26
Extravasation Injuries
Leon S. Benson
History and Clinical Presentation
After giving birth, a 26-year-old woman became acutely hypotensive from postpartum bleeding. Despite initial efforts at fluid resuscitation, she developed hypovolemic shock and subsequently was the recipient of massive volumes of intravenous fluids and blood to save her life. At one point an infusion pump was used to aid in rapid administration of electrolyte solution. Efforts to resuscitate her were successful and she was then transferred from the maternity ward to the intensive care unit (ICU). It was noted shortly after transfer to the ICU that her left forearm was swollen and discolored, but no further assessment of the extremity was performed at that time. Nursing notes indicated that despite the forearm appearance, peripheral pulse remained “good.” The patient was intubated and heavily sedated.
About 8 hours after transfer to the ICU, it was noted that the patient’s left forearm and hand were massively swollen and blue. The hand surgery service was then consulted.
PEARLS
- Fluid extravasation injuries that present with a diameter of less than 10 cm and have induration and redness as the primary findings are generally less severe and can often be treated with elevation and ice.
- The incidence of doxorubicin hydrochloride (Adriamycin) extravasation injury is ∼3% of those patients receiving the drug. The incidence of extravasation injury from any chemotherapy administration is ∼6%.
- The pain associated with a chemotherapy extravasation can be a significant long-term problem. Surgical excision of the affected area often greatly improves the patient’s quality of life, even for those individuals who are quite ill already. Excision also diminishes the likelihood or severity of joint stiffness and sympathetic dystrophy.
- Because of their low osmolarity and less direct cytotoxicity, nonionic radiographic contrast agents (such as iohexol) are safer and better tolerated than traditional ionic agents (such as diatrizoate meglumine).
Physical Examination
Massive swelling was noted from the left elbow to left hand with severe ecchymosis throughout the dorsal forearm. The patient was obtunded, and no pain responses could be elicited. Radial and ulnar pulses were easily palpable at the wrist. The entire forearm reflected “rock-hard” soft tissue tension. A hospital identification bracelet that had been around the left wrist was extremely tight and at this time was removed. Furthermore, an automatic blood pressure cuff had been placed at the left upper arm and had been cycling on and off every 20 minutes to check the patient’s blood pressure. This cuff was also removed and relocated elsewhere. It was also noted that an intravenous catheter (20-gauge) had been placed into the dorsal wrist to aid in rapid fluid replacement earlier in the day. This catheter was now removed and fluid could be seen leaking from the site. Later review of the catheter, IV tubing, and fluid bags revealed that epinephrine-containing solution had also been administered through this intravenous site.
Diagnostic Studies
Plain radiographs of the elbow, forearm, and hand showed no fractures or other bony abnormalities. There was no gas or contrast media in the soft tissues.
Compartment pressures of the dorsal and superficial volar forearm compartments were checked. The dorsal compartment pressure was 131 mm Hg and the volar compartment pressure was 125 mm Hg. Clear fluid began leaking from both puncture sites after compartment pressures were measured.
No other diagnostic studies were pursued at that time.
Differential Diagnosis
Forearm compartment syndrome due to intravenous extravasation
Forearm compartment syndrome due to chronic compression
Forearm ischemia due to proximal vascular occlusion
Forearm muscle necrosis due to sepsis or localized infection
PITFALLS
- Intravenous infusion pumps can be particularly dangerous because they can inadvertently force fluid into an extravascular space, producing a compartment syndrome. Pediatric patients can be especially at risk for pump-related problems since the automatic shut off pressure of the pump may be gauged for adult physiology.
- A specific protocol for administration of doxorubicin hydrochloride (Adriamycin) should be followed. Preventable problems have been identified as producing extravasation events, such as failure to release a proximal tourniquet, use of poor veins, or infusion administered under pressure. Small-diameter polyethylene catheters are better than sharp needles, which tend to puncture the posterior vessel wall.
- Application of heat to an extravasation injury is not indicated. It will produce vasodilation, increased interstitial edema, increased swelling, and periarticular stiffness. Use of cool compresses and strict elevation is much better for immediate care.
Diagnosis
Forearm Compartment Syndrome Due to Intravenous Extravasation
The prognosis for extravasation injuries can be characterized by four key variables: (1) the volume of material extravasated, (2) the type of material that has extravasated, (3) the amount of time that extravasated material has been present (also called the “necrosis interval”), and (4) the susceptibility of the host to injury.
Loth et al (1991) have classified the severity of extravasation into three types (mild, moderate, and severe) based on the amount of extravasated agent. Mild extravasations present with minimal swelling and pain and represent small volume injuries. No blistering or redness is present and the patient can be treated with elevation of the extremity and a compression dressing. Moderate extravasations present with an area of soft tissue inflammation of 10 cm in diameter or less. Significant local tenderness and pain are present, although narcotics pain medication is rarely required. Some erythema may be present but blistering of the skin is absent. Moderate injuries are usually caused by extravasation volumes of 1 to 5 cc. Again, conservative measures such as elevation, cool compresses, and a compression dressing constitute the main form of treatment, although the patient may have residual symptoms for up to a month after injury.
Severe extravasation injuries typically result from large volumes of agent and produce severe pain and local soft tissue changes, such as blistering, erythema, and dramatic swelling. Compartment syndrome may result, which would require immediate fasciotomy. In the absence of compartment syndrome or other vascular compromise, specific management of severe extravasations is influenced heavily by the type of extravasated agent involved.
The type of extravasated agent constitutes the second major variable that influences prognosis for these injuries. Extravasated agents can be grouped into two main categories: vesicants and nonvesicants. Vesicants are materials that can produce local tissue necrosis. Chemotherapy drugs are an example of vesicants, with doxorubicin (Adriamycin) and mitomycin commonly producing dramatic local tissue necrosis. Calcium solutions, potassium solutions, fluorescein, sodium bicarbonate, and radiographic contrast media are also examples of vesicant agents. Some vesicant agents produce tissue necrosis via specific cellular mechanisms, such as inhibition of DNA synthesis, whereas other vesicants, such as electrolyte solutions, produce hyperosmolar states and cause cell death by fluid shifts or dramatic pH changes. Many vesicants are capable of producing a deep level of tissue necrosis that may take days or weeks to demarcate.
Two particular vesicant agents merit special mention. Vasoconstrictor drugs that extravasate can be particularly dangerous, producing either a compartment syndrome or severe local ischemia and tissue death. Local injection of phentolamine may reverse ischemia and prevent disaster. Ultimately, surgical drainage may be required if ischemia cannot be reversed within 3 to 6 hours. Radiographic contrast is another common vesicant agent that can produce local tissue death. Obtaining a radiograph of the involved extremity can be helpful in delineating how much tissue is affected. In cases where more than 20 cc of contrast is involved, surgical decompression is usually indicated; postdrainage radiographs should be obtained to confirm satisfactory removal of the contrast material.
Nonvesicant agents do not typically produce local tissue necrosis but do have the potential to cause significant inflammation; these agents are also sometimes called “irritants.” Examples of nonvesicant agents include blood products, Valium, methotrexate, and albumin. Most nonvesicant extravasations can be treated non-operatively as long as circulation is not compromised and large volumes of agent are not involved.
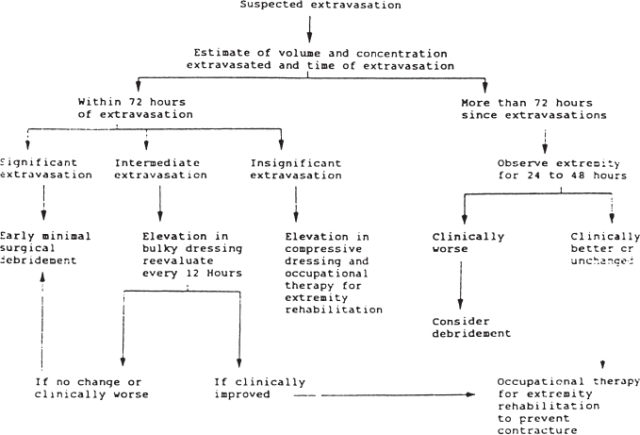
Figures 26–1, 26–2, and 26–3 illustrate treatment algorithms for managing extravasation injuries due to chemotherapy agents, radiographic contrast materials, and vasoconstrictive drugs, respectively.