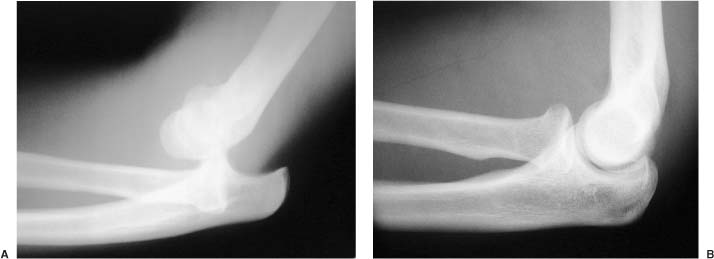
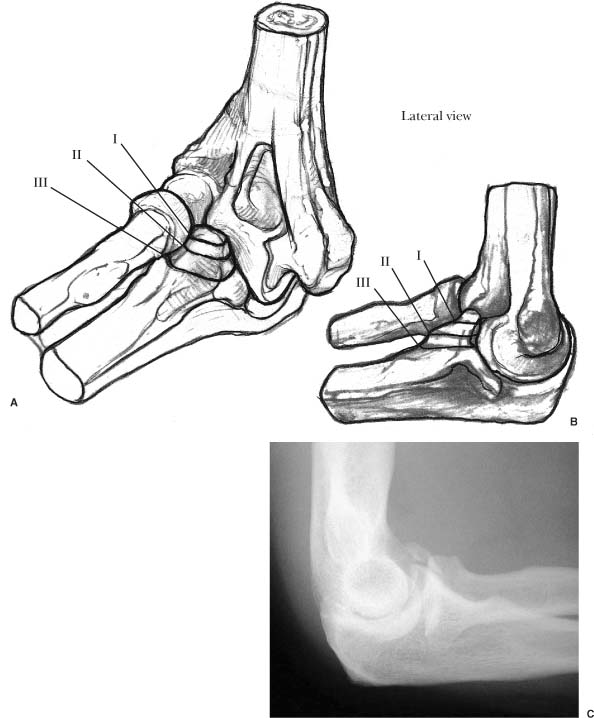
1 Elbow stability is conferred by static and dynamic constraints. The primary stabilizers of the elbow are the ulnar collateral ligament (primarily the anterior band of the ulnar collateral ligament), the lateral collateral ligament (ulnar part), and the ulnohumeral articulation. The coronoid and the trochleohumeral articulations are crucial components to articular congruity. The elbow joint is comprised of the articulation of three bones: the humerus, the radius, and the ulna. The joint can be subdivided into the radiocapitellar articulation laterally, the ulnohumeral or trochleohumeral articulation medially, and the proximal radioulnar joint, where the radial head articulates with the lesser sigmoid notch of the ulna. The distal humerus consists of two condyles. The lateral condyle ends with the lateral epicondyle and the articular surface of the capitellum. The lateral epicondyle serves as the attachment of the lateral collateral ligament and the extensor muscle group. The medial condyle ends with the more prominent medial epicondyle and the trochlea. The medial epicondyle serves as the attachment of the ulnar collateral ligament and the flexor-pronator muscle group. Anteriorly, the coronoid fossa receives the coronoid process of the ulna; posteriorly, the olecranon fossa receives the tip of the olecranon. The lateral collateral ligament complex is comprised of the radial collateral ligament, which arises from the lateral epicondyle and inserts onto the annular ligament. The annular ligament originates from the anterior aspect of the lesser sigmoid notch and inserts on the crista supinatoris (supinator crest) and holds the radial head reduced against the ulna. The ulnar part of the lateral collateral ligament (LUCL) is the main lateral stabilizer of the elbow.1 It also originates from the lateral epicondyle and inserts on the crista supinatoris. The ulnar collateral ligament complex originates from the medial epicondyle and inserts onto the base of the coronoid. It is comprised of the anterior, posterior, and transverse bands. The anterior band has the biggest role in medial stability of the elbow joint.2 It has been further subdivided into anterior and posterior bundles. Unlike the lateral collateral ligament, which is isometric throughout the range of motion of the elbow, the ulnar collateral ligament originates from a site that is away from the axis of rotation. Therefore, different portions of the ligament will tighten at different angles of flexion. The anterior bundle of the anterior band is tight in full extension. At 60 degrees of flexion, the posterior bundle of the anterior band starts to tighten. At 90 degrees, the posterior band starts to tighten and is tightest past 90 degrees. At 120 degrees, the anterior bundle of the anterior band becomes loose, and the posterior bundle of the anterior band and the posterior band are the main stabilizers. The transverse band does not have a major role in stability. Next to the shoulder, the elbow is the most frequently dislocated joint.3 Dislocations account for 11 to 28% of injuries to the elbow.4 The mechanism of injury is a fall on an outstretched arm. It can also result from direct trauma, motor vehicle accidents, and high-energy trauma from sports injuries. Over 90% of dislocations are in the posterior and posterolateral direction. O’Driscoll et al5 have postulated that as a person falls on an outstretched arm, an axial load is placed on the elbow. The body then rotates internally on the fixed, supinated forearm, resulting in a valgus moment placed on the elbow. This causes a posterolateral dislocation of the elbow. Elbow dislocation occurs in stages of soft tissue disruption extending from the lateral side of the joint to the medial side.6 In stage 1, the ulnar part of the lateral collateral ligament is disrupted resulting in posterolateral rotatory subluxation. In this stage, the subluxed elbow can reduce spontaneously. In stage 2, there is further soft tissue tearing anteriorly and posteriorly, resulting in a partial dislocation. On a lateral radiograph, the trochlea appears perched on the coronoid. In stage 3A, all the soft tissue structures are torn except for the anterior band of the ulnar collateral ligament. In this stage, a complete dislocation is possible. In stage 3B, the anterior band of the ulnar collateral ligament is also torn. The patient presents with a history of trauma, swelling, and deformity about the elbow. Although neurovascular injury is rare, a thorough neurovascular examination should be performed before and after the reduction procedure. Other associated injuries have been reported in 10 to 15% of cases, such as distal radius fractures, perilunate dislocations, and shoulder injuries.7 The interosseous membrane and the distal radioulnar joint should be examined to rule out an Essex-Lopresti injury. Radiographs should be carefully examined to diagnose associated injuries such as coronoid fractures, radial head fractures, and avulsions of medial or lateral epicondyles (Figure 1-1). FIGURE 1-1. (A). Lateral radiograph of a simple posterior elbow dislocation. (B). Postreduction radiograph shows a well-reduced joint where the radial head articulates with the capitellum without subluxation. Reduction should be performed with adequate anesthesia and muscular relaxation. A general anesthetic is preferred; however, if adequate anesthesia can be achieved, the reduction could be performed in the emergency room. Several reduction maneuvers have been described. First, the medial and lateral displacement should be corrected, followed by longitudinal traction. Pressure should be applied to the olecranon to push the forearm anteriorly. The forearm should be supinated to clear the coronoid around the trochlea. The elbow is then examined under anesthesia. The stable range of motion should be documented. Any blocks to a full range of motion should be felt because this could indicate intra-articular free fragments. Varus and valgus stability should be assessed at full extension and at 30 degrees of flexion so that the olecranon is brought out of the olecranon fossa. With the forearm in pronation, the lateral structures are tightened and an assessment of the medial structures is better determined. The lateral soft tissues are always torn with a dislocation and do not need to be individually assessed. Nonoperative treatment of simple elbow dislocations traditionally has yielded good results.4,7–9 The elbow is placed in a well-padded posterior molded splint. The rotation of the forearm depends on the amount of instability. If the elbow is unstable with the forearm in neutral rotation, pronation of the forearm will tighten up the lateral side and help maintain the reduction. Radiographs are taken after the splint is applied, and the maintenance of the reduction is verified. Close attention should be paid to the lateral side of the joint. The radial head should line up with the capitellum in all views. The patient is seen in 7 days in the clinic. Repeat radiographs are taken to ensure the reduction of the elbow joint. The immobilization is removed, and an aggressive active rehabilitation program is begun. Radiographs should be repeated once again within 14 days of reduction to ensure that reduction is maintained. The use of indometh-acin to prevent heterotopic ossification in simple dislocations is controversial. We do not routinely use indomethacin at our institution. Operative treatment of simple dislocations is rarely indicated. One of the indications for surgery includes associated fractures (complex dislocations), which will be discussed in the next section. Another indication is persistent instability despite a closed reduction and immobilization. An examination under anesthesia is performed to determine the stable arc of motion. Josefsson et al10 noted that the more unstable the elbow is during examination under anesthesia, the more likely that the muscular attachments could be detached. All elbows demonstrate instability with a valgus load; however, only about half of the elbows show lateral instability.11 Surgery would include a close inspection of the joint surfaces for osteochondral fragments and removal of these loose bodies. Durig et al12 have found cartilage abrasions and loose bodies in 100% of cases treated surgically. Surgical explorations have found that the ular and lateral collateral ligaments are ruptured in all cases.11 The flexor-pronator mass is avulsed in 6010 to 80%11 of cases, and the extensor muscle mass is avulsed 4011 to 46%10 of the time. Extensive damage to the anterior capsule and brachialis muscle is also noted.11 The surgical repair would include the reattachment of the collateral ligaments, the muscles detached from the epicondyles, and the anterior capsule. A lateral and medial incision can be used; however, a posterior utilitarian approach is best in case future operations are required. Both the medial and lateral sides should be explored and the pathology addressed. Either suture drill holes or suture anchors can be used to reattach the ligaments and tendons to their anatomic/isometric positions. This is crucial to allow early postoperative rehabilitation without worrying about stretching the repaired ligaments. The ulnar collateral ligament is a large and broad ligament and can easily be identified and repaired. The ulnar part of the lateral collateral ligament may sometimes be difficult to identify or may be too tattered to allow adequate repair. The author has frequently used a strip of the triceps tendon to reinforce the repair. This technique is demonstrated later in this chapter. The results of simple elbow dislocations have been universally good. Several studies have documented good or excellent outcomes with nonoperative management. Recurrent instability is seen in 1 to 2% of cases, and more than 95% of patients are able to return to their previous occupation.4,10,11 Mehlhoff et al4 reported generally favorable results in 51 adult patients with an average follow-up of 34 months. However, 60% of patients reported some symptoms at follow-up. Fifteen percent of patients had a flexion contracture greater than 30 degrees, and 45% had residual pain. Worse results were associated with prolonged immobilization. Lansinger et al13 reported 85% good or excellent results with the nonoperative management of simple elbow dislocations. Elbow fracture-dislocations, especially those with contributions to elbow stability, are extremely demanding to treat. These types of injuries can lead to loss of motion, recurrent dislocation, chronic instability, and the development of post-traumatic arthritis. Good functional outcome can be achieved if stable, anatomic fixation of all of the osseous structures that contribute stability is restored. This will allow early, active motion of the elbow and healing of the capsule and ligamentous structures in their appropriate resting points. The management of radial head fractures will be discussed in detail in Chapter 2. However, the role of the radial head as a stabilizer of the elbow will be emphasized here. The radial head is an oval-shaped structure, which has a concave portion that articulates with the capitellum. The radiocapitellar joint accounts for 60% of load transfer of the elbow. Experimental studies by Morrey et al2 have shown that the radial head is an important secondary stabilizer of the elbow to valgus stress. They showed that when the ulnar collateral ligament was intact, the radial head had little effect on stability. When the ulnar collateral ligament was resected but the radial head was left intact, there was mild instability. However, resection of both the ulnar collateral ligament and the radial head resulted in gross instability of the elbow. If the radial head is fractured, the area of load transmission is decreased, as is the resistance to valgus stress. When the radial head is fractured with a concomitant elbow dislocation, it is imperative to perform an internal fixation or to replace it if it is too comminuted. By restoring the radiocapitellar joint anatomy, the ulnar collateral ligament is not stressed and is allowed to heal. Whether the radial head can be fixed or not depends on the type of fracture. Mason type I fractures are small, nondisplaced fractures that may not have to be addressed surgically. Mason type II fractures are large, displaced fractures that can be fixed internally. Mason type III fractures are too comminuted and cannot be fixed. Therefore, the fragments need to be excised and a radial head implant inserted. The significance of the coronoid in elbow stability is becoming increasingly noticeable. The coronoid serves as a bony anterior buttress, which prevents the posterior displacement of the forearm relative to the humerus. The triceps, brachialis, and biceps brachii have a net resultant force, which is posteriorly directed. When the coronoid fragment is large enough where it can no longer resist the posterior translation of the forearm, the elbow will remain subluxed, despite an initial reduction of the joint. Coronoid fractures are classified based on the location of the fracture (Figure 1-2). Type I fractures are of the tip of the coronoid. The tip of the coronoid does not have any soft tissue attachments and does not require fixation. It does however, indicate that the elbow has been dislocated or subluxed to the point that collateral ligaments have been injured. Type II fractures involve up to 50% of the coronoid. The brachialis and the anterior capsule attach to this portion of the coronoid. The elbow is unstable, especially if there is an associated radial head fracture. The Type III fracture involves more than half of the coronoid and renders the elbow unstable. The anterior band of the ulnar collateral ligament attaches to the base of the coronoid; thus, with a type III fracture, the elbow is unstable to valgus stress. The role of the coronoid as an anterior buttress is also eliminated with this type of fracture. In type I fractures, the ulnohumeral articulation is still stable, and surgical stabilization is not necessary. An adequate lateral radiograph should be obtained to ensure reduction of the joint. Type II fractures require surgical stabilization, especially in the presence of a radial head fracture. If the fragment is large enough and is not comminuted, a single screw can be used to perform osteosynthesis of the fragment. However, if the fragment is small or comminuted, a braided, nonabsorbable suture (number 2 Fiberwire, Arthrex, Naples, FL) can be used (Figure 1-3). Two drill holes are made with a 2 mm drill bit and brought out at the base of the coronoid process. The suture is passed though the fracture fragment(s) as well as the anterior capsule and the brachialis muscle. The two suture limbs are then passed through the drill holes with the help of a suture passer or 20-gauge malleable wire. The suture limbs are tied on the dorsal surface of the proximal ulna (Figure 1-4). Type III fractures render the joint highly unstable and must be fixed internally. The fragment can be fixed with screws alone or through a plate. Occasionally, the medial side of the coronoid is avulsed off secondary to the pull of the anterior band of the ulnar collateral ligament and can be fixed with screws placed from a medial to lateral direction. Alternatively, a small plate from the Acumed (Hillsboro, OR) system, designed by Shawn O’Driscoll, can be used to internally fix the anteromedial coronoid fragment. In either type II or III fractures, if the joint remains unstable after the fragment is fixed and the ligaments are repaired, an external fixator should also be applied. It is the editors’ experience that if the coronoid fragment is well fixed, an external fixator is usually not necessary. McKee et al15 have shown that, in 52 fracture dislocations, the lateral collateral ligament complex was torn in 100% of cases and that the common extensor tendons were ruptured in 66% of cases. These injuries need to be identified and repaired after the fractures have been fixed. The literature is scant with reports on the results of complex elbow fracture dislocations. A recent study by Ring et al16 shows that when a fracture dislocation of an elbow is not treated appropriately, poor results are obtained. Eleven patients with a “terrible triad” were evaluated after a minimum of 2 years. The radial head was repaired in five and resected in four. None of the coronoid fractures were repaired, and the lateral collateral ligament was repaired in only three. Overall, the result of treatment was unsatisfactory for 7 of the 11 patients. All four patients with a satisfactory result had retained the radial head, and two had undergone repair of the lateral collateral ligament. The authors concluded that identification of a coronoid fracture is therefore important and that computed tomography should be used if there is uncertainty.
Dislocations, Fracture Dislocations, and Instability
Anatomy
Bones
Ligaments
Simple Dislocations
Mechanism of Injury
Assessment
Treatment
Nonoperative Treatment
Operative Treatment
Results
Fracture-Dislocations
Radial Head Fractures
Coronoid Fractures
Classification (Regan-Morrey)14
Treatment
Results
Dislocations, Fracture Dislocations, and Instability
Only gold members can continue reading. Log In or Register to continue

Full access? Get Clinical Tree








