47
Dorsal Dislocations of the Proximal Interphalangeal Joint
Rosa L. Dell’Oca and Amy Ladd
History and Clinical Presentation
A 40-year-old right hand dominant mechanic presented with a painfully swollen incongruent proximal interphalangeal (PIP) joint of his right index finger after a tire exploded while he was increasing the air pressure. Closed reduction, although successful, resulted in an unstable joint.
Physical Examination
The PIP joint demonstrated 15 degrees of ulnar deviation with considerable edema and a volar laceration. Tenderness was elicited over the volar and radial aspects of the joint. Pain limited full active flexion, and the middle phalanx subluxed dorsally at 10 degrees of active extension.
Diagnostic Imaging
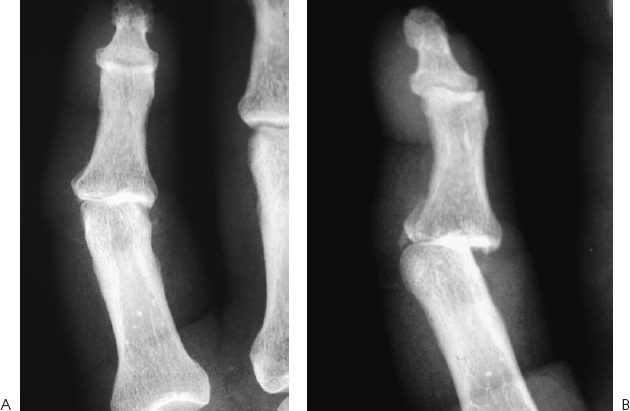
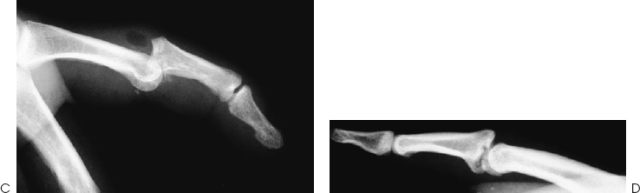
Anteroposterior, lateral, and oblique radiographs of the involved digit were obtained (Fig. 47–1).
Differential Diagnosis
Dorsal dislocation of the PIP joint
Lateral dislocation of the PIP joint
Volar dislocation of the PIP joint
Fracture of the distal proximal phalanx
Fracture of the proximal middle phalanx
Sprain of the PIP joint
Lateral dislocation: greater than 20 degrees of angulation with ulnar/radial stress of the PIP joint; radial or ulnar joint tenderness with or without volar plate tenderness; anteroposterior (AP) radiograph may demonstrate lateral displacement.
Volar/lateral dislocation: lateral radiograph exhibits middle and distal phalanges at an oblique angle as compared with the proximal phalanx.
Volar dislocation: tenderness of the dorsal aspect of the base middle phalanx; lateral radiograph reveals a fracture of the dorsal aspect of the base of the middle phalanx.
Fractures: AP, lateral, and oblique (condyles) radiographs may display fractures of the head of the proximal phalanx or the base of the middle phalanx.
Diagnosis
PEARLS
- Obtaining perfect lateral radiographs to detect the subtlest incongruity
- Obtaining prompt attention by hand specialist, or knowledgeable practitioner and to not ignore this common injury
PITFALL
- Disregarding the injury as a simple sprain without adequate physical and radiographic examination
Dorsal Proximal Interphalangeal Joint Dislocation
Dorsal PIP dislocations are probably common but underreported, because many high-paid athletes play with fresh injuries set in the field, or present with old untreated injuries that may be painful, unstable, or fused. Estimated at 9/100,000/year, the incidence of dorsal PIP fracture dislocations is much higher.
History, physical examination, and radiographs reveal the diagnosis and prognosis, and facilitate treatment. History divulges the mechanism of injury and suggests the final configuration of the joint despite memory lapse or spontaneous or deliberate reduction. The joint may assume the characteristic bayonet configuration or an obvious posture of hyperextension but occasionally subtle subluxation requires radiographic elucidation. Palpation delineates the injured structures and active range of motion may reveal instability with progressive extension. Although pain and edema typically limit flexion, a torn volar plate interposed within the joint must be considered. If radiographic evaluation displays joint congruity, then subtle instability may be elucidated by passive range of motion facilitated by a digital block.
A simple sprain, recognized by a moderate amount of tenderness over the bruised but stable joint with a normal radiograph represents a partially torn ligament.
Despite the check rein ligaments, proximal detachment of the volar plate occurs experimentally with slow hyperextensile forces. Conversely, longitudinal accelerated hyperextensile forces cause distal rupture of the transversely oriented fibrocartilaginous fibers of the volar plate. This injury alone allows greater than the normal 10 degrees of hyperextension. Typically, in these hyperextension injuries there is no history of abnormal joint position, no evidence of instability on active and passive range of motion, and no articular incongruity or fracture on radiographs. Even with an incomplete longitudinal split in the collateral ligament, the remaining intact accessory collateral ligament imparts some stability.
Higher energy forces produce tears between the thin accessory collateral ligament and the thick primary collateral ligament in addition to volar plate disruptions. Experiments suggest that partial volar plate tears represent areas of potential weakness at risk of rupture with repeated stress. Typically, these injuries present with a history of joint misalignment and radiographs may demonstrate a small volar fragment.
Part of the weak volar central trabecular base of the middle phalanx may remain attached to the volar plate, otherwise known as an avulsion injury. Larger volar fragments typically result from greater longitudinal rather than hyperextensile forces, where the proximal phalanx shears off the volar base of the middle phalanx. Smaller volar fragments (<30–50%) retain support from the remaining accessory collateral ligaments and a portion of the primary collateral ligament (Eaton and Dray’s “stable dislocations”), whereas larger fragments portend relying solely on the extensor tendon and dorsal capsule for stability in flexion and have no support in extension, which explains the propensity to redislocate after reduction (Eaton and Dray’s “unstable dislocations”). A direct correlation exists between the percent of volar middle phalanx surface fractured and the likelihood of dorsal subluxation/dislocation. Maximum contact between the articular surfaces of this ginglymus joint, and the action of the flexor and extensor tendons pulling axially through a column consisting of the middle phalangeal base, resting on the proximal phalangeal condyles stabilized by the interdigitation of the intercondylar sulcus and eminence, resist dislocation even in the face of collateral ligament and volar plate disruption. With intraarticular fractures, the residual middle phalangeal dorsal articular surface and shaft form an inclined plane that tends to slide dorsally and proximally as the extensor and flexor tendons pull the distal portion of the middle phalanx volarly and the proximal end of the middle phalanx dorsally, creating a zigzag posture. Furthermore, the slightly different radii of curvature of the condyles allow some rotation despite the inherent lateral stability, which explains disproportionate injury to radial versus ulnar collateral ligaments.
Classification systems with varying emphasis on the degree of ligamentous integrity, the percentage of articular involvement, or the degree of subluxation exist to facilitate the correct treatment. The history of injury, the point and degree of instability, and radiographic evaluation are adequate determinants in our opinion.
Treatment
The injured athlete often reduces the dislocated finger. If not, usually gentle traction will suffice to reduce the subluxated PIP joint. Reduction of a true dislocation requires reproduction of the original angle of injury to realign the joint surfaces and traction on the middle phalanx with volarly directed pressure at its base. Regional blocks, muscle relaxants, finger-trap traction and arm-loaded countertraction facilitate the difficult reductions, unless there is a hindering soft tissue entrapment. The ease of reduction is proportional to the quantity of intact ligament and inversely proportional to the size of the fragment. Fragments greater than 40% of the base herald instability. Joint congruity takes precedence over anatomic reduction of the fracture, for the subtlest incongruities may lead to chronic pain, degenerative changes, and ankylosis. The goal is stable, smooth, and pain-free range of motion of the affected joint. This may be surprisingly difficult to attain.
Nonoperative Management
After reduction or placement of the PIP joint at an acceptable angle without evidence of subluxation, a period of rest is followed by protected active range of motion. For simple sprains, 1 to 3 weeks of splinting followed by a protected return to normal activities within a few weeks with buddy taping, suffices.
An extension block splinting (EBS) regimen succeeds for hyperextension injuries, yet some might buddy tape for 3 weeks or implement dorsal splinting for 7 to 14 days with an additional 2 weeks for residual volar instability followed by active and passive range of motion. Similar injuries, with radiographic evidence of minor subluxation that achieves congruity with manipulation fall into the same category but require hypervigilance with weekly radiographic confirmation of joint congruity for several weeks, followed by active and passive range of motion in a splint worn for an additional 1 to 2 weeks.
A known dislocation, demonstrating instability at less than 30 degrees of flexion with or without a nondisplaced intraarticular fracture involving less than 50% of the volar lip, may be treated successfully by closed reduction and EBS for 3 weeks, with active range of motion commencing at 7 days followed by 3 weeks of buddy taping.
Operative Intervention
Dislocations involving large volar fractures or those irreducible, unstable, or incongruous joints, regardless of fracture size, require operative intervention. In large disruptions of the middle phalanx volar surface, without the stabilizing collateral ligaments, the proximal phalangeal condyles sink into the volar plate and the distal inserting flexor digitorum superficialis (FDS) and flexor digitorum profundus (FDP) bend the middle phalanx rather than produce gliding palmar rotation of the articular base. The joint fails to remain congruent and parallel with the proximal phalangeal head through flexion. As a result, the joint hinges or angles. For these tenuous fractures, a transarticular Kirschner wire (K wire) may be placed through the PIP joint flexed at 40 degrees or more to diminish the subtle fracture articular site incongruities associated with eventual failure and EBS initiated after K-wire removal at 3 weeks. Failure of closed reduction leaves open intervention or constant traction as subsequent options. Open reduction with internal fixation and EBS mobilization at 3 weeks have been successful for tenuous fractures using such means as a single K wire with or without a tension band, an interfragmentary screw or an interosseous wire with the well-known complications of malunion, pin tract infection, tenodesis, and posttraumatic arthritis. Other treatments include osteotomy with bone grafting, volar plate arthroplasty, secondary PIP arthroplasty, and arthrodesis.
For fracture-dislocations involving greater than 70% of the volar lip, neither advancing the volar plate nor neocollateralization will successfully maintain reduction. Only reconstruction of a competent volar buttress restraint will prevent redislocation. Yet attempts at realigning the large volar fragment by osteotomy and bone grafting usually fail, requiring PIP joint salvage through replacement arthroplasty or arthrodesis. In fact, regardless of the intervention(s), many ultimately end up with a pain-free ankylosis or require silicone arthroplasty.
For comminuted, impacted, and some irreducible fractures, treatment includes volar plate arthroplasty, dynamic force coupling devices, and transarticular K-wire placement. Secondary options include custom external fixation or placement of an interosseous wire through the volar plate to reduce the subluxed middle phalanx and mobilization with EBS. Typically the comminuted fragments are too small for fixation and are debrided.
In compound (open) dislocations involving a volar transverse tear in the skin with occasional protrusion of the head of proximal phalanx through skin and/or flexor tendon involvement, Stern and Lee found that the joint could not be stably reduced if the volar plate was not repaired distally, whereas Green and Posner found that it was not necessary with proximal tears.
Acutely treated injuries enjoy better outcomes than those that present late, that is, greater than 4 weeks after the injury. Injuries limited to volar plate avulsion with flexion deformity less than 30 degrees allow late primary repair, which may decrease the chance of severe flexion contractures.
For a subacute, greater than 10 days postincident, volar plate injury with collateral ligament injuries and persistent subluxation, restoration of range of motion may require excision of the contracted and normal primary and accessory collateral ligaments and dorsal capsule with immediate active range of motion, for excision of only the contracted ligaments will not restore full range of motion. Sparing part of the accessory collateral ligaments affords some stability.
Delayed treatment of large fractures requires release of the collateral ligaments to allow fragment reduction and possibly additional volar plate arthroplasty for comminuted fragments. Osteotomy of the proximal middle phalanx may provide an additional 40 degrees range of motion as the volar lip of the middle phalanx tilts to embrace the volar proximal phalanx.
For severe articular damage, failed reconstruction, persistent deformity, and pain, salvage procedures may be necessary. Arthrodesis in the radial digits to stabilize pinch, and replacement arthroplasty for the little and ring fingers to allow power grasp, may provide significant improvement in function and appearance.
Extension Block Splinting
Based on early range of motion within a stable arc, this straightforward, easily instituted and monitored method requires readily available and inexpensive materials and enjoys great success for stably reduced dislocations or as a means of protected range of motion after an open procedure. Although indicated for stable fractures of less than 10 to 15% involvement of the volar base, fractures constituting <40% of the base are still considered in the ideal group, and success has been found with some fractures as great as 70%. Once adequately reduced, a digital, hand, or forearm-based splint ensures that the digit remains well opposed to the splint and maintains flexion of the PIP joint blocked at 10 to 20 degrees greater than the point of demonstrable instability. Although McElfresh et al allowed up to 60 degrees of flexion to obtain stability, most accept a maximum of 30 degrees. This guideline prevents the chance of irreversible flexion contracture and delegates cases requiring greater than 30 degrees to other treatments. Lateral radiographs within the splint confirm this optimal point of flexion where the articular surfaces are absolutely congruent, for the PIP joint may become incongruous slowly, gradually, and subtly with extension. Some embark on immediate active range of motion, whereas others allow 1 week of rest. After 1 week of mobilization and radiographic and clinical confirmation of sustained congruity at rest and in maximum flexion, the degree of flexion is reduced by one third and the joint reassessed by a lateral radiograph. If radiographs demonstrate incongruity, extension is increased by only one half of the potential extension. After the usual interval to full extension (6–8 weeks), the splint is removed and grip and massage exercises are started, but pinch to the involved finger and stretching of the involved joint is avoided until grip strength is 50%. Full rehabilitation is complete by the third month postinjury.
Open Reduction and Internal Fixation
Eaton and Malerich describe an elegant volar radial, rather than dorsal, approach to preserve the skin flaps should open reduction prove futile and be abandoned for a volar plate arthroplasty. After excising the sheath between the A2 and A4 pulleys, the volar plate is detached distally from the middle phalangeal fragments and laterally from the accessory collateral ligaments to open and shotgun the floor of the joint. Drilling a hole distal to the fracture allows introduction of a probe to elevate and reduce the fragments. Whichever method of fixation is used, the hardware should exit close to the central slip insertion without tenting the dorsal skin or penetrating the lateral bands or retinacular structures. Once the fracture is stabilized, extension block splinting may be instituted as above.
Volar Plate Arthroplasty (VPA)
Introduced by Eaton in 1967, VPA finds application in the following: acute fracture-dislocations displaying volar proximal middle phalangeal fractures of greater than 60% or those with excessive comminution and/or impaction; and chronic fracture-subluxation of the PIP, where there are degenerative changes or joint stiffness.
Utilizing the volar radial approach described above, the crucial step relies on creating a symmetric trough in the volar base of the middle phalanx to allow the volar plate to slip easily into the defect. Asymmetry usually prevents successful fracture reduction. Introducing a pullout wire Kessler style allows the ends to exit the distal corners of the volar plate and secure it to the radial and ulnar aspects of the middle phalanx through holes drilled laterally into the trough. The author (A.L.) employs tissue anchors, an updated version of this technique. Securing the wires to produce no more than 30 degrees of flexion reduces and stabilizes the joint, fills the volar defect, and decreases lateral angular deviation. By flexing the PIP and DIP joints while passing the pullout sutures dorsally, the lateral bands subluxate volarly, avoid entrapment, and thus lessen DIP stiffness. Embedded fragments of bone or cartilage can be left in place. A transarticular K wire is placed for joint stability and for very large disruptions (50–80%); an external fixator may be required for ∼1 to 2 weeks. After K-wire removal at 2 weeks, EBS commences and the pullout wire is removed 1 week later, with unrestricted extension beginning at 4 weeks.
Aside from acutely reducing the dislocated joint, VPA maintains congruous PIP joint reduction by providing a volar restraint, resurfaces the damaged articular surface of the middle phalanx with compatible vascularized material, fibrocartilage, and may be responsible for later joint remodeling and continuously improving range of motion even years later.
Dynamic Force Coupling
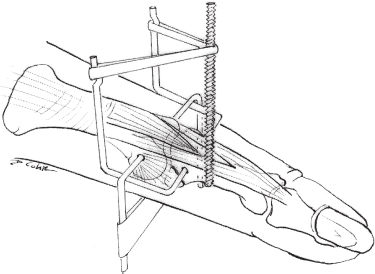
Robertson et al corrected the zigzag deformity by placing K wires to apply traction dorsally on the distal proximal phalanx and volarly on the proximal middle phalanx to realign the joint and axially on the distal middle phalanx to counteract flexor and extensor pull. Beasley used a static, bulky device incorporating distal traction with a volar splint to push the distal proximal phalanx dorsally. By decreasing the size of the device and allowing movement during traction, Agee enjoyed better results compared with Robertson et al and equaled those of McElfresh et al for acute fracture-dislocations and chronic fracture-dislocations.
Implementation requires an adequate stable dorsal shelf of proximal middle phalangeal bone and careful K-wire placement (Fig. 47–2). The K wire placed transversely in the proximal middle phalanx must be a safe distance away from the fracture and volar to the lateral bands. The K wire oriented perpendicular to the middle phalanx should not be driven too far distally through the lateral bands, preventing motion of the distal phalanx, or too deeply through the profundus tendon. Lastly, the transverse K wire through the proximal phalanx must be exactly through the axis of rotation to prevent hyperextension and possible swan neck deformity. Often subacute unstable cases greater than 10 days postinjury cannot be reduced in a closed fashion, and require release of the malpositioned collateral ligaments.