27
Dupuytren’s Contracture
Jack Abboudi and David S. Zelouf
History and Clinical Presentation
A 51 year-old right hand dominant construction supervisor presented with a 2- to 3-year history of a progressive right ring finger contracture. He denies a history of trauma. He is of Scottish descent, and his father has undergone bilateral Dupuytren’s contracture releases. The patient denies a history of diabetes or other medical illnesses, and he is taking no medications.
PEARLS
- The tabletop test is positive when the patient cannot place his or her open hand flap onto a table surface due to flexion contractures. This finding may prompt consideration for surgical treatment.
- Counsel patients with early disease as to your indications for operative treatment. This may help the patient seek revaluation at an appropriate point for surgery before severe contractures form.
- MP contracture correction tends to produce more satisfying results than PIP correction.
- Cleland’s ligaments, the deep transverse metacarpal ligament, and the flexor tendon sheath are not involved in the disease.
PITFALLS
- Procedures performed by “limited exposure” still require adequate visualization of the neurovascular structures that may be displaced from their normal location.
- Neurovascular structures may be displaced superficially and toward the midline of the digit by the spiral cord and should not be assumed to be in their anatomic position. Generally, tracing the neurovascular structures is easier in a proximal to distal direction starting just distal to the transverse carpal ligament.
- Neurovascular structures are displaced more toward the midline and more superficial with increasing PIP contracture.
Physical Examination
A prominent cord is noted in the palm in line with the ring finger extending to the level of the proximal interphalangeal (PIP) flexion crease. There was a prominent nodule present over the palmar aspect of the proximal phalanx, with a 60-degree metacarpophalangeal (MP) contracture and a 10-degree PIP contracture (Fig. 27–1). The left hand exhibited early palmar disease with no contracture. No knuckle pads were noted, and there was no involvement of the plantar surfaces of the feet.
Radiographic Findings
Plain x-rays of the right hand were unremarkable.
Differential Diagnosis
Dupuytren’s contracture
Joint flexion contracture
Scar contracture
Flexor tendon bowstring
Tendon adhesions
Tumor (i.e., fibrosarcoma)

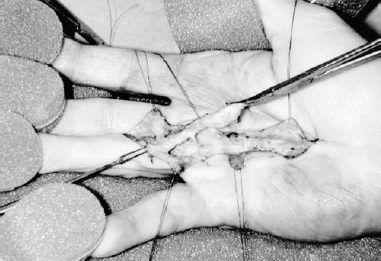
Figure 27–1. Preoperative clinical photo.
Diagnosis
Dupuytren’s Contracture
Dupuytren’s disease has been attributed to genetic lines of Viking heritage and northern European lineage with an autosomal-dominant pattern of inheritance. The condition presents most frequently in males and after the age of 40. Clinical features include painless palmar pitting, cords, and nodules frequently in line with the small and ring finger. Many structures, described as “ligaments” and “bands” in their normal state, are referred to as “cords” in the diseased state (Fig. 27–2). The spiral cord is a continuum of the diseased spiral band, lateral digital sheet, and Grayson’s ligament. The spiral cord is pulled to the midline with contracture, causing the neurovascular bundle to wrap around the straightening and tightening cord. The natatory cord can be palpated in the web space, and its contracture deviates the digit from the midline at the MP joint. See the suggested readings, later, for more comprehensive descriptions of the pathoanatomy. Disease progression generally leads to characteristic flexion deformities of the MP and the PIP joint. Associated findings include dorsal knuckle pads (Garrod’s nodules), thickening of plantar tissue in the foot (Lederhose’s disease), and penile fascia (Peyronie’s disease).
Indications for surgical correction of Dupuytren’s contracture depend greatly on the impact of the deformity on the patient’s ability to perform activities of daily living and the ability and willingness of the patient to participate in the postoperative rehabilitation. Hard-and-fast, objective surgical indications are difficult to define. The “tabletop test” provides the earliest sign of significant flexion contracture, although this test alone is not always an indication for surgery. The test is positive when the patient cannot fully flatten his or her hand against a table surface. Generally, flexion deformities of the MP joints are better tolerated by the patient and are relatively easier to correct, as MP flexion is a relatively “safe” position that maintains collateral ligament length. On the other hand, PIP deformities interfere more with hand function and are more difficult to correct, as PIP flexion is a relatively “unsafe”position that allows for volar plate contracture. Therefore, PIP flexion deformities are stronger indications for surgery at earlier stages than are MP deformities.
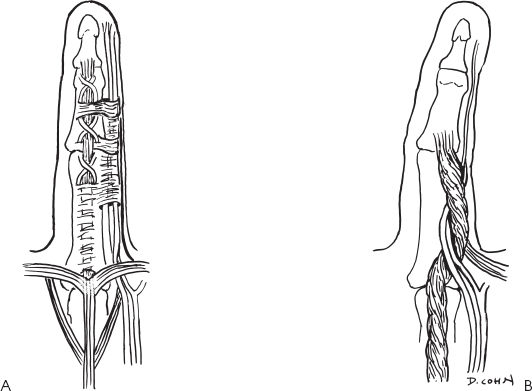
Figure 27–2. Anatomy of normal (A) and contractured (B) digits.
The myofibroblasts share cellular characteristics between fibroblasts and smooth muscle cells and are concentrated within the palmar nodules. The contractile elements of this cell type produce a progressive pull through the Dupuytren cords that leads to the characteristic flexion deformity. Residual myofibroblasts within the dermis and epidermis after surgical excision of diseased tissue have been implicated in the recurrence of the contracture. This notion is supported by the lower recurrence rate seen with palmar skin excision and full-thickness skin grafting after fasciectomy.
Surgical Management
The patient was treated with a subtotal palmar and digital fasciectomy. He was brought to the operating room where, under axillary anesthesia, Brunner incisions were utilized to expose the pretendinous cord (Fig. 27–3). An early spiral cord was encountered at the level of the PIP joint. After both neurovascular bundles were identified and protected, the involved palmar fascia was excised and sent to the pathology laboratory for gross and histologic analysis. At the conclusion of the procedure, complete correction was obtained at both the MP and PIP joints. The tourniquet was deflated prior to closure, and brisk capillary refill was noted immediately. The wounds were closed with interrupted 5–0 nylon sutures, and a short arm plaster splint was placed, immobilizing the MP joints in 30 degrees of flexion, with the PIP joints comfortably extended.