral sclerosis with some cystic changes in the femoral head; radiographs of the right hip were normal in appearance.
MRI of the left hip (Fig. 57.3) demonstrated a medial lesion involving approximately 45% of the weight-bearing surface of the femoral head without evidence of collapse. MRI of the right hip (Fig. 57.4) demonstrated a lesion involving approximately 15% of the central nonweight-bearing surface of the femoral head. Cystic changes were also noted in the humeral head and distal radius, consistent with osteonecrotic changes in these areas.
MRI of the left hip (Fig. 57.3) demonstrated a medial lesion involving approximately 45% of the weight-bearing surface of the femoral head without evidence of collapse. MRI of the right hip (Fig. 57.4) demonstrated a lesion involving approximately 15% of the central nonweight-bearing surface of the femoral head. Cystic changes were also noted in the humeral head and distal radius, consistent with osteonecrotic changes in these areas.
 Figure 57.2. Lateral left hip radiograph of the same patient illustrated in Figure 57.1, showing osteonecrotic lesion of the femoral head. |
Introduction
Osteonecrosis of the femoral head, also known as avascular necrosis or AVN, can be a particularly devastating disease. It often affects younger patients (1,2) in the second to fifth decades of life. When a patient presents with hip and groin pain, it is important to consider other diagnoses. Femoroacetabular impingement, transient osteoporosis, femoral neck stress fracture, and osteochondritis dissecans should all be considered. Our primary differential diagnosis regarding the above patient’s left hip was atraumatic osteonecrosis, possibly with multifocal osteonecrosis, associated with his history of alcohol use and smoking. It is important to identify other painful joints in patients who are at risk, as 3% to 10% of patients may have “multifocal osteonecrosis,” where numerous joints (three separate anatomic sites) are affected (3). In this patient’s unique case, he also had asymptomatic progression of the contralateral hip, which has been found to progress to collapse in approximately 10% to 50% of cases, typically depending on the size of the lesion (4).
 Figure 57.4. Coronal T1-weighted magnetic resonance imaging view of the right hip demonstrating a smaller lesion, with similar characteristics to that shown in the left hip. |
There are multiple risk factors for the development of hip osteonecrosis, some of which were found in the patient described in our case report, as are described in detail in Chapter 19. Risk factors can be categorized as direct (e.g., trauma, blood dyscrasias [e.g., sickle cell disease] (5,6), Caisson disease, Gaucher disease, irradiation, and some autoimmune disorders (7,8,9,10,11,12)) and indirect (alcohol abuse and smoking (13,14,15), and chronic high-dose corticosteroid use (16,17,18,19,20,21)).
Once late collapse of the articulating surface has occurred, the only appropriate course of treatment is arthroplasty. However, precollapse disease, and some early postcollapse lesions can often be treated with various joint-preserving procedures. These essentially fall into three surgical treatment categories: core decompression or drilling, osteotomies, or open bone grafting procedures (i.e., nonvascularized and vascularized grafting). The treatment rationale for osteotomies and grafting techniques is distinctly different and will be discussed in detail in the following sections. For each of these categories of treatment options, we will provide an overview, indications and contraindications to treatment, a description of surgical techniques, and a summary of the reported outcomes.
Proximal Femoral Osteotomies
Introduction
One goal of a proximal femoral osteotomy (PFO) is to alter the biomechanics of the hip; in addition, some have
described that these procedures favorably alter the vascular supply to the femoral head. Treatment rationale is aimed at changing the area of contact stress on the diseased portion of the femoral head to a point on the articular cartilage that is disease-free and structurally stable during weight-bearing activities (22). In theory, this will alleviate the pressure on the degenerated articular cartilage and may lead to a decrease in symptomatology and prevent progression to collapse of the lesion.
described that these procedures favorably alter the vascular supply to the femoral head. Treatment rationale is aimed at changing the area of contact stress on the diseased portion of the femoral head to a point on the articular cartilage that is disease-free and structurally stable during weight-bearing activities (22). In theory, this will alleviate the pressure on the degenerated articular cartilage and may lead to a decrease in symptomatology and prevent progression to collapse of the lesion.
Since it was first described for the treatment of osteonecrosis nearly 40 years ago, numerous variations of PFO have been studied (23,24,25,26,27,28,29,30). These variations include varus or valgus wedge angulation osteotomy and transtrochanteric rotational osteotomies. All of these procedures are technically difficult and many have met with limited success in the United States. However, excellent results continue to be reported from Europe and Japan.
Angular osteotomies were originally described by Merle D’Aubigne in 1965 (25). Since this initial report, numerous authors have reported variable success rates in highly selected patient populations. Rotational osteotomies were originally described by Sugioka in 1978 (29). He continued to follow his initial cohort of patients, and determined that patients did best when the transposed intact area of the femoral head occupied more than 36% of the acetabular weight-bearing area (31). However, his strict inclusion criteria and technically difficult procedure have been difficult to reproduce in other reports (23,30).
Indications
Candidates for PFO should have smaller lesions, typically localized Ficat stage II or III osteonecrosis (24). In addition, the area of the femoral head that will become the new weight-bearing surface must have enough cartilage present for the procedure to be successful.
Contraindications
Patient selection should take into consideration factors that are associated with poor bone healing (kidney disease, chronic corticosteroid use, smoking, etc.). These comorbidities have been associated with poor prognoses, prolonged recoveries, malunions, and nonunions (32). Although varus/valgus osteotomies can be used in early postcollapse lesions, there should be no acetabular involvement, and lesions should be small- or medium-sized (typically less than 30% of the femoral head).
Surgical Techniques
Angular Osteotomies
The decision about which osteotomy to use is often dependent on the location and size of the lesion in the femoral head. For example, if the lesion is located in the medial femoral head then a varus-producing osteotomy is ideal. A varus-producing osteotomy will shift the weight-bearing axis from the medial femoral head onto the unaffected lateral portion of the femoral head. However, if the lesion is located on the anterosuperior femoral head then a valgus extension–producing osteotomy is required. Here, the weight-bearing axis of the patient’s hip will be shifted from the anterosuperior portion to the posteromedial portion of the femoral head.
Technique: Valgus Osteotomy
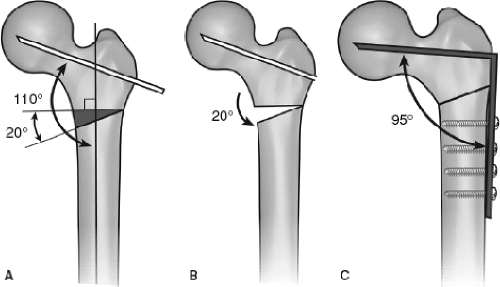
An anterolateral approach to the hip is used to provide exposure to the hip joint. A capsulotomy is performed taking care to leave the superior portion of the capsule attached to the greater trochanter. This allows the greater trochanter to hinge open after the osteotomy. Next, an osteotomy of the greater trochanter is performed. Guide pins can be inserted to obtain the desired valgus and flexion angles. The first intertrochanteric osteotomy is performed 1.5 to 2 cm inferior to the area of the planned blade plate insertion, and should be perpendicular to the femoral shaft. The valgus osteotomy is then performed using a combination of handheld osteotomes and power saws. The psoas tendon is then released from the portion of the lesser trochanter involved in the osteotomy. Fixation of the osteotomy is then performed with either a 95-degree blade plate or a fixed-angle device. The wound is then irrigated and closed (Fig. 57.5A–C).
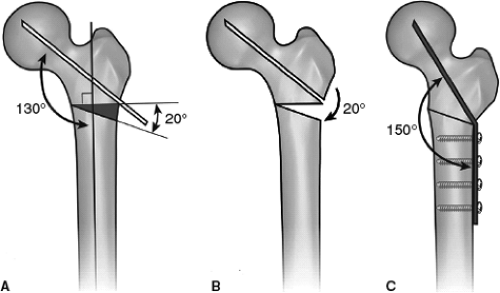 Figure 57.5. A–C: Technique of lateral closing wedge valgus osteotomy. Used with permission from Sinai Hospital of Baltimore, Inc. |
Technique: Varus Osteotomy
On a radiolucent table, the patient is placed supine and a bump under the operative hip. A direct lateral approach to the hip is utilized to gain access to the proximal femur. It is only necessary to expose the joint if a flexion osteotomy is to be performed as well. The first osteotomy is performed using a combination of power saws and handheld osteotomes perpendicular to the femoral shaft starting on the lateral cortex of the proximal femur at the level of the lesser trochanter. A wedge/triangular-shaped osteotomy is again made using a power saw with handheld osteotomes, starting on the lateral cortex at the level of the vastus ridge. The osteotomy is then fixed using a 95-degree blade plate or a fixed-angle device (Fig. 57.6A–C).
Rotational Osteotomies
Technique: Anterior Rotational Osteotomy
A lateral approach to the hip is used for exposure to perform a rotational osteotomy An osteotomy of the greater trochanter is then performed and reflected proximally while leaving the gluteus medius, minimus, and piriformis muscles attached. The lesser trochanter is then exposed and the medial femoral circumflex artery should be preserved, as its vascular pedicle is often found in close proximity to the osteotomy site. The main branch (deep branch) of the medial circumflex femoral artery is fairly constant and crosses posterior to the tendon of obturator externus and anterior to the tendons of the superior gemellus, obturator internus, and the inferior gemellus. The piriformis, short external rotators of the hip, and quadratus femoris muscles can be detached from the proximal femur at their respective insertions. While detaching the quadratus femoris muscle, it is important to keep in mind that the vascular pedicle is located under its distal fibers. In addition, it is important to release the obturator externus muscle completely from the proximal femur. Incomplete release can result in compression of the vasculature with the rotational osteotomy.
Guide wires are placed into the proximal femur to determine proper location for the osteotomy sites. One guide wire is inserted perpendicular to the anterior–posterior axis of the femoral neck at approximately 1 cm distal to the intertrochanteric crest toward the lesser trochanter. The second guide wire is inserted directly anterior to the first so that the two wires are parallel in the coronal plane and perpendicular in the sagittal plane. Another guide wire is placed parallel and distal to the second.
After circumferential capsulotomy, the femoral head is subluxed and the articular surface evaluated. The first transtrochanteric osteotomy is made perpendicular to the femoral neck in the coronal plane using the first wire as a guide for the osteotomy. The second transtrochanteric osteotomy is then performed starting at the most superior edge of the lesser trochanter and ending at the first osteotomy site. This angle should be greater than 90 degrees to ensure that the proximal and distal fragments have sufficient contact. Two pins are inserted, one in the proximal fragment and another in the distal fragment, and the proximal fragment is rotated to allow the unaffected portion of the head articulate with the weight-bearing dome of the acetabulum. The angle between the two pins after rotation is the rotation angle and usually varies between 45 and 90 degrees (Fig. 57.7A–D). The psoas tendon, obturator externus, vastus lateralis muscles, and capsule must be completely divided to ensure adequate rotation of the proximal fragment.
Once there is adequate contact between the proximal and distal fragments, the osteotomies are fixed using a sliding hip screw and side plate or some other type of internal fixation device (Fig. 57.7E). The osteotomy sites are trimmed to ensure that no bony impingement occurs. The wound is then irrigated and closed.
Technique: Posterior Rotational Osteotomy
A posterior approach is used to expose the hip for a posterior rotational osteotomy. The short external rotators and quadratus femoris muscles, along with the capsule are incised. Damage to the vascular pedicle must be avoided. An osteotomy of the greater trochanter is performed and reflected anteriorly. The vastus lateralis muscle must also be released from the hip capsule. Then, a circumferential capsulotomy is performed on the acetabular margin.
A guide wire is inserted into the center of the femoral neck through the greater trochanteric osteotomy site. Two
more guide wires are placed perpendicular to the axis of the femoral neck. The transtrochanteric osteotomy is now performed in two stages. The first osteotomy is made parallel to the second two guide wires in a proximal to distal direction. It begins where the first guide wire was inserted in the central area of the femoral neck and extends distally to the level of the superior portion of the lesser trochanter paralleling the second two guide wires. The second osteotomy is started just superior to the lesser trochanter on the medial femoral cortex and extends transversely to meet the first osteotomy. A pin is now inserted to control posterior femoral rotation. Fixation of the osteotomy is obtained by using a sliding hip screw and side plate, or a comparable device.
more guide wires are placed perpendicular to the axis of the femoral neck. The transtrochanteric osteotomy is now performed in two stages. The first osteotomy is made parallel to the second two guide wires in a proximal to distal direction. It begins where the first guide wire was inserted in the central area of the femoral neck and extends distally to the level of the superior portion of the lesser trochanter paralleling the second two guide wires. The second osteotomy is started just superior to the lesser trochanter on the medial femoral cortex and extends transversely to meet the first osteotomy. A pin is now inserted to control posterior femoral rotation. Fixation of the osteotomy is obtained by using a sliding hip screw and side plate, or a comparable device.
Results
Outcomes for PFO largely depend on surgeon and technique with success rates varying from 25% to 90% (Table 57.1). A potential drawback of PFO is the difficulty related with conversion to total hip arthroplasty if this becomes necessary. Currently, there is no consensus regarding the effects of PFO on subsequent conversion to total hip arthroplasty. There are some advocates of PFO that claim the procedure does not compromise outcomes after total hip arthroplasty. However, there are other investigators that suggest that outcomes after total hip arthroplasty are inferior when converted from previous PFO; there is certainly added morbidity while performing the procedure including increased operative time and blood loss. Fehrle et al. (33) reported on a series of 13 hips that had total hip arthroplasty performed after vascularized fibular grafting. They found that the residual graft prevented optimal canal fit of the femoral stem in 10 of the 13 hips, and 2 of 9 hips (22%) that had 2-year follow-up required revision procedures for femoral component loosening.
Numerous studies regarding varus-producing osteotomies have been reported, all with similar results (Table 57.1) (26,27,28,34,35,36,37,38,39,40). In a study by Pavlovcic and Dolinar (38) of 32 hips that had Ficat and Arlet Stage II or III disease and a mean follow-up of 17 years (range: 9 to 26 years), progression to collapse was delayed a minimum of 3 years in 23 hips (74%). Of those 23 hips, six went on to collapse by 8-year follow-up, 13 hips showed slowed progression of disease with mild arthrosis, and four hips showed no radiographic progression of disease at up to 26 years. Other reports, summarized in Table 57.1, show similar results, indicating the potential for delayed time to collapse of the femoral head in a majority of patients depending on stage of disease and degree of collapse at the time of osteotomy.
Japanese authors have noted the highest success rates using rotational PFO for osteonecrosis. Sugioka has widely published regarding his work with rotational PFOs in Japan and his some of his studies have shown greater than 90% survivorship past 10 years mean follow-up (29,31,41). His technique of a transtrochanteric rotational PFO allows for greater than 90% of rotational transposition of the femoral head. He recently reported on a series of 51 hips with an Association Research Circulation Osseous (ARCO) stage III and IV disease (late-stage disease). These patients were
treated with a posterior rotational PFO. At a 12-year mean follow-up, none of the patients required a conversion to total hip arthroplasty.
treated with a posterior rotational PFO. At a 12-year mean follow-up, none of the patients required a conversion to total hip arthroplasty.
Table 57.1 Proximal Femoral Osteotomy | ||||||||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|