Chapter 62 Distal Realignment of the Patellofemoral Joint
Indications, Effects, Results, and Recommendations
Effective surgical treatment of patellofemoral pain and/or instability depends on an accurate diagnosis, understanding of the pathophysiology of the condition, and knowledge of the effects of a given surgical treatment on the mechanics and biology of patellofemoral function. Anterior knee pain, often caused by a patellofemoral disorder, is a common disabling complaint in young adults, predominantly women. Fortunately, nonoperative treatment, including quadriceps strengthening, stretching, core stability training, McConnell taping, and bracing, is usually effective.* However, when conservative treatment fails, and a specific treatable cause of anterior knee pain can be identified after careful physical, radiographic, and, in some cases, arthroscopic examination, successful surgical treatment of patellofemoral disorders is likely. Likewise, in the event of recurrent patellar instability, when anatomic variables are correctly defined, a logical choice can be made for successful treatment. The purpose of this chapter is to define the situations in which tibial tubercle transfer is indicated for anterior knee pain and/or patellar instability and to present appropriate techniques for safe and reproducible treatment.
Pathophysiology of Patellofemoral Pain and Instability: Implications for Treatment
Patients with patellofemoral pain problems typically have various degrees of articular pain, soft tissue pain from overuse or chronic stretch, and mechanical instability from malalignment or dysplasia of the joint. Quadriceps weakness almost always accompanies anterior knee pain and may be a cause and/or result of knee pain. Restoration of quadriceps strength and flexibility is critical to improving load acceptance. A primary function of the quadriceps is to absorb energy during gait.106 If the quadriceps is relatively weak and stiff, it can neither generate the desired force concentrically nor absorb the necessary energy eccentrically. In knees with a deficiency of muscular energy absorption as a result of eccentric quadriceps weakness, this energy must be absorbed elsewhere in the extensor mechanism, which may result in painful overload of patellar subchondral bone or excessive stretch of peripatellar soft tissues. Should the peripatellar soft tissues be less compliant and flexible than normal, such loads may be poorly tolerated. When the problem is viewed as a deficiency in energy absorption, one can imagine that nonoperative management must focus on improving strength and flexibility throughout the lower extremities. The rehabilitation regimen must not overload the system. The concept of staying within the “envelope of function” during patellofemoral rehabilitation is especially critical to success.27 Rehabilitation efforts that attempt to increase strength and function by working the knee as hard as possible are destined to fail in patients with patellofemoral disorders. The prime example is the effect of isokinetic exercise on patients with anterior knee pain. Because isokinetic equipment is designed to produce resistance proportional to the force applied, the joint is forced to work at its upper limits. Already overloaded tissue tolerates this situation poorly. Instead, flexibility, strengthening, judicious use of anti-inflammatory medication, and patience should be emphasized to allow overloaded tissues to heal.
Not every anterior knee pain patient with objective radiographic patellofemoral malalignment with or without arthrosis will need surgery. Only if a dedicated effort at nonoperative management of these patients fails and if malalignment is objectively present, surgery to realign the extensor mechanism and/or decrease patellofemoral joint reaction force may be appropriate. Although our discussion is limited to patellofemoral problems, it is important to remember that anterior knee pain does not necessarily come from patellofemoral disease. Other causes of pain to be considered before surgery on the patellofemoral joint itself is planned include symptomatic chondromalacia patellae, patellofemoral arthrosis, plica or fat pad syndrome, iliotibial band friction syndrome, vastus lateralis tendinitis, quadriceps or patellar tendinitis, retinacular strain,42,94 referred pain, and chronic effusion from mechanical (meniscal and/or instability) or inflammatory problems. In addition, one must remember to examine the patient for posterior cruciate ligament deficiency, a condition sometimes associated with anterior knee pain.61 Anterior cruciate ligament (ACL) deficiency has been reported to produce anterior knee pain in 20% to 27% of patients with chronic tears.9,14 ACL reconstruction, particularly that performed with the use of a bone–patellar tendon–bone autograft, is well known to activate anterior knee pain in some cases.
Postoperative neuromas or reflex sympathetic dystrophy may further complicate the initial diagnosis. Referred, neoplastic, and nonorganic causes of knee pain must also be excluded.66 Most diagnoses can be made on the basis of the history and physical examination and require only confirmation by radiographic and arthroscopic examination. Patients with patellofemoral problems, including recurrent dislocation, malalignment causing subluxation and/or tilt, osteoarthrosis, traumatic chondromalacia, and postpatellectomy pain, at times are candidates for surgery. It is imperative for the clinician to understand the pathophysiology of each diagnosis and whether the goal of surgery should be realignment, soft tissue débridement, and/or relief of pressure.
A rational approach to patellofemoral disorders requires the understanding that various problems are evidenced by different combinations of articular pain, soft tissue pain, and lateral instability of the joint. The search for the correct diagnosis therefore will require a search for the cause of the pain and/or instability. Of course, painful stimuli can originate only from tissues that contain pain receptors. Anatomic sources of pain in the patellofemoral joint include retinacular tissue, synovium, and subchondral bone (articular cartilage is devoid of nerve tissue).28,87 In knees with patellofemoral degenerative disease, afferent pain-transmitting substance P–containing fibers were isolated in the retinaculum, fat pad, periosteum, and subchondral plate of the patella, thus suggesting that anterior knee pain may have multiple origins.107 Conversely, a deficiency of such fibers has been seen in the case of congenital insensitivity to pain.25
Observation
Examine the patient while standing and ambulating for evidence of an increased Q angle, torsional deformities of the femur or tibia, knee varus/valgus, pronation of the hindfoot, leg length discrepancy, ankle deformity, scars, and other factors that may affect patellar alignment. Have the patient perform a single-leg knee bend as you watch from the front to see whether the knee rolls inward, thus suggesting weakness of external rotation at the hip. Quadriceps atrophy should also be noted, although we believe that apparent “isolated” VMO atrophy is not a true finding but rather is the superficial reflection of generalized quadriceps atrophy, as suggested by Lieb and Perry.67,68
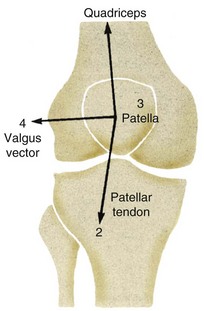
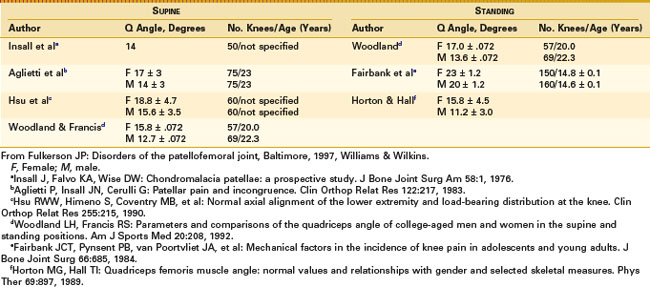
The Q angle is classically measured in extension from the anterior superior iliac spine to the midpoint of the patella and onward to the tibial tuberosity (Fig. 62-1). An increased Q angle should be considered to potentially increase the lateral vector of quadriceps force, possibly causing at least a theoretical tendency toward lateral patellar translation (subluxation). Although the Q angle has always been part of the traditional evaluation of the patellofemoral joint, careful review of the available literature reveals that Q angle measurements have not been well standardized. Measurements of the Q angle have been made while the patient is supine and standing. We favor the standing measurement because it includes physiologic loading. Unfortunately, the Q angle also has not been proved to correlate with the incidence of pain or the results of treatment.85 Normal populations have been measured, and the results are summarized in Table 62-1. Although the importance of understanding the lateral extensor moment and its potential effects on patellar alignment is undeniable, the role of Q angle measurement is less clear.
At 90 degrees of flexion, the tuberosity is normally directly inferior to the patella. Lateral deviation of the tubercle can be measured in this position and recorded as the tubercle-sulcus angle.62 Observation of these relationships allows the clinician to estimate the degree of valgus in the knee, as well as the position of the tibial tuberosity, which may be laterally displaced out of proportion to the tibiofemoral valgus. Lateral displacement of the tibial tubercle is more common in patients with patellofemoral pain and arthrosis and can be detected by physical examination and documented with computed tomography (CT).78 The Q angle, as measured clinically, does not directly correlate with patellofemoral pain, and although it is related to patellofemoral mechanics, it is only one of the many factors that influence patellar balance. However, once nonoperative management maximizes dynamic factors, static alignment, including tubercle position relative to the trochlear groove, should be considered. Patellar tracking must be considered as well. Normally, the patella lies superior and lateral to the trochlea on the supratrochlear fat pad in full extension. One may recognize patella alta on examination by the abnormally proximal position of the patella, but it is more accurately diagnosed radiographically. The patella enters the trochlea smoothly from its superolateral position at 10 degrees of flexion and, with increasing flexion, is centered and drawn into the trochlea. If during early flexion the patella tracks laterally and then suddenly shifts medially into the trochlea with active or passive flexion, the J sign is positive. In a review of 210 asymptomatic adults, Johnson et al59 found no subject with a positive J sign. Also, it should be kept in mind that the reverse J sign, in which the patella of a patient with medial patella subluxation slides in a medial-to-lateral direction on knee flexion, is clearly an abnormal pattern, but often is very subtle. As with all tests of alignment, comparison with the other side is important.
Provocative Tests
Strong compression of the patella resulting in pain and crepitus during flexion and extension of the knee is helpful in determining whether the patient’s pain syndrome has a significant patellofemoral component. Another method of provocative testing is isometric contraction of the quadriceps at different angles of flexion.73 Isometric contractions, which should be sustained for 10 seconds, provide the advantage of avoiding direct palpation in patients who are particularly apprehensive. If one or both of these methods reproduce the patient’s complaint, it is likely that the pain has a patellofemoral origin. These techniques of examination do not, however, distinguish between soft tissue and articular sources of pain because soft tissue stretch, as well as articular compression, is noted when the knee is moved or the quadriceps is fired during these examinations.
In an attempt to confirm whether a patient has medial patella subluxation, hold the patella slightly medial with one finger and the knee in extension, then abruptly flex the knee. If this maneuver reproduces the symptoms, the patient probably has a problem with medial subluxation, most commonly in the clinical setting of previous lateral release.35
Palpation
The subcutaneous position of the patellofemoral joint makes it uniquely available to careful examination. Palpation of the patellofemoral joint has two goals: (1) to differentiate between soft tissue and bony pain, and (2) to precisely localize the soft tissue or articular area that reproduces the patient’s complaint. Firm compression of the patella directly into the trochlea while the knee is held in various angles of flexion, combined with the knowledge that articulation starts distal on the patella and moves proximally with increasing flexion, can provide information to localize the articular disease. This can be accomplished by direct compression (with care taken to avoid compressing adjacent soft tissue structures). Meaningful specific palpation of medial or lateral patellar facets seems anatomically unlikely, given the interposition of innervated synovium and retinacular tissue. The degree of crepitus is more significant when absent or asymmetrical with the contralateral knee. When evaluating the presence or absence of crepitus, remember that Johnson et al found 94% of asymptomatic women to have crepitus.59 It is more important to note whether articular compression reproduces the patient’s pain. Also, knowledge of the character of the crepitus is helpful. Harsh, sustained grinding is different from the faint click that is common on flexion and extension of a normal knee.
Soft tissue palpation should systematically include the retinacular structures, the insertions of the quadriceps tendons into the superior pole of the patella, and the patellar tendon. Structures are generally best palpated in a position that places them on stretch and allows gentle palpation to achieve relative isolation from the underlying structures. This strategy allows discovery of specific points prone to overuse-type injury. We have previously described in detail a thorough anatomically and functionally oriented soft tissue examination, and the reader is encouraged to practice and master these techniques.37,38,85 Points of intersection between structures, such as the junction of the medial patellar tendon, the inferior pole of the patella, and the medial retinaculum, seem particularly prone to tenderness, perhaps because of the stress concentration at locations where two or more different structures under load meet. These locations are frequently tender in patients with excessive lateral patellar tilt. A cautious search for such locations will often uncover the origin of a patient’s soft tissue pain.
Stability Testing
The passive patellar tilt test is performed with the knee in full extension. While the patella is held in the center of the trochlea, the examiner attempts to correct the patellar tilt to neutral or beyond, if possible (Fig. 62-2). We agree with Kolowich et al62 that normally the tilt should correct at least to neutral, although normal patellae often tilt up to 10 degrees or more past neutral. It is also possible to gain an impression of the nature of the resilience of the lateral retinaculum. Some patients seem to have a springy endpoint, whereas others have a very stiff and unyielding restraint. Comparison with the opposite knee often reveals relatively limited correction of lateral patellar tilt on the symptomatic side. Because the iliotibial band fibers contribute to the lateral retinacular tissue, poor iliotibial band flexibility frequently accompanies abnormal lateral tilt.

Figure 62-2 Physical examination for patellar tilt. Tilt should correct to neutral.
(From Scott WN: The knee, vol 1, St Louis, 1994, Mosby-Year Book, p 445.)
Medial and lateral patellar glide testing has been well described by McConnell73 and by Kolowich et al.62 It is similar to the passive hypermobility testing described by Hughston.54 We believe that these tests should be performed with the patella in neutral tilt if possible to allow consistent comparison of the medial/lateral restraints. As described, medial patellar glide is tested with medially directed pressure on the patella and the knee in 20 to 30 degrees of flexion to effectively engage the patella in the trochlea (Fig. 62-3). This test is also effective with the knee in extension and earlier degrees of flexion. Near full extension, the ligamentous and muscular restraints may be more isolated because of less bony constraint before engagement of the patella in the trochlea. Through testing of lateral glide with the knee in extension, it is possible to palpate an endpoint to lateral translation similar to that palpable with the Lachman test. Absence of such an endpoint, together with increased translation, is highly suggestive of medial patellofemoral ligament (MPFL) deficiency. Any abnormal tightness found in the retinaculum at these lesser angles of flexion can affect the direction of patellar entry into the trochlea. Medial patellar glide is judged abnormal if medial translation is seen in less than one quadrant, as described by Kolowich and Paulos. Laterally directed pressure on the neutral patella that results in displacement of three quadrants or more is consistent with an abnormally lax medial restraint. Ligamentous laxity itself, as might be measured by quadrant displacement, should not be confused with actual subluxation and, if found, should generate caution if a realignment procedure is contemplated. Evidence of systemic ligamentous laxity should be sought in such patients before any conclusions are drawn regarding specific isolated incompetence of peripatellar restraints or malalignment. In hypermobile patients, dynamic muscular control of patellar position is even more critical. Emphasis should be placed on active muscular control and on being patient. Involuntary quadriceps contraction during positive lateral glide testing or the classic apprehension reaction to the perception of imminent dislocation is strong evidence of clinically relevant patellar instability.
Several tests have been developed to assist in the diagnosis of medial patellar instability, a condition that almost always occurs as a complication of patellar realignment. In patients with symptomatic medial patellar instability, one can displace the patella medially and then passively flex the knee, and the symptoms will be reproduced as the patella moves laterally from the subluxated position into the trochlea.85 Although the patella is moving laterally, it is moving from a subluxated position into the trochlea, essentially a “reverse apprehension” test. Another helpful test in the setting of potential medial instability is the gravity subluxation test.82 This test requires that the patient be placed in the lateral decubitus position. The patella is then manually displaced medially. Because of previous operative transection of the vastus lateralis, the patient cannot actively reduce the patella into the trochlea. Although provocative testing for medial patellar instability is not routinely necessary, these tests should be regularly included in the evaluation of patients after failed patellofemoral realignment.
Flexibility
Radiologic Evaluation
Once a complete history and physical examination have been performed, radiologic studies are frequently indicated to confirm and document the clinical impression. Standing anteroposterior and lateral x-ray films are important to search for associated conditions and patella alta. A normal ratio of patellar ligament length to patellar length of less than 1.2 has been described by Insall and Salvati.56 Blackburne and Peel8 described the ratio of the articular length of the patella to the height of the lower pole of the patellar articular cartilage above the tibial articular surface (normal, <1.0). These ratios can be used to quantify patella alta if desired. In cases in which patella alta is prominently abnormal, distal transfer of the tuberosity should be part of the surgical plan.
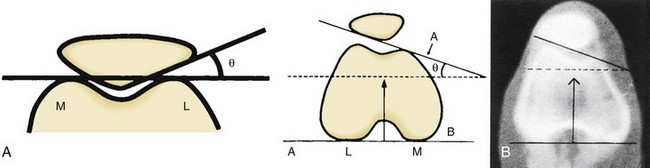
Axial tangential views of the patellofemoral joint, such as those described by Merchant et al75 and Laurin et al,65 may be used as screening tests for malalignment but can be difficult to interpret because of image overlap (unless the image is precisely tangential to the joint). The congruence angle of Merchant and Mercer and the lateral patellofemoral angle of Laurin and Dussault are estimations of lateral subluxation and tilt, respectively. The symmetry of subchondral sclerosis of the patellar facets should also be evaluated for signs of localized sclerosis (indicating unbalanced stress). These authors and their colleagues recognized the importance of imaging the patella early in flexion in the less constrained proximal femoral sulcus. Kujala and Kormano64 emphasized imaging of the patellofemoral joint in early flexion. They found greater magnetic resonance imaging (MRI) differences in tilt and lateral subluxation on views with less than 30 degrees of flexion in a group of patients with recurrent patellar dislocations than in a normal control group. CT scans, first suggested by Delgado-Martins24 in 1979, offer a significant advantage by providing imaging of earlier degrees of flexion with absolutely no image overlap. Advanced imaging studies such as CT scans assist in confirming the diagnosis and should be considered only in the evaluation of an unusual patient in whom nonoperative management fails.
Further work on CT technique, evaluation, and classification of patellofemoral disorders has been done by Schutzer and associates.97,98 Several significant advantages of CT evaluation are now clear. Use of the posterior femoral condyles as a reference plane for measurement of the patellar tilt angle has proved significantly more consistent than use of the anterior intercondylar line, as reported by Laurin and Dussault. This increases the precision with which tilt can be measured and eliminates the variable of femoral rotation40 (Fig. 62-4). Measurement of the congruence angle is also enhanced by the nature of the CT scan “slice” because it ensures that the trochlear and patellar images being measured are, in fact, at the same level and are not artifacts of image overlap (Fig. 62-5). Furthermore, a patellofemoral CT scan can be useful in detecting subtle patellar or trochlear dysplasia, such as a shallow trochlear groove in patients with lateral patellar subluxation. Moreover, limited CT evaluation of the patellofemoral joint can be accomplished quickly and at a cost similar to that of multiple conventional x-ray films. Patterns of patellofemoral malalignment on CT images are usually classified into three types. Type I is lateral subluxation, type II combines lateral subluxation and lateral tilt, and type III includes lateral tilt without subluxation (Fig. 62-6). Type IV has been defined as radiographically normal alignment.41 This classification has been very helpful in confirming the clinical impression of specific patellar malalignment patterns (tilt and/or subluxation). Treatment selection is also dependent on accurate classification, as will be appreciated in the later discussion of our recommended surgical approach.

Figure 62-5 Congruence angle as measured on a midtransverse patellar computed tomographic scan.
(From Scott WN: The knee, vol 1, St Louis, 1994, Mosby-Year Book, p 446.)
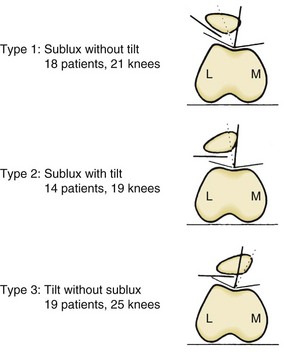
Figure 62-6 Computed tomographic scan classification of patellofemoral malalignment.
(From Schutzer SF, Ramsby GR: Computed tomographic classification of patellofemoral pain patients. Orthop Clin North Am 17:235, 1986.)
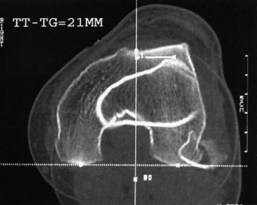
When distal realignment including tibial tuberosity transfer is considered, we believe it is wise to measure the position of the tuberosity relative to the trochlea. The most acceptable method for this consists of CT measurement of the tibial tuberosity–trochlear groove (TT-TG) distance (Fig. 62-7). Dejour and associates first described this measurement and found, upon comparing normal patients with those with patellar instability, that the threshold for normal was 20 mm.23 This measurement is done by measuring the lateral distance of the tibial tuberosity from the most posterior point in the femoral sulcus, along a line parallel to the axis of the posterior femoral condyles. Schoetle et al showed that the MRI scan may be used for this measurement as well.96 When the TT-TG distance is 20 mm or greater, available data suggest that such a measurement is abnormal on MRI or CT scan. Medialization of the tuberosity is then rational. The amount of medialization needed can also be estimated from this measurement, and the most often targeted goal for postoperative TT-TG distance is less than approximately 10 mm. Measurement of the TT-TG is helpful in confirming that tuberosity medialization is appropriate in a clinical situation that otherwise warrants medial or anteromedial transfer.
Nonoperative Management
Most patients with patellofemoral disorders improve without surgery. Dye has provided excellent reviews and a theoretical model that he calls the envelope of load acceptance model to enhance understanding of the mechanisms and reasons for improvement of patients with patellofemoral pain by rest and activity modification.27 Initial management of patellofemoral disorders should include the goals of normal flexibility and balanced quadriceps strength. One should remember to include the entire extremity in rehabilitation, especially hip strengthening. This program should be directed by specific physical examination findings. Discussion of specific techniques exceeds the scope of this chapter. In addition to reassurance, strengthening, stretching, core stability training, taping techniques, anti-pronation orthotics, and patellar braces may be very beneficial in selected patients. Weight loss in obese patients is imperative in controlling patellofemoral pain. It is sometimes surprising how well patients, even those with severe radiographic findings, do without surgery. Therefore, before surgery, it is always important to confirm that a comprehensive nonoperative treatment program has been followed.
A Rational Approach to Distal Realignment
Distal Realignment Procedures
Theory
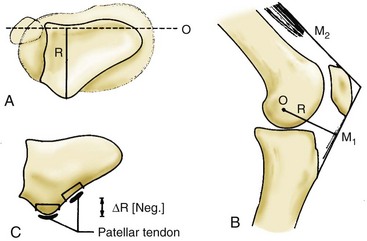
Distal realignment of the patellofemoral joint by medial transposition of the patellar tendon insertion decreases the laterally directed moment that causes patellar subluxation upon quadriceps contraction. Ideal candidates for distal realignment have laterally displaced tibial tubercles, although this has not been proven to be a prerequisite. Lateral release usually accompanies the various methods of medialization and is important in relieving any lateral tether that is present. Alternatively, advancement of medial structures, or medial patellofemoral ligament (MPFL) reconstruction, might potentially create abnormally increased medial patellar facet pressure by attempting to counteract forceful, laterally directed pull on the patella using a posteromedially directed tether on the extensor mechanism. The concept that we wish to put forth here is that the extensor mechanism must be balanced first, before medial incompetent structures such as the MPFL are reconstructed. The biomechanics of posterior displacement of the tibial tuberosity dictates an increase in joint reaction force to accomplish the same work, and this should be avoided (Fig. 62-8). Distal transfer of the tuberosity when pathologic patella alta is present helps the patella to enter the trochlea earlier in flexion and can be very helpful in some patients with patellar instability.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree