CHAPTER 12 Disorders of the Acromioclavicular Joint
In those cases where the acromion has been torn off, the bone which is thus separated appears prominent. The bone is the bond of connection between the clavicle and scapula, for in this respect the constitution of man is different from that of other animals.1
DEVELOPMENTAL ANATOMY
Clavicle
As the sixth postgestation week approaches, the clavicle develops two centers of ossification for its body and becomes the first bone to ossify. In contrast to the other bones in the human body, which form from cartilaginous precursors, clavicle ossification evolves from a mesenchymal or precartilaginous stage, sometimes termed membranous or dermal bone.2 Not present at birth, a secondary center of ossification appears in the medial end of the clavicle at 18 to 20 years with union to the remaining clavicle before 25 years. A similar ossification center both appearing and uniting in the 20th year at the lateral end of the clavicle was described by Todd and D—Errico.3
Acromion and Coracoid Processes
The acromion and coracoid processes are cartilaginous at birth. As many as three secondary ossification centers have been reported for the coracoid process, which phylogenetically is a separate bone.2 These centers, as well as two for the acromion, appear between 13 and 16 years and typically unite to form a single bond between 14 and 20 years. Nonunions are possible at all sites, but are most commonly seen in the acromion (os acromiale).
ANATOMY AND FUNCTION
Overview
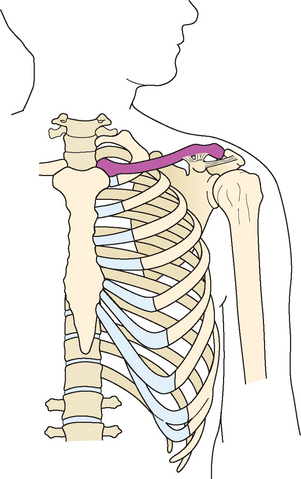
The human torso bears the upper limb by means of suspensory muscles to the scapula, clavicle, and humerus, maximizing the opportunity for movement. The muscles also serve as support for the sternoclavicular joint, the limb’s only true articulation to the axial skeleton. The clavicle braces the upper limb at a fixed distance from the axial skeleton that permits optimal movement and power (Fig. 12-1). This is possible only through the clavicle’s attachment to the scapula at the acromioclavicular joint and at the coracoid process via the coracoclavicular ligaments.
The acromioclavicular joint is said to be served by branches from the suprascapular, axillary, and pectoral nerves.4 Its blood supply is derived from the acromial branch of the thoracoacromial artery, the posterior humeral circumflex artery, and the suprascapular (transverse scapular) artery. These vessels converge to form a smaller network (acromial rete) that overlies the acromion and penetrates the joint.5
Skin
The innervation of the skin overlying the distal clavicle, acromioclavicular joint, and acromion process is predominantly via the supraclavicular nerves, deriving from cervical roots C3 and C4.6 From anterolateral to posterolateral, the coverage can overlap with the upper lateral brachial cutaneous nerve, a branch of the axillary nerve derived from cervical root C5.
Pertinent Osteology
Distal Clavicle
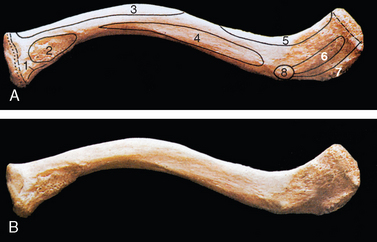
The S-shaped clavicle tapers from being a cylindrical bone medially to a more-flattened bone laterally, where superior and inferior surfaces are distinguishable. The anterior portion of the lateral clavicle articulates with the acromion process of the scapula, hence the acromioclavicular joint. On its inferior surface, points of attachment for the coracoclavicular ligaments are delineated by a slightly prominent tubercle and a more subtle line for the conoid and trapezoid ligaments, respectively (Fig. 12-2).
Coracoid Process
Oriented superior, anterior, and lateral to the axis of the scapula, the coracoid process assumes a hooked shape as it projects from the superior body of the scapula. The coracoid attachments of the coracoacromial ligament as well as the conoid and the trapezoid ligaments, together sometimes referred to as the coracoclavicular ligament, though relatively constant in location, lack specific identifying osseous prominences. The distance separating the coracoid’s superior aspect from the overlying clavicle’s inferior aspect ranges from 1.1 to 1.3 cm.7,8
Acromion Process
A rather small, facet-like portion of the anterior medial aspect of the acromion process is the articulation area with the lateral clavicle. The acromial attachment of the coracoacromial ligament is without identifying prominence.9,10
Acromioclavicular Joint Architecture
The hyaline cartilage–covered convex lateral clavicle and the concave medial acromion articulate as a true diarthrodial joint. Whether it remains so throughout life is uncertain. Transitional changes of hyaline cartilage to fibrocartilage have been reported to occur on both sides of the joint between the second and third decades of life.11
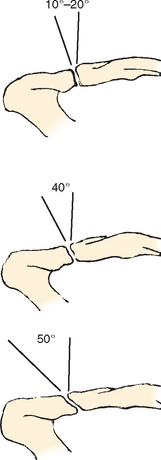
The joint normally varies in size and shape with respect to adult age, gender, and skeletal morphology.8,12 Likewise, the orientation of the sagittal plane of the joint is variable, ranging from nearly vertical to angulations from superior lateral to inferior medial approaching 50 degrees, a phenomenon that results in increasingly greater overriding of the lateral clavicle on the medial acromion (Fig. 12-3).13,14 Although less common, angulations from superior medial to inferior lateral leading to underriding of the clavicle with respect to the acromion have also been reported.15 It is not unusual for some degree of vertical incongruence of the acromioclavicular joint to exist in the complete absence of pathologic events.14,16 The relatively lax joint capsule enables essential movement while resisting displacement of the acromion over the clavicle.
Intra-articular Disk
A fibrocartilaginous disk of variable shape and size separates the acromioclavicular joint, either partly (meniscoid) or completely, into two halves. Although it is presumed to function in a manner similar to a meniscus in the knee (contributions to load distribution, joint stability, motion, and articular cartilage nourishment), its actual role is unknown. In younger patients, it is a structure potentially at risk for an acute injury, including contusion, tearing, or maceration. Structural and functional survival beyond the active years is unlikely as the disk succumbs to age-related degeneration.17–19
Ligaments
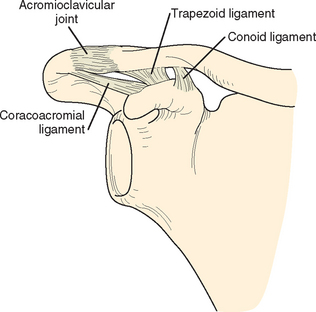
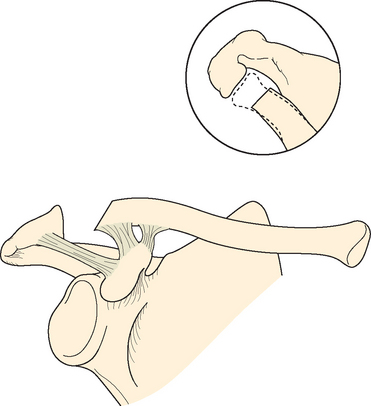
The coracoclavicular ligament is actually two ligaments, the trapezoid and the conoid (Fig. 12-4). Despite their morphologic differences, the trapezoid and the conoid ligaments have similar dimensional, viscoelastic behavioral, and structural properties.19–21
Both ligaments attach to the superior aspect of the angular region of the coracoid process. From a more anterior and lateral site that begins at the angle of the coracoid, courses in the direction of its tip, and ends posterior to the pectoralis minor tendon attachment, the trapezoid ligament is oriented toward the clavicle in a superior, anterior, and slightly lateral direction to attach at the trapezoid line on the inferior clavicle. From a more posterior and medial site on the angle, the conoid ligament expands in circumference as it runs superiorly and slightly medially toward its point of insertion, the conoid tubercle. Here the lateral one third and medial two thirds of the clavicle join to form the posterior curve of the clavicle; at the curve’s apex the conoid tubercle can be identified on the posteroinferior clavicle, just posterior and medial to the most medial aspect of the trapezoid line (see Fig. 12-2).
Distal to the angle, on the lateral aspect of the more horizontal part of the coracoid is the attachment of the coracoacromial ligament (Fig. 12-5). It joins onto nearly the entire width of the acromion process at its anteroinferior edge.
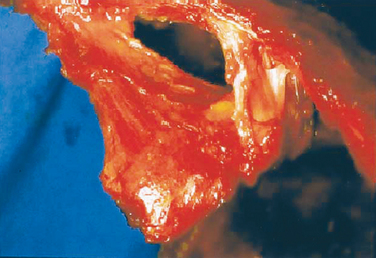
FIGURE 12-5 The coracoacromial ligament attachment to the superolateral aspect of the coracoid process.
(From Fealy S, April EW, Khazzam M, et al: The coracoacromial ligament: Morphology and study of acromial enthesopathy. J Shoulder Elbow Surg 14[5]:542-548, 2005, Figure 1).
Rios and colleagues showed that regardless of gender or race, the length of the clavicle can serve as a gauge to the determination of the anatomic attachments of the trapezoid and conoid ligaments.22 Reliable anatomic points in osteology specimens and fresh specimens were used to measure to the center of the trapezoid ligament and the medial edge of the conoid ligament. The distance from the lateral edge of the clavicle to the respective ligament point of reference was measured and used to express a ratio of the measured distance to the clavicle length. This value was 0.17 for the trapezoid and 0.31 for the conoid. In another cadaver study, Renfree and colleagues determined that there were no gender differences for the measurement from the center of the articular surface to the lateralmost point of trapezoid ligament, but the lateralmost point of the conoid ligament was more medial in men than in women.23
By way of its attachments to the clavicle and scapula, and their respective relationship to the axial skeleton and torso, the coracoclavicular ligament helps to link scapulohumeral motion and scapulothoracic motion.24–26 These two ligaments create a much stronger union of the clavicle to the scapula than the acromioclavicular ligaments. This ensures that the clavicle and scapula will move simultaneously as the acromioclavicular ligaments reach maximum tension, signifying the limits of the natural excursion of the acromioclavicular joint. The functional strength of the acromioclavicular joint increases in the presence of an intact coracoclavicular ligament.14,27 Thus, the effective suspension of the upper limb from the torso via the sternoclavicular joint and supporting musculature is assured.
Although it is tempting to simplify the function of the acromioclavicular and coracoclavicular ligaments as anterior-to-posterior and superior-to-inferior stabilizers, respectively, displacement resistance of the lateral clavicle is significantly more complex, as borne out in the results of experimental cadaver investigations.28–35 Not only are the ligaments distinguishable as discrete anatomic structures, the individual roles they play biomechanically is becoming more clear. Collectively, in the midst of a wide range of load, displacement, and restraint variables, these studies have shown that anterior restraint is afforded by the inferior acromioclavicular ligaments, posterior restraint predominantly by the superior and posterior acromioclavicular ligaments and the trapezoid ligament, superior restraint by the conoid ligament, and acromioclavicular joint compression restraint by the trapezoid ligament.36
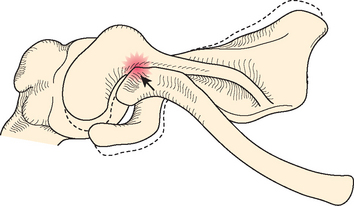
Experimental sectioning of either the conoid or the trapezoid ligaments had no effect on the overall strength of the coracoclavicular ligament.36 Complete dislocation of the lateral clavicle superior to the acromion process requires the interruption of the integrity of the conoid and the trapezoid ligaments (Fig. 12-6).14,27,33–35,37 In an experimental study using a high-speed Instron machine and loading shoulders to failure, ligament disruptions were more common than fractures.38 Age, height, and weight showed no significant relationship to the ligament cross-sectional area or the mechanical properties of the shoulder.
Coracoclavicular Articulation
Although lesser bursae can interdigitate between the layers of the conoid and trapezoid ligaments, a more prominent bursa can exist between the ligaments, sometimes sufficiently expanded to create a coracoclavicular joint between the coracoid process and the clavicle.39 Twenty cases of such an articulation were documented by dissection or with radiographs in 1939.40 The gross and histologic appearance is that of a diarthrodial joint with cartilage-covered articulating surfaces and a synovial-lined capsule and correlates with its radiographic properties (Fig. 12-7).39,40–42 The incidence of this unusual shoulder articulation is probably around 0.5% but, depending upon geographic region, can vary widely from 0.04% to 27%, and it is often bilateral (Fig. 12-8).43–53 The incidence appears to increase with age.44 It can develop in response to restricted movement of the scapula caused by variations in the shapes of the scapulae, clavicles, and first ribs.49
Symptomatic coracoclavicular joints have been reported in the settings of osteoarthritis and rheumatoid arthritis, trauma, and thoracic outlet syndrome, but the overall clinical significance of the coracoclavicular joint is uncertain (Fig. 12-9).50,54–56
Lehtinen and colleagues recognized resorption of the undersurface of the clavicle and believed it to be an atypical manifestation of rheumatoid arthritis involvement of the coracoclavicular joint.55 Corticosteroid injection into the joint has been successfully used to treat a painful coracoclavicular articulation.56 Surgical excision of the joint to resolve pain has been reported.50,53,57
EXCISION OF THE DISTAL CLAVICLE
Complete Excision
The surgical removal of the lateral clavicle is the definitive treatment for a multitude of disorders of the acromioclavicular joint. It seems that either Facassini or Morestin first performed the operation about a century ago.27,58 Subsequently, it has been the subject of many investigations seeking to define the essential yet safe extent of excision. Nearly all recommendations that have been proposed, whether the technique is performed in the traditional open manner or with an arthroscope, take into account the protection of the investing ligamentous support for the acromioclavicular joint and the coracoclavicular ligaments. By doing so, postresection instability that might contribute to discomfort and dysfunction is potentially minimized.
The recommended resection length varies from 0.5 to 2.5 cm. Although the precise amount to be excised in each instance is unknown, it would not be erroneous to suggest removing approximately 1 cm of the lateral clavicle.59 However, this recommendation lacks a high level of evidence support from the literature.60 Branch and colleagues suggested that 5 mm is adequate to prevent bony abutment in both rotationally and axially loaded shoulders if the coracoclavicular and acromioclavicular ligaments are intact.61 Boehm and coworkers advised a resection of no greater than 0.8 cm in women and 1.0 cm in men based upon cadaver studies using magnification and microcalipers.62 Exceeding the recommended amount consistently resulted in detachment of some portion of the trapezoid ligament. The anatomic study by Renfree and colleagues measured the distance from the center of the articular surface of the distal clavicle to the resected edge of the clavicle.23 They concluded that resection of less than 11.0 mm should never violate any portion of the trapezoid ligament in 98% of men or women, and resection of less than 24.0 mm should never violate any of the conoid ligament. Resection of more than 7.6 mm of the distal clavicle in men and 5.2 mm in women, performed by an arthroscopic approach, can violate the superior acromioclavicular ligament.23 Eskola showed that patients with a resection of more than 1.0 cm have more pain than patients with less than 1 cm resection.63
In a biomechanical cadaver study, Matthews and associates determined no significant differences in residual acromioclavicular joint stiffness and compressive contact between the acromion and the lateral clavicle when comparing mock 5-mm arthroscopic resection to 10-mm open resection.64 In a clinical study, Kay and colleagues advised resection of 1.0 to 1.5 cm.65
In a cadaver study by Harris and coworkers, 15.3 mm was the average distance between the end of the clavicle and the most lateral fibers of the trapezoid ligament.20 Rockwood observed cases with persistent pain after lateral clavicle excision that he attributed to inadequate resection and confirmed radiographically.66 He recommended excision of at least 2 to 2.5 cm of the clavicle, acknowledging that resection to this extent sacrifices the majority of the trapezoid ligament but spares the conoid ligament so that the lateral clavicle remains stabilized. With open techniques for lateral clavicle excision, meticulous closure of the superior capsule and investing acromioclavicular ligaments is extremely important.67
Intraoperative ultrasonography has been used for verification of appropriate arthroscopic distal clavicle excision.68
Under experimental conditions, it was predicted that when the distal clavicle is resected, higher loads may be borne by the adjacent soft tissues.69 In the same model, the intact surrounding soft tissues exerted a dampening effect with a reduction in the compressive loads across the acromioclavicular joint. In another study using cadavers, posterior translation of the clavicle was significantly reduced when the coracoacromial ligament was incorporated as an augment to the capsule repair performed at the time of open excision of the distal 1.0 cm of the distal clavicle.70
Partial Excision
Concern exists for the fate of the acromial stability at the time of open or arthroscopic subacromial decompression operations, especially when performed with coplaning of the acromioclavicular joint and distal clavicle. The inferior acromioclavicular ligament can extend as far as 10 mm lateral to the joint line.71,72 In addition, the fibers of the medial-most coracoacromial ligament can be found intimate to the inferior acromioclavicular ligaments and capsule.19,71,73 It has been shown experimentally that it is impossible to perform the standard subacromial decompression without violating the integrity of the inferior acromioclavicular ligaments on the acromion process.71 Although the immediate effect in the experimental cadaver model is anteroposterior (AP) and superior compliance increased as much as 32%, in vivo factors such as ligament healing and muscle recovery can dampen the effect of acromioplasty and coplaning. In a cadaveric study by Edwards, coplaning the lateral clavicle together with acromioplasty contributed to more joint laxity and translations of the lateral clavicle than did acromioplasty alone.74
According to studies with 4- to 7-year follow-up data, coplaning of the acromioclavicular joint at the time of arthroscopic subacromial decompression did not contribute to instability, pain, or further surgery at the acromioclavicular joint (Fig. 12-10).75–79 Contrary to these reports, Fischer and colleagues reported increased osteoarthritis and instances of symptomatic acromioclavicular joint instability, some necessitating reoperation, and expressed their concerns with coplaning at the time of arthroscopic subacromial decompression.80 This experience led to their recommendation for either resection or preservation of the entire lateral clavicle. Other authors have observed that arthroscopic subacromial decompression accompanied by coplaning or partial excision of the lateral clavicle can result in AP laxity and instability symptoms arising from the modified acromioclavicular joint.72,81–83 Kuster and associates reported that arthroscopic subacromial decompression did not accelerate the development of osteoarthritic changes in the acromioclavicular joint.72 The evidence from the literature is conflicting but suggests that coplaning can create or intensify symptoms arising from the acromioclavicular joint.60
Results of Excision
Rabalais and McCarty performed a systematic review confirming that the best level of evidence for the excision of the lateral clavicle is level III or level IV.60 From their careful analysis and identification of low levels of evidence, they concluded that the method with the best results or fewest complications could not be determined. That stated, there is little argument that excision of the lateral clavicle successfully addresses the majority of the pathologic entities encountered at the acromioclavicular joint. However, there are unsatisfactory outcomes because of cosmesis, pain, and dysfunction that have at their root mechanical more than nonmechanical factors. The factors are often interrelated and include improper resection, instability, loss of soft tissue integrity, heterotopic ossification, scars, and neuromas. The vast majority of clinical scenarios for which excision of the lateral clavicle is the only reasonable treatment to consider offer absolutely no technical challenges. It is, therefore, the execution of the technique that results in unsatisfactory outcomes.
In the orthopaedic literature, there are abundant citations of the results of lateral clavicle excision performed open.63,84–97 The report by Rabalais and McCarty indicated 76.8% excellent and good results.60 In the presence of worker’s compensation or litigation, the results might not be as predictable.89
Arthroscopic excision of the distal clavicle was first described by Johnson in 1986.98 Snyder and Esch and colleagues reported arthroscopic excision of the distal clavicle in 1988.99,100 Numerous publications that describe the techniques and the results have followed.59,65,100–118
Two studies have compared the results of arthroscopic and open excision of the lateral clavicle with confirmation of the benefits of each method.105,119 Flatow and coworkers reported earlier recovery of comfort with the arthroscopic method.105 Freedman and colleagues, using validated outcome measurements tools, showed no significant differences at 1 year, with the exception that the improvement in visual analogue scores from before surgery to 1 year postoperatively was significant for their arthroscopic group but not their open group.119 With the arthroscopic method, there is opportunity to diagnose and treat intra-articular lesions.120
The direct, or superior, arthroscopic approach to the joint is reported less often than the bursal arthroscopic approach.105,106 Although the direct approach can yield results similar to those of the bursal approach, a possible disadvantage is that it places the important superior stabilizing structures at risk.113 Continued pain and instability in the AP plane have been reported after arthroscopic lateral clavicle excision, sometimes necessitating further reconstruction (Fig. 12-11).80,81,113,115 Inadequate or uneven bone resection has been reported after arthroscopic lateral clavicle resection.103,105,108,112 The report by Rabalais and McCarty indicated 92.5% excellent and good results with arthroscopic lateral clavicle excision.60
Rabalais and McCarty analyzed level IV evidence reports of lateral clavicle excision performed in conjunction with other procedures and reported 94.7% excellent and good results.60,65,112,114,116,121–123
Heterotopic ossification and calcification can occur after an acromioclavicular joint injury or following the excision of the lateral clavicle.84,85,114,116,124 Symptomatic ossification or calcification is quite uncommon, although it may be an offending lesion when the outcome of distal clavicle excision by either open or arthroscopic methods is not considered satisfactory (Fig. 12-12).91,116,124 Patients at high risk for developing heterotopic ossification, such as those with previous history of the lesion or patients having either hypertrophic pulmonary osteoarthropathy or spondylitic arthropathy, may be candidates for pharmacologic prophylaxis.
It appears that lateral clavicle excision, regardless of method, following trauma to the acromioclavicular joint produces fewer excellent and good results than when it is performed for nontraumatic conditions.60,89,90
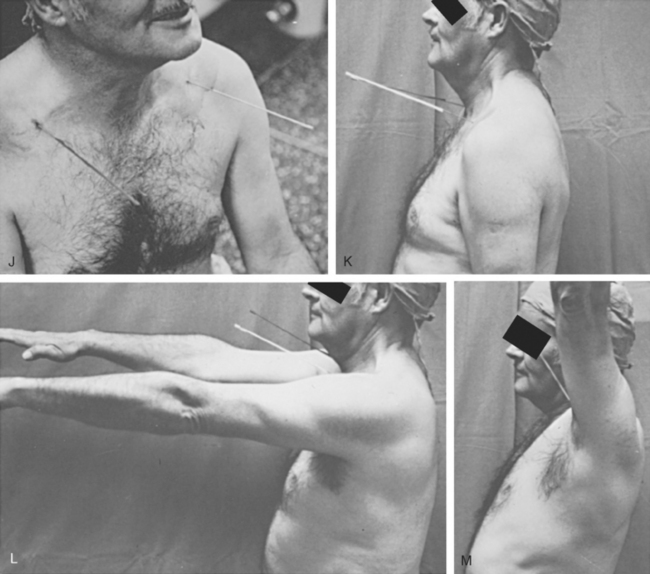
Author’s Preferred Method
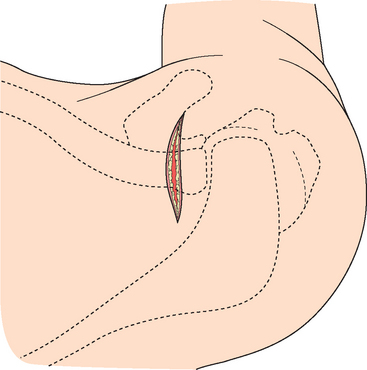
The patient is placed in the beach chair position with the head supported on an adjustable well-padded headrest to allow free access to the superior aspect of the shoulder. The skin incision is made in the relaxed skin tension lines approximately 1 cm medial to the acromioclavicular joint, extending for 3 to 4 cm (Fig. 12-13). A small straight Gelpi retractor is placed into the subcutaneous tissue, which is gently elevated from the underlying fascia.
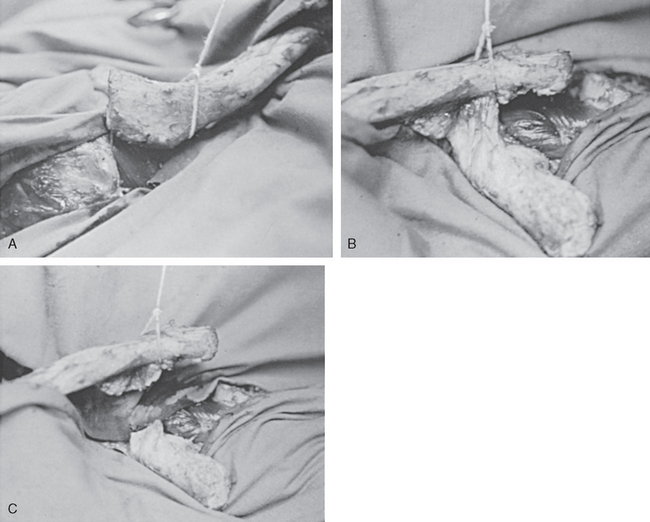
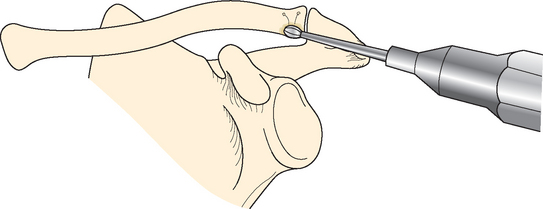
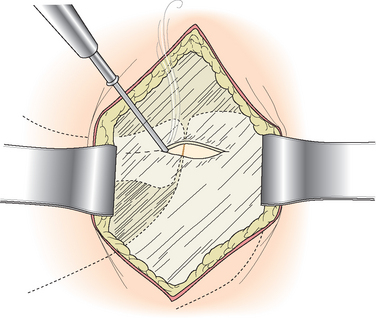
Beginning 2.0 to 2.5 cm medial to the acromioclavicular joint, electrocautery is used to incise the soft tissue overlying the superior aspect of the clavicle (Fig. 12-14). The incision should be carefully placed to avoid the trapezius and deltoid muscles from their respective insertions. The incision is continued laterally through the capsule of the acromioclavicular joint onto the acromion process for a distance of approximately 0.5 to 1 cm. Subperiosteal dissection of the distal clavicle is carried out with electrocautery to create anterior and posterior soft tissue flaps that include the capsule, the superior ligaments of the acromioclavicular joint, and the adjacent muscles. Complete soft tissue dissection is confirmed with a 0.25-inch Key elevator enabling the placement of two small Chandler retractors bent to 90 degrees anterior and posterior to the distal clavicle. A length of 1.25 cm of the distal clavicle is measured, marked, and resected using a microsagittal saw (Fig. 12-15). The resected fragment is grasped with a towel clip or pointed bone-reduction forceps and manipulated to allow access for the release of the remaining soft tissue attachments inferiorly.
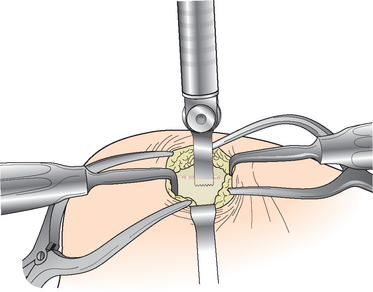
FIGURE 12-15 The surrounding soft tissues are protected as the lateral clavicle is excised with a microsagittal saw.
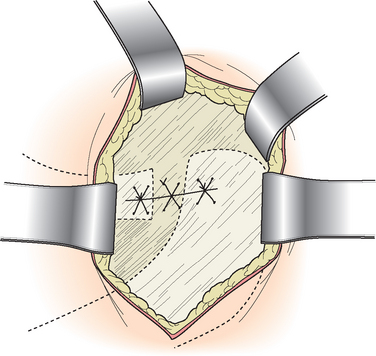
The surrounding soft tissues are infiltrated with a local anesthetic solution consisting of equal parts of 0.5% Marcaine with epinephrine and 1% lidocaine. With the medial subcutaneous flap retracted with a bent Army–Navy retractor, a 6-D Mayo trocar needle delivers No. 2 nonabsorbable suture through the anterior and posterior soft tissue flaps (Fig. 12-16). No more than three sutures placed with a figure-of-eight technique are usually necessary. The sutures are tied with four throws to limit the likelihood of palpable and potentially painful knots beneath the skin at the surgical site. Leaving a small tag further reduces the possibility of palpable suture. For extremely thin patients, an absorbable suture is preferred. The subcutaneous tissue is closed with 2-0 absorbable suture using a buried technique, capturing the dermal layer to ensure excellent superficial soft tissue apposition. Strips of 0.5-in adhesive-backed paper tape cut in half are applied to the skin. A sterile dressing covers the wound and the arm is placed in a sling.
Patients are discouraged from active arm elevation without the assistance of the opposite limb for 3 to 4 weeks to protect the deep soft tissue repair. Heavy use of the extremity is not recommended for 6 to 8 weeks to ensure that sufficient preliminary healing of the acromioclavicular ligaments has taken place and that the residual void created at the time of distal clavicle resection has been filled with scar. Hydrotherapy to obtain range of motion is suitable as soon as the wound is dry. Return of full strength, range of motion, and full function can be expected in most cases by 12 weeks.
Technical Pearls and Pitfalls
Optimum and safe placement of the saw is enabled by placing the skin incision approximately 1 cm medial to the palpable prominence of the distal clavicle. The angle of resection favors removing slightly more bone superiorly and posteriorly than inferiorly and anteriorly (Fig. 12-17). This orientation of the plane of resection prevents contact between the remaining clavicle and the acromion when the arm is placed in cross-body adduction. A saw is preferred to the use of either a bur, which creates more bone debris, or an osteotome, which can shatter the bone.
Summary
Disorders of the distal clavicle that result from internal derangement of the acromioclavicular joint or irreversible deterioration of its articular surface can be effectively treated with excision of the distal clavicle through a limited open surgical approach. It is very important to carefully preserve the soft tissues contiguous with the joint capsule. A sufficient resection requires removal of no less than 1 cm and no more than 2.5 cm of the distal clavicle.
BIOMECHANICS OF ACROMIOCLAVICULAR MOTION
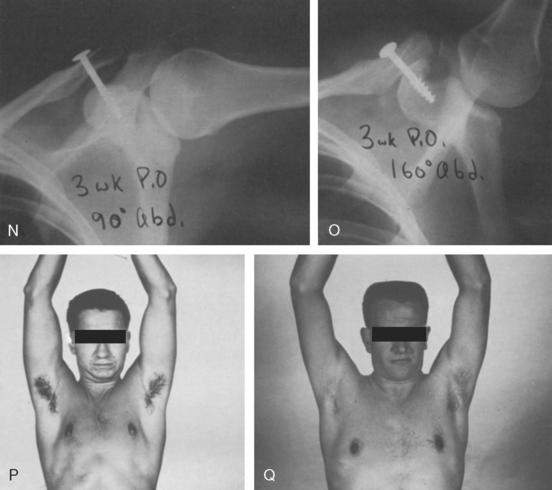
Based upon observations of patients with acromioclavicular joint arthrodesis, observations of the movement of pins drilled into the skeleton under certain conditions, and the data from investigational laboratory models, opinions vary with respect to the amounts and types of movement that takes place at the acromioclavicular joint. With upper limb elevation, Inman and associates recognized 20 degrees of acromioclavicular joint motion and 40 to 50 degrees of clavicle rotation.25 Codman was the first to suggest that the motion was far less, around 5 degrees.24 Caldwell’s patients with acromioclavicular arthrodesis had excellent range of motion.125 The studies of Kennedy and Cameron provided the initial description of the downward scapular rotation occurring in conjunction with upward rotation of the clavicle during upper limb elevation.26,126 Codman’s opinion was later supported by the investigations of Rockwood, who detected only 5 to 8 degrees of acromioclavicular joint motion (Fig. 12-18).24,33–35 Rockwood surmised that in the presence of the diminutive amount of motion at the acromioclavicular joint, full or nearly full elevation of the upper limb was only possible with 40 to 50 degrees of upward rotation of the clavicle and by the simultaneous downward rotation of the scapula. He termed the phenomenon synchronous scapuloclavicular motion and acknowledged the earliest description by Codman and later by Kennedy and Cameron (Fig. 12-19).24,26,126
Recent studies have enabled a more complete understanding of the complex motion interactions of the upper limb, scapula, clavicle, and thorax and appear to have validated the conclusions of the pioneering investigators. As the upper limb raises, the clavicle elevates 11 to 15 degrees and retracts 15 to 29 degrees.127 This motion is linked to the movement of the scapula by means of the acromioclavicular joint, the coracoclavicular ligaments, and the deltoid and trapezius muscles, whose attachments the two bones share. When the upper limb is elevated in the scapular plane, the scapula not only rotates 50 degrees upward but also tilts posteriorly 30 degrees around a medial–lateral axis and externally rotates 24 degrees around a vertical axis.128 Sahara and colleagues performed a three-dimensional (3D) kinematic analysis of the acromioclavicular joint using magnetic resonance imaging (MRI) and observed that the scapula rotated 35 degrees on an axis that passed through the insertions of the acromioclavicular and coracoclavicular ligaments on the acromion and coracoid process, respectively.129 They also showed that with abduction, the lateral clavicle translated 3.5 mm in the AP and 1 mm in the superior directions.
Changes in the position of the scapula with respect to the clavicle are accompanied by a subtle gliding motion between the articular surfaces of the acromioclavicular joint and virtually undetectable motion through the coracoclavicular ligaments. Mazzocca and coworkers considered the mechanical coupling of the clavicle, the scapula, and upper limb elevation vital to upper limb motion and function.130 They stated, “the acromioclavicular joint should not be fixed, either by fusion, joint-spanning hardware (screws, plates, pins) or by coracoclavicular screws. Motion will be lost, limiting shoulder function, or the hardware can fail.”
SPECTRUM OF DISORDERS
The most prevalent disorder of the acromioclavicular joint is degenerative disease. From his classic studies of the aging shoulder, DePalma was able to determine that most persons experience acromioclavicular joint deterioration with advancing age.131,132 His work revealed a pattern of age-related changes within the joint emerging as early as the third or fourth decade of life and increasing exponentially with time. The incidence in the shoulder is far less than in the hip or knee, but it is notable that the acromioclavicular joint is affected significantly more often than the glenohumeral joint.133 These pathologic changes of the joint are recognized radiographically as osteoarthritis.
The acromioclavicular joint is commonly involved with inflammatory arthritis, especially in the more-advanced stages.134 Superior ascent of the humeral head associated with cuff-tear arthropathy and massive defects in the rotator cuff can erode the acromioclavicular joint, eventually leading to destruction of the joint, sometimes with the formation of large cysts that can mimic a soft tissue tumor.135–137 Crystal arthropathy with acromioclavicular joint involvement and other forms acromioclavicular arthritis are uncommon. Infections of the acromioclavicular joint are uncommon, even when the general health of the patient is compromised.138 Neoplasms, both benign and malignant, as well as proliferative disorders of the synovium very rarely affect the acromioclavicular joint.139
EVALUATION
History
Pain is the most common symptom of an acromioclavicular joint disorder. Without prompting, nearly all patients point directly at the acromioclavicular joint or its vicinity when they begin to describe their symptoms However, the expression of acromioclavicular joint pain may be altogether different as reported in an interesting study by Gerber and colleagues.140 Hypertonic saline injected into the acromioclavicular joint of otherwise asymptomatic volunteers resulted in variable pain patterns that included not only the acromioclavicular joint but also the area of the anterolateral deltoid, the suprascapular region including the trapezius and the supraspinatus, and the anterolateral aspect of the neck.
The positive value of pain diagrams for detecting and diagnosing acromioclavicular disorders was shown by Walton and colleagues.141 For the patient exhibiting shoulder pain between the mid clavicle and the deltoid insertion with a positive Paxinos test (described under Physical Examination) and a positive bone scan for uptake at the acromioclavicular joint, the researchers were convinced that the diagnosis of acromioclavicular joint pain was “virtually certain.”
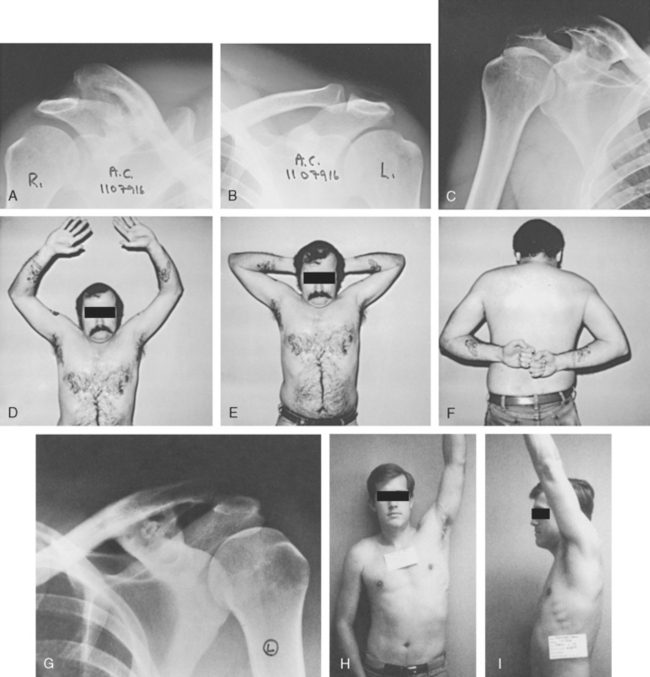
Physical Examination
With the patient either sitting or standing and the overlying clothing removed from both shoulders, the examiner looks for asymmetry: shoulder posture at rest, skin color, muscle bulk, and surface topography (Fig. 12-20). Both shoulders are examined for active motion, voluntary provocative maneuvers, skin temperature, tenderness, ligamentous laxity, passive motion, sensation, strength, circulation, and discriminatory maneuvers. The depth of examination of the cervical spine, remaining components of the shoulder girdle, and the upper limb is variable and determined individually.

FIGURE 12-20 Patient preparation for physical examination requires unimpeded access to both shoulders.
Asymmetric tenderness well localized to the acromioclavicular joint indicts the acromioclavicular joint as the source of symptoms, especially if the pain so produced is essentially the same in character as the pain experienced by the patient. It is sometimes very difficult to confidently identify and successfully palpate the acromioclavicular joint when the patient is obese or very muscular. In these instances, it might prove helpful to reference the triangle formed by the clavicle, scapular spine and base of the neck. The acromioclavicular joint is directly anterior to an examining fingertip placed just medial to the acromion process at the lateral apex of the triangle (Fig. 12-21).
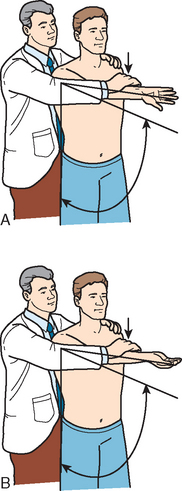
Several pain-exacerbating examination maneuvers that indicate acromioclavicular joint pathology have been described, including the cross-body adduction stress test, the acromioclavicular resisted-extension test, Buchberger test, the active compression test, and the Paxinos test.141–145 With the cross-body adduction stress test, the examiner passively elevates the upper limb to 90 degrees in the sagittal plane and, with the elbow either extended or flexed slightly, moves the limb medially (Fig. 12-22).144 The test is considered positive if it reproduces pain in or near the acromioclavicular joint.
The acromioclavicular resisted-extension test starts with the upper limb elevated 90 degrees in the sagittal plane, the elbow flexed to 90 degrees, and internal rotation to 90 degrees (Fig. 12-23).143 With the examiner’s hand fixed in space against the posterior elbow, the patient extends the shoulder in the transverse plane, meeting the examiner’s resistance. The test is considered positive if pain is experienced in the acromioclavicular joint.

FIGURE 12-23 The acromioclavicular resisted-extension test is performed in this patient with shoulder pain.
The Buchberger test combines inferiorly directed force to the lateral clavicle with passive forward elevation of the slightly adducted and externally rotated upper limb.142 The test is considered positive if pain is invoked or intensified in or near the acromioclavicular joint. To perform the Paxinos test, the examiner places a thumb over the posterolateral acromion and the ipsilateral or contralateral index or long finger (or both) over the superior aspect of the mid-part of the clavicle.141 Anterosuperior pressure is applied by the thumb while inferior pressure is applied to the acromion. The test is considered positive if pain is produced or intensified in the region of the acromioclavicular joint (Fig. 12-24).

FIGURE 12-24 The Paxinos test. The thumb and finger are squeezed together.
(From Walton J, Mahajan S, Paxinos A, et al: Diagnostic values of tests for acromioclavicular joint pain. J Bone Joint Surg Am 86[4]:807-812, 2004.)
The active compression test is begun by requesting the patient to fully extend the elbow and forward elevate the upper limb 90 degrees in the sagittal plane followed by 10 to 15 degrees medial to the sagittal plane (Fig. 12-25).145 The thumb is pointed downward by full internal rotation of the shoulder and pronation of the forearm. An inferiorly directed force is applied to the upper limb thus positioned. The force is released, the forearm is fully supinated, and the force is reapplied. The test is considered positive if pain is produced with the first maneuver and reduced or eliminated with the second maneuver. Pain in or near the acromioclavicular joint indicates a problem of the acromioclavicular joint.
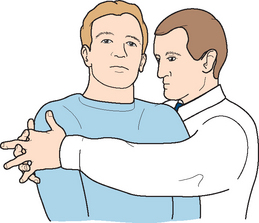
I learned the hug test from Douglas Harryman, II, MD, and Frederick A Matsen, III, MD, as an additional clinical tool for assessing the acromioclavicular joint (Fig. 12-26).146 The examiner stands at a right angle to the patient’s symptomatic side, reaches around the patient’s shoulders, and locks both hands together. The hug is then performed, compressing both shoulders in the coronal plane between the examiner’s chest and hands. The test is considered positive if pain is produced or aggravated in or near the acromioclavicular joint closest to the examiner.
Maritz and Oosthuizen showed high sensitivity for acromioclavicular joint line tenderness and cross-body adduction stress testing.147 O—Brien and associates determined that the active compression test exhibited high degree of accuracy (100% sensitive and 96.6% specific) for acromioclavicular joint lesions.145
In the study by Walton and colleagues, acromioclavicular joint tenderness to direct palpation had the greatest sensitivity for the detection of acromioclavicular joint disorder in patients with shoulder pain, followed by the Paxinos test.141 They also reported that the most accurate clinical maneuver for detecting an acromioclavicular abnormality was the Paxinos test. Chronopoulos and coworkers analyzed patients with isolated chronic disorders of the acromioclavicular joint to determine the diagnostic value of physical examination provocative testing techniques.148 The most sensitive test, the cross-body adduction test, was also the least accurate. The active compression test had the greatest specificity, the least sensitivity, and the most accuracy. The acromioclavicular resisted-extension was between the other two for all diagnostic values. Interestingly, provocative maneuvers described for other shoulder maladies (Neer impingement sign, Hawkins impingement sign, painful arc sign, drop arm sign and Speed’s test, Jobe’s sign, neck tenderness) are capable of inducing pain in patients with chronic lesions of the acromioclavicular joint.147,148
The response to local anesthesia instilled into the acromioclavicular joint can help identify the cause of shoulder pain.141 This is especially true when provocative testing is performed both before and after the injection.
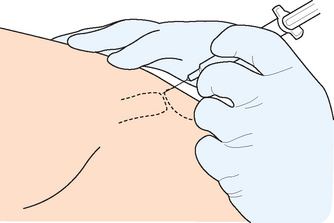
Despite the very superficial location of the acromioclavicular joint, its relative size, variable anatomy, and pathologic changes often confound arthrocentesis. Successful needle entry into the joint often lacks tactile confirmation (Fig. 12-27). Bisbinas and colleagues reported incorrect placement more than 60% of the time when orientation to the joint was obtained by palpation alone.149 When accuracy of injection was deemed critical, they recommended using image guidance. In a cadaver study, acromioclavicular joint injection accuracy was 67%.150
Imaging
Plain Radiographs
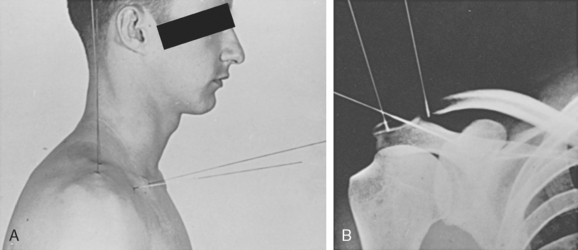
Due to its composition of less-dense bone and its location in a region of the shoulder with relatively less soft tissue coverage, standard shoulder techniques must be altered to properly delineate the acromioclavicular joint. Depending upon the patient’s stature or body habitus, a reduction of x-ray kilovoltage by as much as one half is sometimes necessary in order to gain optimal visualization of the acromioclavicular joint.66,151
In addition, a filter can be placed between the patient and the film cassette for further image enhancement (Fig. 12-28). Better techniques decrease the probability of misdiagnosis (Fig. 12-29).
Anteroposterior View
It is preferable to obtain this view with the patient either standing or sitting with the arms unsupported and neutrally positioned in the sagittal plane. Anatomic variations and technical inconsistencies are effectively dealt with by imaging bilateral acromioclavicular joints simultaneously on a single cassette or on two smaller cassettes for wider patients (Fig. 12-30). A 10- to 15-degree cephalic tilt applied to the x-ray beam optimizes the image of the acromioclavicular joint by eliminating is superimposition on the posterior acromion and lateral scapular spine (Fig. 12-31).151
Dimensions and configuration are extremely variable, mandating a cautious approach to interpretation in the setting of injury.14,152 Acromioclavicular width ranges from 0.5 mm to 7 mm.151,153,154 The coracoclavicular interval ranges from 1.1 cm to 1.3 cm.7,8
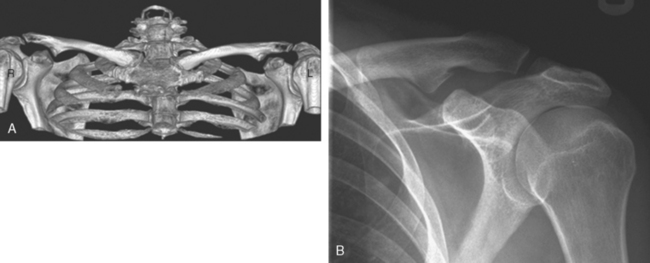
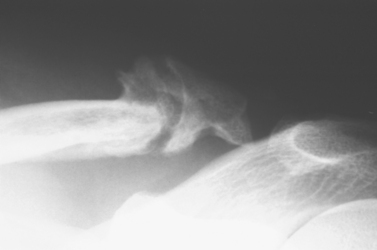
Lateral Views
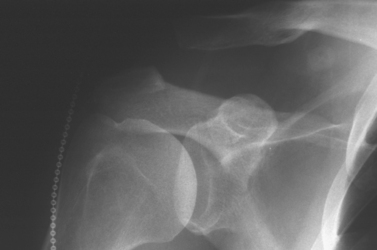
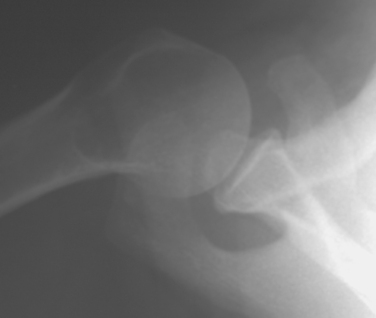
One of two views is selected: either an axillary lateral view or a scapular Y view. The axillary view offers an advantage for determining the anterior or, much more commonly, posterior displacement of the clavicle (Fig. 12-32). The scapular Y view highlights superior displacement of the clavicle, although posterior displacement can be demonstrated (Fig. 12-33).
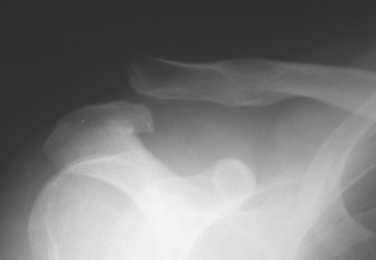
Stress Views
It is sometimes possible to subject the acutely injured shoulder to an additional deforming stress as an aid to diagnosis. A radiograph obtained simultaneously with the stress maneuver often captures the critical information sought by the examiner (Fig. 12-34). Stress views can facilitate the diagnosis and characterization of the severity of an acromioclavicular dislocation, although some question their value.155–157 In a survey of members of the American Shoulder and Elbow Surgeons, 94% responded; 81% indicated that they did not recommend the routine use of stress radiographs in the emergency department157 and 57% did not use the views. Only 9% changed their treatment plan based upon the outcome of the views. The radiographic assessment for nontraumatic conditions of the acromioclavicular joint does not usually incorporate stress views.
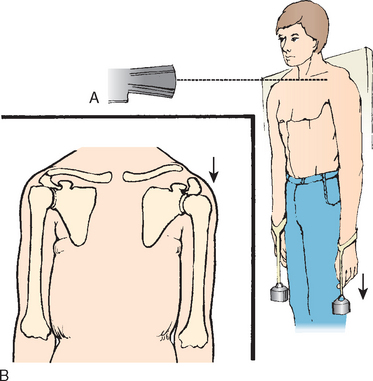
Anteroposterior Stress Views.
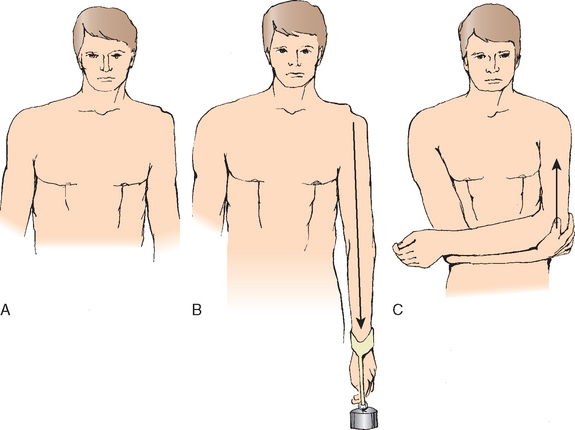
For standard AP stress views, the technical principles and patient positioning are unchanged from routine AP views of the acromioclavicular joint. Stress of 10 to 15 pounds is applied to both upper limbs while the patient is invited to relax as much as possible (Fig. 12-35). The method of weight attachment to the upper limb, hand-held versus wrist-suspended, might not be important.158 It may be possible to ascertain avulsion of the anterior deltoid by other forms of stress application, but the accuracy of a weight-lifting view and its role in the routine assessment of suspected acromioclavicular dislocations has yet to be determined.159
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree