Disorders of the Biceps Tendon
Brian R. Wolf
David W. Altchek
INTRODUCTION
Any overhead athlete places a tremendous amount of stress on the mechanical properties of the shoulder. Excessive stresses may lead to disorders of the biceps tendon and its anchor, ranging from inflammation and instability to degeneration or rupture. Diagnosis of disorders of the long head of the biceps and associated superior labral lesions can be problematic. This results from the often concomitant problems that are present in addition to the biceps lesion, as well as from difficulty in clinically and radiographically confirming biceps pathology. A significant amount of debate surrounds the long head of the biceps tendon with regard to its function in the shoulder. Similarly, some controversy clouds the clinical management of biceps tendon disorders. Although debate remains, there continues to be increasing interest in the role of the biceps within the spectrum of shoulder problems afflicting overhead athletes. Significant advances in technology and techniques have influenced management of biceps disorders. This chapter explores the anatomy and function of the long head of biceps at the shoulder. A discussion of the pathologic disorders that can occur involving the biceps and their proper management with specific attention to the overhead athlete follows. These disorders include inflammatory and degenerative conditions, instability of the biceps tendon, and superior labrum anterior-to-posterior (SLAP) lesions.
ANATOMY AND FUNCTION OF THE LONG HEAD OF THE BICEPS
The biceps brachii muscle has two origins: the long head and the short head. The short head originates from the coracoid process and joins the long head medially at approximately the level of the deltoid tuberosity. The long head arises from the superior aspect of the glenoid and is intimately related to the glenohumeral joint. Previous work has shown that 48% of the time, the long head arises primarily from the posterosuperior labrum, 20% from the superior glenoid tubercle, and 28% from both (1). A separate cadaver study reported approximately 50% originating from the superior labrum and the remainder from the superior glenoid tubercle, with four variations of biceps origin identified (2). The mobility of the origin of the long head of the biceps is variable, and a large amount of mobility can be normal in some shoulders (3).
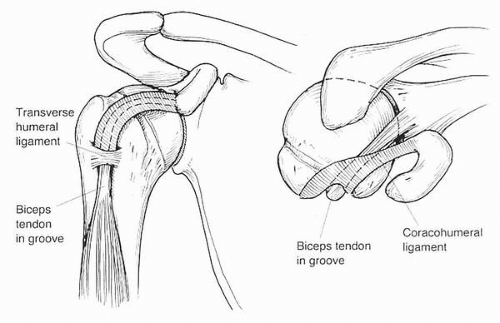
The long head of the biceps traverses the glenohumeral joint from its origin at the posterosuperior labrum and superior glenoid tubercle, through the rotator interval beneath the coracohumeral ligament, to the intertubercular sulcus between the greater and lesser tuberosities. The tendon is intraarticular but is lined by synovium, making it extrasynovial (3). The tendon turns under the “pulley” of the soft tissues that insert at the articular end of the sulcus (Fig. 15-1). These restraints include the superior glenohumeral ligament, the coracohumeral ligament, and the superior portion of the subscapularis tendon. Once in the groove, the tendon passes beneath the transverse humeral ligament that spans the groove. The groove has an average depth of 4.1 to 4.3 mm and average medial wall angle of 56 degrees (4,5). The tendon is widest at its origin and narrows distally in the arm to form a muscle belly. The blood supply to the tendon is the ascending branch of the anterior circumflex humeral artery, which runs with the tendon in the sulcus. The origin of the tendon also receives arterial supply from labral branches of the suprascapular artery (6). The musculocutaneous nerve supplies innervation.
The function of the long head of the biceps at the shoulder is controversial and not entirely understood. The biceps seems to function as a static anterior and superior restraint for the humeral head, and evidence for a dynamic role has also been reported. Neer proposed that the tendon served as a humeral head depressor and emphasized the importance of maintaining the tendon (7). Electrical stimulation of the long head of the biceps in five patients undergoing arthroscopy was shown to result in compression of the humeral head into the glenoid (8). In a study using, 15 cadaveric shoulders in a hanging arm model, superior migration was seen following intraarticular biceps tenotomy
(9). These authors concluded that the long head of the biceps stabilizes upward humeral migration during powerful biceps contraction. Similarly, superior migration during shoulder abduction in the scapular plane was shown dynamically in seven patients with isolated long head of biceps tears when compared with the intact contralateral shoulder (10). Yet, evidence exists that contradicts any major role of the biceps tendon at the shoulder. In most patients with massive rotator cuff tears not amenable to repair, whose long head of the biceps tendon has ruptured spontaneously or who have undergone a biceps tenotomy during surgical management, it is uncommon to see superior migration of the humeral head. Additionally, electromyographic (EMG) analysis in studies that have controlled for elbow motion has shown no biceps tendon activity at the shoulder in patients with either intact or torn rotator cuffs (11,12).
(9). These authors concluded that the long head of the biceps stabilizes upward humeral migration during powerful biceps contraction. Similarly, superior migration during shoulder abduction in the scapular plane was shown dynamically in seven patients with isolated long head of biceps tears when compared with the intact contralateral shoulder (10). Yet, evidence exists that contradicts any major role of the biceps tendon at the shoulder. In most patients with massive rotator cuff tears not amenable to repair, whose long head of the biceps tendon has ruptured spontaneously or who have undergone a biceps tenotomy during surgical management, it is uncommon to see superior migration of the humeral head. Additionally, electromyographic (EMG) analysis in studies that have controlled for elbow motion has shown no biceps tendon activity at the shoulder in patients with either intact or torn rotator cuffs (11,12).
Several biomechanical studies in cadaveric specimens have examined the role of the biceps tendon in glenohumeral joint stability (13, 14, 15). The long head of the biceps has been shown to significantly decrease humeral head translation in the superior, anterior, and inferior directions with increased tension placed in the tendon (14,15). Contraction of the long head of the biceps with the shoulder abducted and externally rotated produces torsional stability of the anterior capsule, which could limit force transmission to the inferior glenohumeral ligament (13). Additionally, injury to the superior labrum biceps origin complex results in increased strain on the inferior glenohumeral ligament (13) and significant increases in anterior inferior glenohumeral joint translation (16).
Evaluation and treatment of the overhead athlete requires some understanding of the physiologic muscle activation patterns seen in overhead activities. Most overhead athletic activities, such as pitching and the tennis serve, include phases of cocking, acceleration, and follow-through. EMG analysis during pitching has shown biceps function to mainly involve motion at the elbow (17, 18, 19). Moderate biceps activity is present during the cocking phase because the elbow usually is flexed in preparation for acceleration. During the acceleration phase, minimal biceps activity is seen. An increased EMG response in the long head of the biceps has been seen in throwers with instability-related symptoms as compared to those without instability symptoms (17). Significant biceps activity is seen during follow-through as the forearm is decelerated to prevent hyperextension at the elbow. It has been postulated that this high-tension period of follow-through results in SLAP lesions in some throwers (8). In analysis of professional versus amateur throwers, professional pitchers were found to use less biceps activity during both acceleration and follow-through phases (18). This implies that the elite athletes, usually with increased skill and optimal form, may use technique that lessens stress on the biceps tendon (20). An alternative “peel-back” mechanism has also been implied to result in superior labral lesions in throwers (21). In extreme abduction and external rotation, the vector of the biceps tendon changes from relatively horizontal and anterior to posterior and vertical. This vector change can result in a torsional injury, or a peeling back, of the superior biceps anchor and labrum complex. Once such an injury is present, repetitive throwing may result in propagation of the lesion.
CLINICAL EVALUATION FOR DISORDERS OF THE BICEPS TENDON
As with all shoulder conditions, a thorough history is necessary to define the nature of a patient’s symptoms. Specifics
on the onset of symptoms, progression of pain or disability, aggravating activities especially as it relates to athletics, and any treatment to date are crucial information to obtain at the onset of the evaluation. Biceps tendon pain is usually located anteriorly over the region of the intertubercular groove. This pain may migrate inferiorly into the biceps muscle region. Any popping, grinding, clicking, or feeling of subluxation or apprehension should be documented. However, biceps pain can be vague and nonspecific, often presenting in a similar fashion to impingement symptoms, labral pathology, or instability. Often biceps-related disorders occur in conjunction with other pathologic conditions, creating an overlap of symptoms. The different pathologic conditions of the biceps tendon often have subtle differences in terms of symptoms and patients’ complaints. Tenosynovitis or degenerative lesions of the biceps tendon often have anterior shoulder pain, which can sometimes be focal. Most of these patients have associated symptoms consistent with impingement. Biceps instability may develop after a traumatic event, with the patient complaining of “snapping” or “popping.” A painful clicking within the shoulder can hallmark a SLAP lesion or other labral disorder.
on the onset of symptoms, progression of pain or disability, aggravating activities especially as it relates to athletics, and any treatment to date are crucial information to obtain at the onset of the evaluation. Biceps tendon pain is usually located anteriorly over the region of the intertubercular groove. This pain may migrate inferiorly into the biceps muscle region. Any popping, grinding, clicking, or feeling of subluxation or apprehension should be documented. However, biceps pain can be vague and nonspecific, often presenting in a similar fashion to impingement symptoms, labral pathology, or instability. Often biceps-related disorders occur in conjunction with other pathologic conditions, creating an overlap of symptoms. The different pathologic conditions of the biceps tendon often have subtle differences in terms of symptoms and patients’ complaints. Tenosynovitis or degenerative lesions of the biceps tendon often have anterior shoulder pain, which can sometimes be focal. Most of these patients have associated symptoms consistent with impingement. Biceps instability may develop after a traumatic event, with the patient complaining of “snapping” or “popping.” A painful clicking within the shoulder can hallmark a SLAP lesion or other labral disorder.
PHYSICAL EXAMINATION
It is important to perform a thorough examination of the shoulder to define any pathology that may be present. The shoulder should be examined for symmetry compared to the unaffected side. Tenderness related to the biceps tendon is often located anteriorly over the intertubercular groove, located approximately 7 cm distal to the anterior edge of the acromion.Confirmation that this pain is related to the biceps is achieved by eliciting tenderness over the groove with the shoulder in slight internal rotation. This brings the groove directly anterior in the shoulder. Biceps tendon pain rotates laterally with external rotation of the arm, whereas pain related to the deltoid or other static anterior structures do not change location. Assessment of range of motion should be performed. Overhead throwers often lack some internal rotation compared with the nondominant arm. Biceps pathology can result in some motion loss over time related to pain and resultant stiffness. Impingement testing using Hawkins and Neer tests is usually positive with biceps lesions. Rotator cuff strength testing should be performed. This includes a thorough evaluation of the subscapularis, because biceps tendon pathology is often associated with lesions of the subscapularis insertion on the lesser tuberosity. The lift-off test and the belly-press test best reveal whether an intact subscapularis is present (22). Stability testing using the crank test and the load and shift test are used to evaluate for glenohumeral instability. Overhead athletes with biceps pathology related to subtle instability may present with pain only and not apprehension during these provocative maneuvers (23). Yergason’s test can isolate biceps tendon pain. This is performed with resisted forearm supination (24). Anterior shoulder pain with this maneuver is a positive result. Speed’s test is performed by elevation of the supinated arm against resistance. Again, anterior shoulder pain over the groove is considered positive and localizes pain to the biceps tendon. Detecting labral pathology is done with the use of the active compression test (25). The patient elevates the arm 90 degrees and internally rotates the shoulder approximately 10 to 15 degrees with the thumb pointed to the floor. The patient resists a downward pressure. If pain is produced, then the test is repeated with the thumb pointed to the ceiling. This is considered a positive finding if pain resolves, and the positive finding is often related to superior labral pathology. Biceps tendon instability is difficult to isolate. A test has been described in which the patient is placed supine, and palpation is done over the anterior aspect of the shoulder near the anterior acromion and intertubercular groove. The arm is abducted to 90 degrees and externally rotated to 90 degrees. A palpable snap may reveal the subluxation of the biceps tendon out of its groove (26). Differential diagnostic injections are often of benefit when considering biceps tendon pathology. Subacromial injection can improve impingement-related pain but does not improve biceps pain unless a full thickness rotator cuff tear is present. Biceps tenosynovitis or degenerative lesion pain over the anterior shoulder should be improved with an intraarticular injection or an ultrasound-guided biceps sheath injection. This can be confirmed with provocative testing done before and following injection.
IMAGING
Imaging of patients suspected to have pathology related to the biceps tendon should begin with standard x-ray studies of the shoulder including a true anteroposterior (AP), axillary, and outlet view. Lesions of the acromioclavicular joint, osteoarthritis, and a hooked acromion can be found in association with underlying biceps lesions. Degenerative lesions in the biceps related to arthritis of the groove have been described (4,27). A “groove view” is obtained by placing the cassette at the apex of the shoulder and angling the beam slightly medial to the long axis of the humerus (4). This allows for analysis of the depth of the groove and reveals any arthritic changes in the groove. Ultrasound has been advocated by many as a noninvasive and relatively inexpensive modality to evaluate the biceps tendon, sheath, and rotator cuff (28,29). Ultrasound has a reported sensitivity of 0.8 and accuracy of 0.95 in diagnosing bicipital tendinitis (5). A sensitivity of 0.75 and accuracy of 0.98 was found when ultrasound was used to diagnose biceps tendon rupture (5). Tendon dislocation or subluxation can be documented with manipulation of the shoulder during the ultrasound. The
imaging modality of choice for biceps tendon pathology is magnetic resonance imaging (MRI) (30,31). MRI can define tendon subluxation, rotator interval lesions, and superior labral pathology in detail. Any associated tears of the rotator cuff are also best defined by MRI. Consideration, however, must always be given to normal anatomic variants, especially when looking for superior labral lesions (3,32). Despite the tremendous improvement in imaging available for lesions of the biceps tendon and associated disorders, there still remains some difficulty with nonspecificity in many cases later found to have biceps pathology at arthroscopy. Imaging findings should always be considered in conjunction with symptoms and clinical findings when considering the optimal treatment course for a patient.
imaging modality of choice for biceps tendon pathology is magnetic resonance imaging (MRI) (30,31). MRI can define tendon subluxation, rotator interval lesions, and superior labral pathology in detail. Any associated tears of the rotator cuff are also best defined by MRI. Consideration, however, must always be given to normal anatomic variants, especially when looking for superior labral lesions (3,32). Despite the tremendous improvement in imaging available for lesions of the biceps tendon and associated disorders, there still remains some difficulty with nonspecificity in many cases later found to have biceps pathology at arthroscopy. Imaging findings should always be considered in conjunction with symptoms and clinical findings when considering the optimal treatment course for a patient.
PATHOPHYSIOLOGY OF BICEPS TENDON INJURIES
Most injuries to the biceps tendon and its origin can be separated into one or more of three different categories. These include inflammatory or degenerative lesions, tendon instability, and SLAP lesions (7,33,34). Often, injuries fall into two or more categories, as in the athlete with a SLAP lesion and tendon degeneration. In other cases, one injury can predispose to another, as in the case of a traumatic injury leading to tendon instability and possibly to tenosynovitis or tendon degenerative changes. Thus, there is a wide spectrum or interrelation among the diagnoses related to the long head of the biceps tendon. It is the role of the physician taking care of the overhead athlete to determine the primary cause of the pathology present and to restore optimal function to the shoulder.
TENDON INFLAMMATION AND DEGENERATIVE CHANGES
Injury to the biceps tendon produces a spectrum of disorders ranging from inflammation of the tendon sheath to various stages of degenerative change of the tendon itself. Tendinitis, or inflammation of the tendon, is a misnomer in regard to the long head of the biceps. As is the case with similar maladies involving the lateral elbow and Achilles tendon, inflammatory changes do not typically occur involving the tendon itself. Rather, inflammation of the synovial sheath of the tendon may result in tenosynovitis. Degenerative change of the biceps tendon, frequently referred to as tendinitis, is more appropriately termed tendinosis because degenerative change of the substance of the tendon occurs without evidence of inflammatory changes on a histologic level (35). Early in the process of tendon injury, the tendon remains mobile but becomes swollen. In later stages, the sheath of the tendon becomes thickened and can render the inflamed and irregular tendon immobile. Ultimately, a degenerative frayed tendon loses its gliding ability, may become scarred down, and, ultimately, can result in rupture. The overall incidence, and incidence amongst overhead athletes, of bicipital tenosynovitis or tendinosis is unknown. In patients younger than 50 years of age at the time of death, the incidence of degenerative lesions involving the long head of the biceps tendon was 12% in one cadaver study (36). None of these specimens had associated rotator cuff lesions. When evaluating a patient with inflammatory or degenerative changes of the biceps, a determination must be made regarding the cause of the pathology present. This includes a determination of whether the biceps tendon injury is secondary to some other disorder, such as impingement or instability, or is an isolated lesion within the shoulder. Most authors have considered most biceps tendon injuries as secondary lesions to other causes (7,37).
Neer described tenosynovitis of the long head of the biceps as it occurred in relation with rotator cuff injury secondary to impingement (7). Tendon injury and later rupture have been described occurring in conjunction with supraspinatus or subscapularis injury or tear in the vast majority of cases (38). The initial inflammation and later degeneration of the biceps tendon results from impingement of the tendon under the coracoacromial arch. The anterior location of the biceps tendon predisposes it to compression with activities of arm flexion and abduction. Additionally, there is a medial displacing force on the tendon, toward the lesser tuberosity, as it enters the shoulder joint and then traverses at an angle of approximately 30 degrees to the origin at the superior glenoid and labrum (39,40). This potentially adds a mechanical cause for inflammatory or degenerative changes as the tendon abrades against the medial wall of the bicipital groove. Arthritic changes in the bicipital groove have been associated with degenerative tendon changes (41).
Specific translations of the humeral head on the glenoid have been directly related to specific shoulder motions, including anterior and superior translation with flexion and internal rotation of the arm (42). Hence the follow-though phase of overhead throwing or hitting, with the arm in the flexed and internally rotated, also is associated with this anterior and superior translation of the humeral head. This places anterior shoulder structures, such as the biceps and rotator cuff, at risk for injury from impingement on the coracoacromial arch. Many throwers also exhibit decreased internal rotation thought to be secondary to an acquired tight posterior capsule. A tight posterior capsule also results in superior and anterior head translation (42), again placing the biceps at risk. Kinematic comparisons have found baseball pitchers to be at increased risk for this anterior impingement compared to football quarterbacks (43).
Jobe and colleagues were the first to describe impingement in the overhead athlete related to subtle glenohumeral instability (44) (Fig. 15-2). With overuse, the anterior stabilizing
structures of the shoulder can be overloaded and may become stretched, leading to injury to the rotator cuff, superior labrum, and biceps tendon. As the static restraints anteriorly in the shoulder become lax and weak, increased humeral head translation can occur. Subsequently, potential impingement with the coracoacromial arch can involve the rotator cuff and biceps tendon anteriorly. Eventually, the tensile limits of the anterior soft tissue structures and the biceps tendon can be overwhelmed, leading to a tendinopathy from collagen fiber damage (see Fig. 15-2). In this scenario of overuse and excessive strain, the intraarticular tendon may be overtly damaged or can appear fine with the damage occurring to the tendon located in the groove anteriorly. This may or may not be related to additional degenerative changes or abnormalities in the bicipital groove (26). Alternatively, increased translation anteriorly can result in “internal impingement” of the posterior rotator cuff on the posterosuperior glenoid labrum when the shoulder is maximally abducted and externally rotated, the cocking position for throwers (23). This may result in posterosuperior labral pathology and articular sided rotator cuff injury.
structures of the shoulder can be overloaded and may become stretched, leading to injury to the rotator cuff, superior labrum, and biceps tendon. As the static restraints anteriorly in the shoulder become lax and weak, increased humeral head translation can occur. Subsequently, potential impingement with the coracoacromial arch can involve the rotator cuff and biceps tendon anteriorly. Eventually, the tensile limits of the anterior soft tissue structures and the biceps tendon can be overwhelmed, leading to a tendinopathy from collagen fiber damage (see Fig. 15-2). In this scenario of overuse and excessive strain, the intraarticular tendon may be overtly damaged or can appear fine with the damage occurring to the tendon located in the groove anteriorly. This may or may not be related to additional degenerative changes or abnormalities in the bicipital groove (26). Alternatively, increased translation anteriorly can result in “internal impingement” of the posterior rotator cuff on the posterosuperior glenoid labrum when the shoulder is maximally abducted and externally rotated, the cocking position for throwers (23). This may result in posterosuperior labral pathology and articular sided rotator cuff injury.
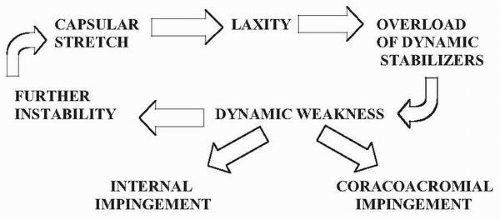 FIGURE 15-2. Diagram illustrating the vicious cycle that may occur in overhead throwers with subtle instability.
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|