Fig. 3.1
Erythema nodosum of limbs: symmetrical, erythematous, tender, rounded and oval nodules
The peak incidence is closed to the 20–30 years of age and the sex ratio favours females (3–6 times). The clinical picture is always that of a nonspecific systemic illness with mild-grade fever (in 60 % of cases with 38–39 °C), arthralgias (60 %), sometimes arthritis (30 %) and fatigue, while associated illness, in case of any, may prevail the presentation. It is consensually agreed that EN is a hypersensitive reaction to different antigenic stimuli and can therefore occur within the course of many diseases including infections, inflammatory and immune disorders, malignancies or drug therapy. However, an underlying aetiology cannot be found in about half of cases [1].
Differential Diagnosis
Differential diagnoses: insect bites, erysipelas, erythema induratum (nodular vasculitis), urticaria, thrombophlebitis.
Biopsy
In the large majority of cases, which exhibit typical EN, there is no indication to perform a skin biopsy. The dermatological diagnosis is based on clinical features. However, in very few atypical cases of unusual presentation, a skin biopsy can be performed to rule out other diagnoses. Histopathologically, erythema nodosum is a septal panniculitis (Fig. 3.2a), which is characterised by inflammation of fibrous septa between fat lobules variably spreading into the lobules, septa being thickened [2, 3]. Inflammatory cells often extend to the periseptal areas of the fat lobules. Direct immunofluorescence studies have shown deposits of immunoglobulins in the blood vessel walls of the septa of subcutaneous fat. At early stages, lymphocytes and macrophages dominate but neutrophils are often present (Fig. 3.2b). Oedema, fibrin deposition and foci of vasculitis may also be seen; at later stages, fibrosis dominates (Fig. 3.2c). In some cases, giant cells may be present, located around clefts in collagen. Miescher’s granuloma is unconstant but prototypical of EN and is formed by more or less radially arranged macrophages, often around cleft-like defects of septal collagen.
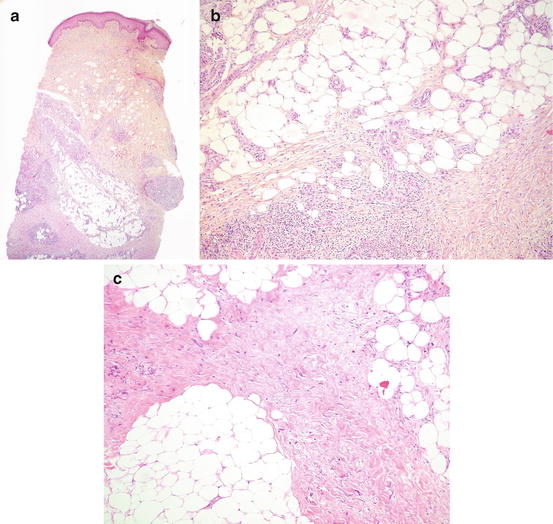
Fig. 3.2
(a) Erythema nodosum characterised by septal panniculitis (X50). (b) The inflammatory infiltrate is made of lymphocytes admixed with few neutrophils, and extends in the periseptal part of the fat lobules (X100). (c) A septal fibrosis without inflammation is seen in this late lesion of erythema nodosum (X100)
Some series have reported the characteristic of EN patients seen in rheumatology (Table 3.1). A series from Greece included 110 patients (83 % women, mean age 41.0 ± 14.0 years) [4]. Sarcoidosis was diagnosed in 28 % of the patients, infections in 17.3 % and tuberculosis in 1.5 %. Other aetiologic factors were Adamantiadis-Behçet’s syndrome (3.8 %), pregnancy (6 %), oral contraceptives (3.8 %) and other drugs (3.8 %). The aetiology of EN was not found in 35 % of the patients. Among 100 Turkish patients [2], the leading aetiology was poststreptococcal (11 %), followed by primary tuberculosis (10 %), sarcoidosis (10 %), Behçet’s syndrome (6 %), drugs (5 %), inflammatory bowel diseases (IBD) (3 %) and pregnancy (2 %), but nearly half (53 %) of the cases had undetermined aetiology. Recurrences occurred in patients having primary EN in 62 % (33/53) of patients. The outcomes were usually favourable within 7 days, patients being at bed rest and receiving nonsteroidal anti-inflammatory drugs, together with specific treatment for patients with an underlying disease.
Table 3.1




Aetiologies
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








