Chapter 134 Economics of Total Knee Arthroplasty
The increased expenditure for TKA costs health care payers billions of dollars each year and the cost of TKA has become a concern, in spite of its clinical success. In 2008, $2.4 trillion was spent on health care in the United States and health care as a percentage of the gross domestic product (GDP) increased to 17%. This percentage is expected to continue to increase to 20% of GDP in 2010.1,2
Epidemiology
Primary TKA has been demonstrated by clinical studies to yield successful surgical results and satisfactory patient outcomes in more than 90% of patients at 10 years.3,4 Furthermore, TKA is a cost-effective means of alleviating pain, restoring function, and improving quality of life for patients with advanced arthritis of the knee that cannot be treated satisfactorily with nonoperative treatment.
In 2008, approximately 602,600 TKA were performed in the United States, of which 483,495 TKAs (80.2%) were done for Medicare patients.5 The growth of TKA is underscored by the fact that 40,000 TKA operations were performed in 1980, 138,552 in 1990, 308,250 in 2000, and 602,600 in 2008. Demand for primary total knee arthroplasties is projected to grow by 673% to 3.48 million TKAs by the year 2030 (95% confidence interval [CI], 2.95 to 4.14 million TKAs).6
Primary TKA can fail for several reasons, including improper surgical technique, infection, bearing surface wear, osteolysis, loosening, implant breakage, and fracture. Factors such as diabetes, smoking, malnutrition, obesity, and patient noncompliance can contribute to the failure of primary TKAs. These factors, coupled with the increasing number of primary TKAs being performed, has resulted in an increased prevalence of revision TKAs—11,369 revision TKAs in 1990, 19,138 in 1995, 26,926 in 2000, and 38,300 in 2005. TKA revision operations are projected to grow 601% to 268,200 in 2030 (95% CI, 192,700 to 381,400).6
Reimbursement
Surgeon
Professional reimbursement for orthopedic surgeons for primary and revision TKA has decreased considerably since 1991. In 1991, the average Medicare reimbursement to orthopedic surgeons for a primary TKA was $2250 and, for a revision TKA, $2700. By 2009, professional payment from CMS for TKA dropped to $1456 for a primary TKA and to $1677 for revision TKA. This represents a 35% decrease in professional reimbursement for primary TKAs and a 38% decrease in professional reimbursement for revision TKAs from 1991 to 2009.7
To the best of our knowledge, erosion of surgeon payment for TKA has occurred without affecting the quality of the TKA operation or access to the operation. It is not clear how long this will continue. Health care personnel assessments predict an insufficient number of subspecialty trained knee surgeons to meet the demand for TKAs in 2020.8 Decreasing professional payment for TKA may be associated with the decreasing numbers of orthopedic residents who choose to specialize in knee replacement surgery. Furthermore, it is not clear how low TKA surgeon payment can go before surgeons object to additional decreases by limiting TKA surgery, which could further reduce patient access to TKA. By any measure, TKA has proven to be one of the most successful medical treatments of the last half-century. It is not known why these successes have been associated with a paradoxical reduction in payment for service.
Hospital
Diagnosis-Related Group Payment
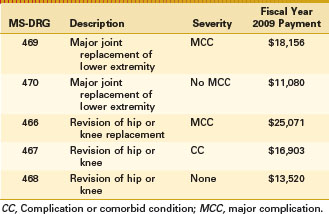
Hospitals are reimbursed for their services to Medicare patients by a single DRG payment according to a specific diagnosis (ICD-9 code). Since the advent of this system in 1983, primary and revision TKAs were paid according to the same DRG 209 payment scale (major joint replacement) regardless of the diagnosis, complexity of the procedure, or patient’s health status at admission. In 2005, DRG 209 was split into DRG 544 (Primary Hip and Knee Replacement) and DRG 545 (Revision Hip and Knee Replacement) to reflect the higher resource utilization and cost associated with performing revision joint arthroplasty. In 2007, Medicare subdivided primary and revision joint replacement to account for the presence or absence of a major complication or comorbidity. The new payment groups are shown in Table 134-1.
Medicare pays for approximately 80% of knee replacement operations in the United States. Of these, 86% are paid according to the MS-DRG payment system, whereas 14% are reimbursed at a lower rate by managed Medicare programs. In 2008, MS-DRG 470 accounted for the largest CMS payment to hospitals, accounting for 4.6% of all Medicare payments.9 As noted, the magnitude of the CMS expense for TKA is explained by the rising prevalence of the operation and the increasing cost of TKA operations.
In an effort to control Medicare expenditures, CMS has limited hospital reimbursement for primary and revision total joint arthroplasty. In 1993, the average DRG payment for a primary TKA was $9645. The DRG payment rose to $11,080 in 2009. This represents a 15% increase in reimbursement between 1993 and 2009. However, inflation rose 49.5% during this time period.10 CMS payment for revision total knee arthroplasty has followed a similar pattern, with a 2005 payment of $12,791 rising to $13,520 in 2009. This represents a 5.7% increase in hospital reimbursement as compared with an inflation rate of 10.6%. In an attempt to control Medicare spending, CMS is limiting increases in hospital payment for TKA to less than inflation.
Indirect Medical Education Payment
In addition to the DRG payment, the actual reimbursement a hospital receives for a TKA is different for private and teaching hospitals. If the hospital is an approved teaching hospital, it receives an additional payment for each case, known as an IME adjustment. The amount varies depending on the size of the teaching hospital and uses a formula based on the ratio of residents to beds (Table 134-2). In the example shown in this table, the IME percentage is 16.7%, which would account for a $1850 payment for an uncomplicated primary TKA in 2009 (MS DRG 470, $11,080).
Table 134-2 Medicare Calculation to Determine Cost of Indirect Medical Education*
| Parameter | IME Calculation Example (%)† |
|---|---|
| Total hospital interns and residents | 100 |
| Total hospital beds available | 300 |
| Ratio of hospital beds to interns and residents | 33.33 |
| Medicare multiplier (same for all acute hospitals) | 1.35 |
| IME percentage add-on† | 16.7 |
† IME formula = 1.35 × ([1 + ratio of beds to residents] § 0.405) − 1).
Capital Payment
Hospital Expense for Total Knee Arthroplasty
At the Lahey Clinic in Massachusetts, there are 18 service centers that contribute to the overall cost of a TKA admission (Table 134-3). A service center is an accounting group, such as the operating room, laboratory, or radiology department, for which charges and costs are available. The cost of the implant is included in “Supplies (medical and operative).” The operating room cost includes staff and administrative expenses based on half-hourly charges for operating room use. In 2008, the charge for operating room usage was $775.00/half-hour. The recovery room cost includes staff and administrative expenses based on charges of $220/half-hour for the first half-hour and then $80.00 for each subsequent half-hour. The reason why the first half-hour amount was larger is because more services (e.g., nursing) need to be devoted to a patient in the immediate postoperative period. The hospital room service center charge was based on the average cost of room and board during a patient stay, which was $890 in 2008.11 In calculating hospital expenses, anesthesiology costs do not include professional services.
Table 134-3 Service Centers for Primary Total Knee Arthroplasty at the Lahey Clinic in 2008
| Service Center | 2008 Dollars |
|---|---|
| Anesthesiology | 874.19 |
| Blood bank | 269.73 |
| Radiology | 56.18 |
| Vascular laboratory | 8.25 |
| Pathology | 0.00 |
| Intravenous therapy | 44.88 |
| Electrocardiography | 7.86 |
| Physical therapy | 345.43 |
| Operating room | 2094.56 |
| Orthopaedic appliances | 118.91 |
| Occupational therapy | 52.58 |
| Laboratory | 199.00 |
| Recovery room | 889.34 |
| Hospital room | 3257.29 |
| Supplies (medical and operative) | 2554.65 |
| Pharmacy | 103.78 |
| Respiratory therapy | 14.26 |
| Other | 18.94 |
| Total hospital cost | $10,909.83 |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree