FAI—Acetabular Retroversion
Martin Beck
Ralf Schoeniger
Introduction
Acetabular retroversion in the nondysplastic hip is one of the causes of pincer-type femoroacetabular impingent (FAI) (1,2) and has been implicated in the development of hip osteoarthrosis (OA) (3–6). The prevalence of acetabular retroversion in the normal population is 5% to 6% but this figure rises to approximately 20% in hips affected with OA (3,4). Aside from coxa vara, coxa profunda and protrusio coxae are other more common reasons for pincer FAI, both of which are related to global overcoverage of the femoral head. The treatment of global overcoverage includes resection of the overriding acetabular rim with preservation of the labrum (7–9). In the case of acetabular retroversion, an otherwise normal acetabulum is malpositioned within the hemipelvis (11,12). To correct acetabular malpositioning, a reorienting periacetabular osteotomy (PAO) appears to be the optimal treatment. Initially, the Ganz PAO was developed and designed to treat acetabular dysplasia and over time has become one of the most successful orthopedic procedures (12). When compared with other forms of pelvic osteotomy, the mobility of the osteotomized acetabular fragment in a PAO allows for better correction of acetabular orientation in all three dimensions (13). More recently, PAO has been successfully used in reorientation of the retroverted acetabulum (14,15).
Clinical Presentation and Examination
The clinical presentation is consistent with FAI. Groin pain, often radiating to the buttock, adductors, or knee, is the primary symptom. The pain can be reproduced by activities that involve forced hip flexion, adduction, and internal rotation. Such activities include swimming the breast-stroke, getting into or out of a car, and certain sports which require cutting or twisting maneuvers. In the later stages of the disease, a slight limp may be observed and pain may be present at rest. On clinical examination, flexion and/or internal rotation often are limited because of the prominent acetabular rim. The impingement test is typically positive reproducing the patient’s pain. Occasionally, patients present with pain localized exclusively to the posterior aspect of the joint, a possible explanation for which being stretching of the joint capsule because of subluxation of the femoral head in positions similar to those created during the impingement test.
Radiographic Findings
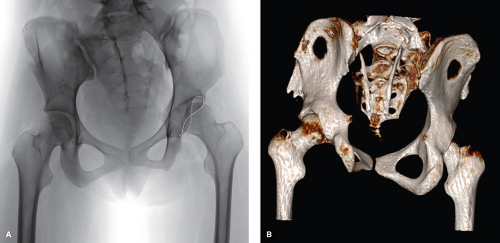
Radiographic examination includes standard anteroposterior pelvic and lateral hip radiographs. The center of rotation of the femoral head, lateral cover of the acetabulum, (center-edge angle) and the anterior and posterior rim of the acetabulum are identified. In addition, the position of the ischial spine relative to the ilioischial line is analyzed. Acetabular retroversion is identified by the presence of a crossover or figure-of-eight sign (14), a positive posterior wall sign (15), and projection of the ischial spine into the small pelvis medial to the ilioischial line (Fig. 40.1) (16).
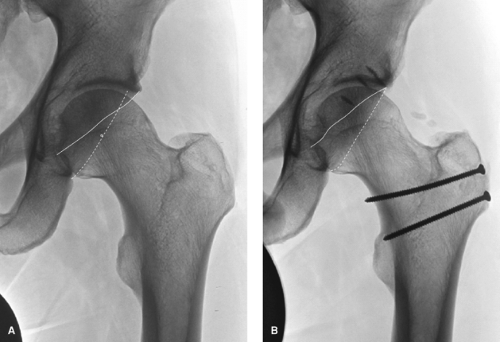
The crossover sign indicates that the acetabulum proximal to the crossing of the anterior and posterior rim faces posteriorly (Fig. 40.2A,B). The morphology of acetabular retroversion is inconsistent and the overlap of the anterior rim varies considerably (17). Normally, the caudal acetabulum is more anteverted than the cranial acetabulum. Jamali et al. (18) have shown, that if central anteversion, measured at the center of rotation, is greater than 20 degrees, cranial retroversion is present only exceptionally. If central anteversion measures between 10 and 20 degrees, approximately 38% of hips have cranial retroversion. In cases with a central anteversion of less than 10 degrees, all hips will have cranial retroversion. Another study showed a reduced central anteversion of 14 degrees in hips with acetabular retroversion, compared to 20 degrees in normal hips (14). Attempts have been made to quantify retroversion. The quotient between the length of overlap of the anterior rim and the entire length of the lateral acetabular opening is expressed as a retroversion index. An index of less than 5% is considered clinically not relevant (17).
The posterior wall sign describes the relationship of the posterior rim to the center of rotation. In a normal hip the center of rotation projects onto the posterior rim. In acetabular retroversion the posterior rim is medial to the center of rotation.
An anatomic study demonstrated that in acetabular retroversion the acetabulum faces posteriorly but that the size and shape of the acetabulum is otherwise normal (10,11). These findings were supported by 3D-CT data, which has demonstrated that retroversion involves the acetabulum at all levels and includes the entire pelvic segment containing the acetabulum and the ischial spine (11). This finding explains projection of the ischial spine into the “small” pelvis in acetabular retroversion. The projection of the ischial spine sign medial to the ilioischial line (positive ischial spine sign) is directly related to the degree of retroversion (16).
All these radiographic parameters described above are highly sensitive to alterations in pelvic orientation and inclination. A standardized radiographic technique must be employed whereby the film-focus distance measures 1.2 m, and the central beam is directed to the midpoint between a line connecting both anterior superior iliac spines (ASISs) and the superior border of the symphysis (19,20,21). Any deviation from this standard will cause a distorted projection of the acetabular contours and make interpretation useless.
Because of the divergence of the x-ray beams retroversion is overestimated on conventional radiographs. The magnitude of overestimation averages 4 degrees (range: 3.2 to 4.5 degrees) (18).
Differential Diagnosis of Acetabular Retroversion
Acetabular retroversion has to be differentiated from focal anterior overcoverage (Fig. 40.3A). The common feature of both conditions is the presence of a crossover sign. However, other than in retroversion the posterior
wall sign is negative, indicating a normal posterior rim and cover. In anterior overcoverage, the acetabulum has excess anterior rim. Treatment of overcover involves open or arthroscopic resection of the prominent anterior rim (Fig. 40.3B).
wall sign is negative, indicating a normal posterior rim and cover. In anterior overcoverage, the acetabulum has excess anterior rim. Treatment of overcover involves open or arthroscopic resection of the prominent anterior rim (Fig. 40.3B).
Mechanism of Impingement
Acetabular retroversion as well as anterior overcoverage is considered to be a cause for pincer FAI. Depending on the shape of the proximal femur, FAI may be pincer alone or a combination of cam and pincer. A spherical femoral head–neck junction will result in pincer FAI (Fig. 40.4), with an aspherical head–neck junction on the other hand causing cam FAI (Fig. 40.5




Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree