Chapter 75 Dupuytren Contracture
Ectopic Dupuytren disease deposits may occur in a variety of areas (Fig. 75-1). Approximately 5% of patients with Dupuytren contractures have similar lesions in the medial plantar fascia of one or both feet, known as Ledderhose disease, and 3% of patients have plastic penile induration, known as Peyronie disease. Garrod nodules, “knuckle pads” are common on the dorsum of the proximal interphalangeal joints. Patients with these associated findings are considered to have a Dupuytren diathesis and are prone to progressive and recurrent disease.
Commonly occurring in adults in their 40s to 60s, Dupuytren contracture occurs 10 times more frequently in men than in women. According to McFarlane, the disease occurs significantly earlier in men (33 to 63 years old) than in women (46 to 70 years old). It is most common in individuals of Scandinavian and Celtic origin, although it has been reported occasionally in blacks and rarely in Asians. The lesion has been reported to be more frequent and severe in individuals with diabetes mellitus or with epilepsy (42%), and conflicting reports exist concerning the disease in individuals with alcoholism. The involvement, although often bilateral (45%), rarely is symmetrical (Fig. 75-2). Mikkelsen et al. found that mortality may be increased in men who develop the disease before age 60.
Pathogenesis
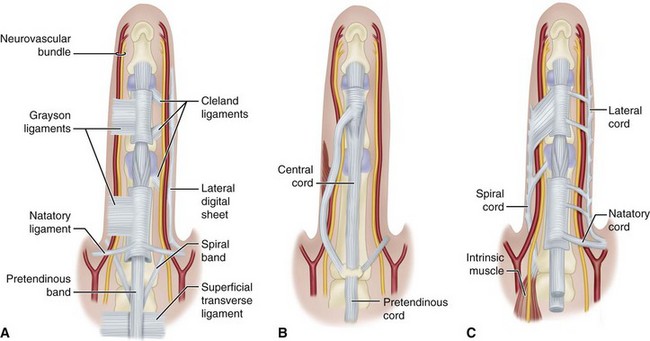
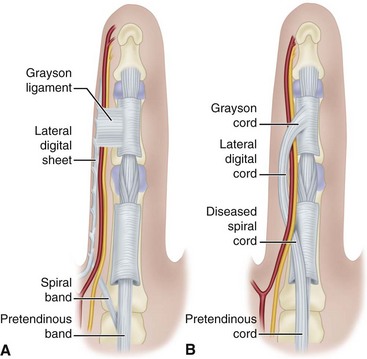
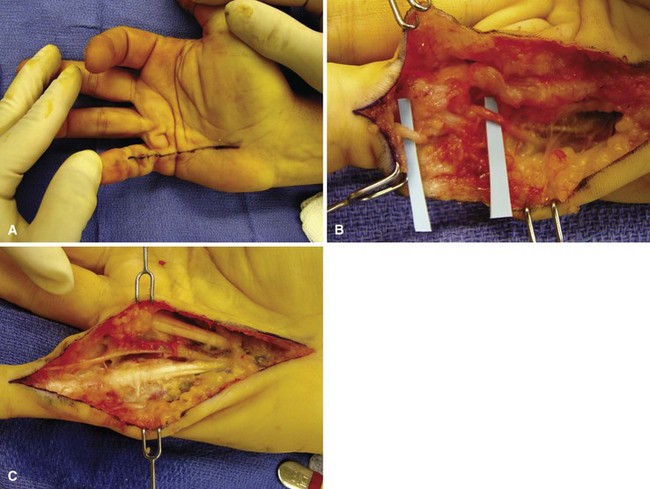
The fascial structures that may become involved in the fibroproliferative process have been clearly outlined by McFarlane (Fig. 75-3). Thomine described a longitudinally oriented fascia located dorsal to the neurovascular bundle, which he termed the retrovascular cord. This structure often is involved in the disease and may be implicated as a cause for recurrent proximal interphalangeal contractures. The Cleland ligament generally is believed to be spared. The pretendinous cord nearly always is responsible for primary contracture of the metacarpophalangeal joint. It may attach to the distal palmar crease skin, base of the proximal phalanx, or the tendon sheath at this level, or it may extend to attach to the flexor tendon sheath over the middle phalanx or the skin in this area. A spiral cord occurs when four normally existing structures (pretendinous band, spiral band, lateral digital sheet, and Grayson ligament) become diseased. The spiral cord runs dorsal to the neurovascular bundle proximally and volar to it distally. When the spiral cord is contracted, the neurovascular bundle is drawn toward the midline of the finger (Fig. 75-4). Neurovascular displacement is found most commonly on the ulnar aspect of the little and ring fingers, and tedious dissection is required to prevent digital nerve injury.
Metacarpophalangeal and distal interphalangeal joint contractures seem to result from pretendinous and lateral cord development. Proximal interphalangeal joint contractures may develop from isolated digital cords, however, in addition to central, spiral, or retrovascular cords (Fig. 75-5). The diseased tissue in this unusual form of Dupuytren contracture most commonly affects the small finger; however, any digit may be involved. The cord originates from the periosteum of the proximal phalanx and fascia overlying the intrinsic muscles and distally courses dorsal to the neurovascular bundles, inserting into the middle phalanx or the overlying flexor tendon sheath volar to the neurovascular bundles. This digital cord frequently displaces the neurovascular bundle superficially to the midline of the finger, similar to a spiral cord.
Prognosis
1. Heredity. A family history of the disease indicates that the lesion is likely to progress more rapidly than usual, especially if the onset is early.
2. Sex. The lesion usually begins later and progresses more slowly in women, who often accommodate better to the resulting deformity; however, long-term results after operation are worse in women than in men, with postoperative flare reaction being twice as likely.
3. Epilepsy. Despite earlier statements positively associating Dupuytren contracture with epilepsy, Geoghegan et al. concluded that neither epilepsy nor antiepileptic medications were associated with the disease.
4. Diabetes mellitus. Diabetes mellitus is a risk factor for Dupuytren disease, especially in patients requiring medical management compared with patients with diet-controlled diabetes mellitus. According to Geoghegan et al., patients taking insulin were more likely to have Dupuytren disease than patients taking metformin or sulfonylureas.
5. Alcoholism or smoking. The lesions are more severe, progress more rapidly, and recur more frequently when associated with these conditions. Godtfredsen et al. found a dose-dependent relationship to alcohol intake and smoking and concluded that the combination of these two factors conveys a high risk for the development of Dupuytren disease.
6. Location and extent of disease. When the disease is bilateral and especially when it is associated with knuckle pads and nodules in the plantar fascia, progression is more rapid, and recurrence is more frequent. Progression is more rapid on the ulnar side of the hand.
7. Behavior of disease. How the disease has behaved in the past, whether treated or not, is an indication of its probable behavior in the future.