Distal Metaphyseal Osteotomies in Hallux Abducto Valgus Surgery
Thomas A. Brosky II
Patrick B. Hall
Distal metaphyseal osteotomies for the correction of hallux abducto valgus (HAV) deformity are among the most common procedures performed in podiatric surgery. The inherent stability of their basic construct allows early weight-bearing, and the ability to afford correction in multiple planes contributes to their wide usage.
Traditionally, osteotomies of the distal first metatarsal have been indicated in mild to moderate HAV deformities (Fig. 27.1). Standard recommendations are for intermetatarsal (IM) angles up to 15 degrees; however, reports of modifications of these osteotomies have demonstrated the ability to correct for larger deformities (Fig. 27.2). The flexibility of an individual deformity and its response to adjunctive soft tissue procedures may also allow for correction of IM angles exceeding 15 degrees. Distal osteotomies may be used for direct transverse correction of increased IM angles in the presence of medial bump pain, and the apical axis guide can be utilized to correct deformities in the sagittal plane. In the presence of adaptive changes at the first metatarsal head, wedging modifications may be performed either alone or in concert with proximal osteotomies.
Although distal osteotomies are versatile, there is no universal procedure for HAV correction. Each patient needs to be considered individually in deciding the appropriate procedure. Over 100 or more surgical procedures have been described for the treatment of this deformity, and though each may have its role in the treatment of HAV, not all can be included in any single discussion (1). Distal metaphyseal osteotomies such as those described by Mitchell, Hohmann, and Wilson have been included in previous editions but are seldom if ever performed by the authors and are not detailed here (2). This chapter discusses the techniques and modifications of the most commonly performed distal metaphyseal osteotomies for the correction of HAV, including osteotomy performance and fixation techniques.
APICAL AXIS GUIDE
In hallux valgus correction, use of the axis guide can assist the surgeon in manipulating and executing an accurate osteotomy. This concept allows a Kirschner wire (K-wire) to be placed from medial to lateral through the metatarsal head to help plan the actual direction of the capital fragment before the osteotomy is performed.
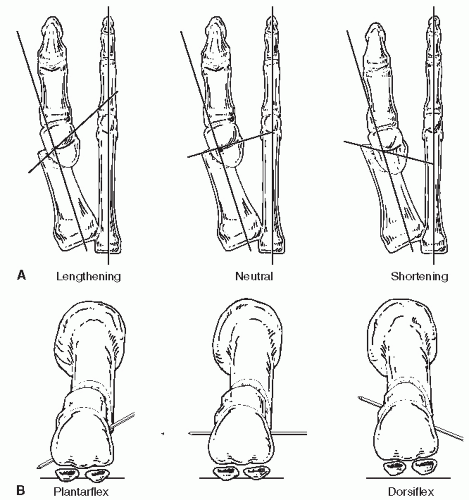
The apical axis guide utilizes a smooth 0.045-inch K-wire into the metatarsal head at the designated apex of the planned osteotomy. Placement of this wire allows for directional control of the osteotomy to correct the sagittal plane, plantarflexion, and metatarsal length, shortening or lengthening, as needed (Fig. 27.3). Once the axis wire is inserted, the surgeon need only keep the saw blade parallel to the guide in order to execute a well-fitting, stable osteotomy. Deviation from the axis guide may result in an incomplete osteotomy, converging bone cuts making lateral translation more difficult, or stress risers that could result in fracture of the osteotomy.
AUSTIN BUNIONECTOMIES
TRADITIONAL AUSTIN
Preparing the Osteotomy Site
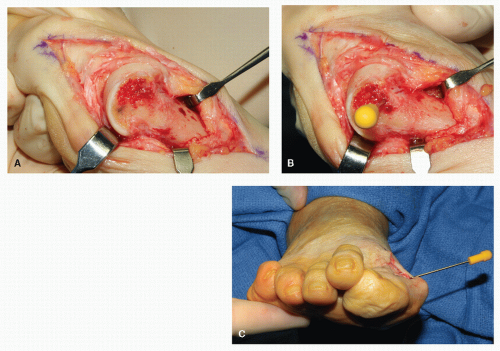
The Austin bunionectomy is a V-shaped osteotomy placed medial to lateral in the head of the first metatarsal (3). Adequate resection of the dorsomedial eminence tissue utilizing a small straight osteotome yields a smooth surface for osteotomy planning and axis guide insertion (Fig. 27.4A). The apical axis guide is traditionally placed centrally in the metatarsal head. This point can be estimated by the midpoint of the superior and inferior-most surfaces of the metatarsal head. Placement too proximal will put the osteotomy in diaphyseal bone, while placement too distal may result in intra-articular fracture. Satisfactory dissection of capsular tissues and good retraction are critical to enable accurate evaluation of this surface for axis guide placement. The authors recommend a Ragnell superiorly, elevating the dorsal insertion of the synovial fold; inferiorly, a Sayer elevator or long end of a Senn retractor enables full visualization of the plantar surface proximally. The exit site for the plantar arm of the osteotomy is determined by the proximal extent of the synovial fold. This is most easily identified during dissection with a Freer elevator and retracted with a Senn retractor. For the Austin osteotomy, fixating the plantar arm of the osteotomy with screw fixation has shown the greatest strength of construct experimentally (4). For this reason, we recommend placing the axis guide slightly superior to the midpoint of the head in order to increase the surface and strength of the weight-bearing portion and surface for fixation of the osteotomy (Fig. 27.4B and C).
Osteotomy Performance
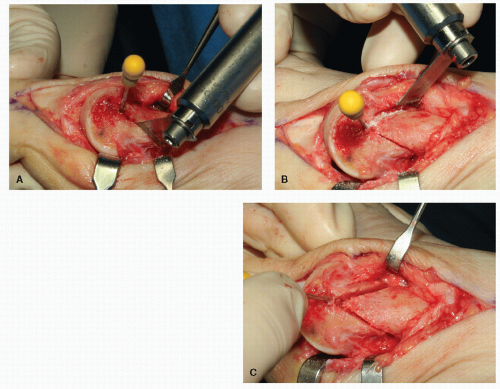
The osteotomy may be performed with either a sagittal or oscillating saw, depending upon surgeon preference. The key, however, is to maintain the saw blade in perfect alignment with the guide wire. It is recommended to perform the plantar arm first (Fig. 27.5A). Its orientation dictates the placement of fixation and allows the osteotomy to be designed to avoid the sesamoid articulation. The dorsal segment is placed just proximal to the dorsal synovial fold (Fig. 27.5B). The angle between the dorsal and plantar segments is approximately 60 degrees (Fig. 27.5C).
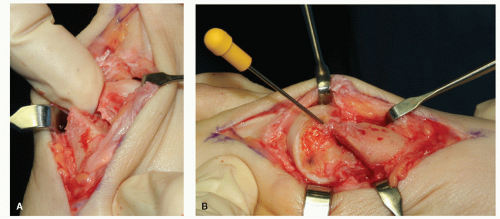
Upon completion of the osteotomy, lateral translation of the capital fragment is effected. This is easily accomplished with a gentle distal distraction force on the hallux and a lateral force on the capital fragment (Fig. 27.6A). Once the capital fragment is satisfactorily transposed, a slight impaction force will seat the osteotomy firmly and should be followed by temporary fixation with a 0.045-inch smooth K-wire. The K-wire should be place with consideration for avoiding the permanent fixative device (Fig. 27.6B).
Fixation Options
There are a number of fixation options for the Austin osteotomy. These include smooth K-wires in a “locked” fashion (Fig. 27.7A and B), cortical and cancellous screws ranging from 2.0 to 4.0 mm (Fig. 27.7C), both cannulated and noncannulated screws, as well as traditional and headless designs (Fig. 27.7D). The choice of fixation depends on patient factors such as bone quality, metal allergy, and surgeon preference.
Oblique Insertion of Partially Threaded Screw
The initial path of the screw is accomplished with a 0.062-inch smooth K-wire. This allows penetration of both proximal and distal cortices in an accurate and deliberate manner without the risk of having the drill bit skive or slide along one of the two cortices. The direction of the K-wire should be perpendicular to the plantar arm of the osteotomy on the lateral view and aimed toward the cristae between the sesamoid articular surfaces in the dorsoplantar (DP) orientation. This should be directed from proximal-dorsal to distal-plantar (Fig. 27.8A). Take this opportunity to inspect the position of the wire at the exit site to ensure sufficient purchase of the plantar segment (Fig. 27.8B).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree