65
Dorsal Capsulodesis for Midcarpal Instability
William K. Feinstein and David M. Lichtman
History and Clinical Presentation
A 24-year-old right hand dominant man sustained a dorsiflexion injury to his right wrist while trying to protect himself from a falling shelf at work. He continued to work with pain for about 6 weeks before he presented to an orthopedic surgeon. He was treated nonoperatively for a year and a half, but he continued to complain of ulnar-sided wrist pain and clunking. He had a positive midcarpal clunk with ulnar deviation, but his midcarpal instability was not as dramatic as his symptoms of ulnar abutment. Radiographs demonstrated ulna positive variance and mild VISI deformity. A triple-phase arthrogram revealed tears of the TFCC and lunotriquetral ligament. The patient was thus given a diagnosis of ulnar abutment syndrome. After failing conservative treatment (nonsteroidal antiinflammatory drugs, steroid injections, splinting), he was taken to the operating room for arthroscopic debridement of the torn TFCC and lunotriquetral ligaments, and open wafer excision of the right distal ulna. He did well postoperatively and progressed with occupational therapy that included range-of-motion exercises, stretching, and later wrist strengthening exercises. However, the clunking sensation remained. At 1 year postoperatively, he had minimal complaints of ulnar abutment; however, the clunking sensation persisted and was associated with pain while gripping in palmar flexion. A pisiform loading volar splint was fabricated and was worn for all activities; however, his symptoms did not improve over the next 2 months.
PEARLS
- Stability of the DRUJ is essential.
- Begin forearm rotation as soon as possible. At minimum, support forearm in supination.
- Carefully analyze degree of comminution.
- Do not expose tendons or nerves to uneven fixation.
PITFALLS
- Unrecognized subluxation of the DRUJ
- Pronation “contracture”
- Failure of fixation secondary to comminution
- Reflex sympathetic dystrophy tendon rupture
Physical Examination
Dorsiflexion to 75 degrees, palmar flexion 75 degrees, pronation 50 degrees, and supination 70 degrees were noted. There was decreased grip strength by Jaymar grip testing, and there was a palpable clunk with ulnar deviation of the wrist (midcarpal shift test). This clunk was associated with apprehension and pain.
Diagnostic Studies
Radiographs of the wrist showed no scapholunate or lunotriquetral dissociation. There was mild VISI deformity.
Differential Diagnosis
Triquetrolunate instability
Triangular fibrocartilage complex tear
Subluxation of the distal radioulnar joint
Extensor carpi ulnaris tendon subluxation
Diagnosis
Midcarpal Instability
This patient was initially treated for ulnar abutment syndrome with TFCC tear and triquetrolunate tear. These disorders create symptoms, which overlap with midcarpal instability. Although the symptoms improved following ulnar shortening, the midcarpal instability clunk continued. Distal radioulnar joint and extensor carpi ulnaris tendon subluxation were ruled out by physical exam. Although a VISI deformity is characteristic of midcarpal instability, this is not an absolute requirement for the diagnosis.
Midcarpal instability is due to congenital laxity, gradual attenuation, or acute disruption of the volar arcuate, and/or dorsal radiotriquetral ligaments. Each of these components couples the distal row of carpal bones to the proximal row, ensuring normal joint contact. In normal wrists with normal midcarpal geometric alignment, bone and ligament contact forces cause the proximal row to move from flexion (VISI) to extension [dorsal intercalated segment instability (DISI)] as the wrist moves from radial to ulnar deviation. With midcarpal instability, the proximal row rests in volar flexion due to ligament laxity, and the distal row is translated volarly. When the wrist moves from neutral into advanced ulnar deviation, the joint geometry, bony restraints, and axial compression on the ulnar side cause the proximal row to suddenly rotate back into physiologic dorsiflexion, and the distal row snaps back into dorsal translation. This produces what has been referred to as the “catch-up clunk,” causing pain in patients with midcarpal instability.
Patients usually present with painful “clunking” on the ulnar side of the wrist during activities, which require active ulnar deviation of the wrist with the forearm in pronation. A history of repetitive loading of the wrist by vocational tasks or avocational interests is common, and symptoms of pain and clunking tend to occur with these repetitive activities. There may or may not be a history of trauma.
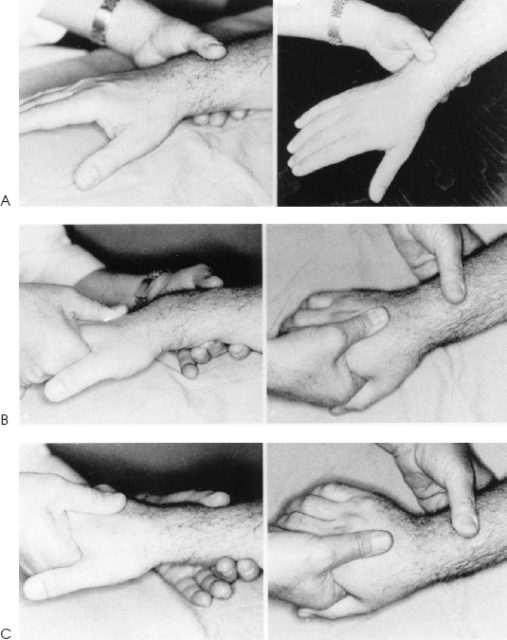
On physical examination, there is often a palmar sag on the ulnar side of the wrist, with a prominent appearing ulnar head, although sometimes swelling or localized synovitis will be present, making the ulnar sag and prominent ulnar head less dramatic. There usually is tenderness over the ulnar carpus in the region of the triquetrohamate joint. Usually the patient can spontaneously reproduce the “clunk” with active ulnar deviation of the pronated wrist. The clunk occurs at the extreme of ulnar deviation, and it is most often visible, audible, and palpable to the examiner. After the clunk occurs, the volar sag disappears. Another reverse clunk can sometimes be appreciated when the wrist moves back into neutral. In this case, the volar sag reappears. The midcarpal shift test is an important diagnostic tool for identifying the patient with midcarpal instability, especially patients who cannot spontaneously cause the clunk to occur in the office (Fig. 65-1).
A lateral radiograph of the wrist in neutral deviation will usually demonstrate a VISI deformity with slight volar translation of the distal carpal row. Cineroentgenograms in the posteroanterior and lateral planes are diagnostic. Wrist flexion and extension is normal; however, as the patient actively moves his wrist from radial to ulnar deviation, one can see the entire proximal row snap suddenly from a flexion or VISI position into an extension or DISI position when the wrist reaches a critical point of extreme ulnar deviation.