Chapter 106 Correction of Fixed Deformities With Total Knee Arthroplasty
Preoperative Planning
Clinical Assessment
Patients with valgus knees and a planovalgus foot walking with a high abduction moment at the knee are prone to stretch the medial collateral ligament after TKA if not overcorrected, and if the foot deformity is not addressed by surgery or insoles.22 In bilateral fixed valgus deformity after one side is corrected with TKA, the other valgus nonoperated knee may push the operated leg in a high adduction moment. If a nonconstrained implant was used and an extensive lateral release was performed, the adduction moment created by the contralateral limb may predispose to a varus angulation, as in a windswept deformity. In bilateral significant fixed flexion contracture deformity, when one side is addressed by TKA, the other flexed and shortened limb will drive the operated leg in flexion again. Careful planning with bilateral simultaneous or short-term staged procedures, when possible, and precautions against flexion contracture recurrence are mandatory. Neuromuscular disorders with low or absent quadriceps activity remain a relative contraindication to TKA; if a patient with this disorder undergoes a TKA procedure, the surgeon will have to address the patient’s need to walk with some residual recurvatum while working with the biomechanical properties of the implant.
Radiographic Assessment
Intra-articular bone deformities can be recognized preoperatively. Ipoplasia of the lateral femoral condyle in valgus knees and the possible need for augmentation should be identified. With ipertrophic medial femoral condyles in knees with a metaphyseal varus deformity, a preoperative kneeling view or computed tomography (CT) scan may prove beneficial to establish the amount of rotational correction needed to achieve a stable and rectangular flexion gap.23,27
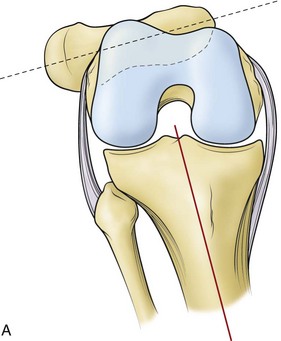
Fixed Varus Deformity
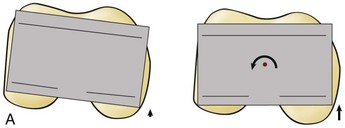
Techniques described to correct fixed varus deformity include the so-called gap technique and the measured resection technique.10,13 Differences between these two techniques are presented in Table 106-1. As described by Whiteside and associates, correction of a varus knee with the gap technique may result in residual varus alignment in flexion.11,29 A 90-degree resection of the tibia without, or with minimal, medial collateral release is followed by soft tissue tension in flexion using tensiometers, which internally rotate the femur (Fig. 106-1A and B). A rectangular flexion gap is then obtained with an externally rotated femoral bone resection parallel to the tibia (see Fig. 106-1B). When the femur derotates in its original position, the knee joint in flexion will be malaligned again in varus (see Fig. 106-1C). Our technique of choice is a combination of the gap technique and the measured resection technique as described by Insall.14 Standard bone resections are performed with different bone landmarks in extension and flexion, while contracted ligaments are released incrementally. Gap equalization is then checked with laminar spreaders, blocks, and trial components.14
Table 106-1 Main Technical Differences Between Soft Tissue Tension and Measured Resection Techniques
| TECHNIQUES | ||
|---|---|---|
| Soft Tissue Tension (Gap Technique) | Measured Resections | |
| Tibia first | Yes | Independent |
| Ligament release | No to minimal | As needed |
| Femoral bone resection | Variable | Fixed |
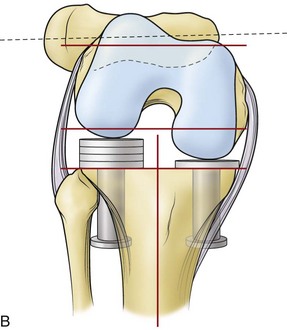
Bone resections are performed according to the preoperative template on the long wb films. Tibial cutting jig positioning should be done according to the talus center distally and the plateau-to-anatomic axis intersection proximally. In constitutional metaphyseal varus deformities, the proximal center of the tibial cutting jig is usually facing the lateral tibial plateau spine (Fig. 106-2). On the femoral side, angulation of the intramedullary cutting guide for valgus correction is established by measuring the divergence between the anatomic and mechanical femoral axes. Failure in achieving varus correction to neutral ±3 degrees is related to a greater incidence of loosening at medium- to long-term follow-up.4
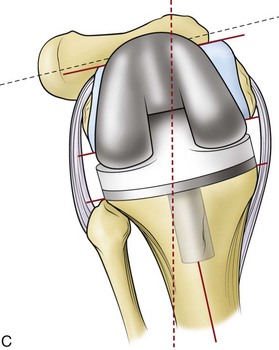
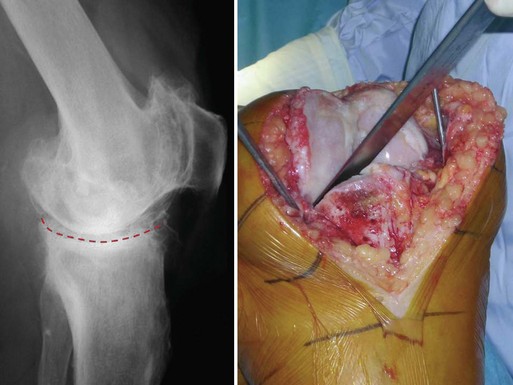
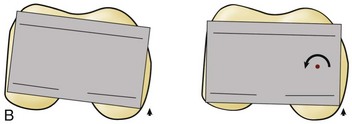
As part of the approach, some initial medial release is performed. With the knee joint in slight flexion, incision of the anterior horn of the medial meniscus allows subperiosteal elevation of a medial flap of tissue, which includes the meniscotibial fibers of the deep medial collateral ligament (MCL). Proximal tibial insertion of the superficial MCL is often involved in the subperiosteal elevation of the medial soft tissue flap as part of the exposure.19 The second step is to sublux the tibia forward in flexion and external rotation (the so-called RanSall maneuver, from its originators Ranawat and Insall). In advanced deformities, the worn tibial medial plateau develops a concave “pagoda” shape in which the femoral condyle is embedded, leading to a difficult tibial dislocation maneuver that may arm the MCL. In these cases, we suggest violating the posterior tibial osteophyte with the tibia still in situ by using a straight osteotome between femur and tibia at 90 degrees of flexion (Fig. 106-3). After joint exposure, both tibial and femoral osteophytes are removed. Proximal tibial and distal femoral cuts are performed. Anteroposterior femoral resections are performed with a rotational position of the cutting jig, according to multiple bone landmarks such as the Whiteside line, the transepicondylar axis, and the posterior condylar line. In cases where more than 3 degrees of external rotation with respect to the posterior condylar line is required, we suggest switching the pivot point of the cutting guide from the center of the knee, as usual, to the medial condyle.26 Pivoting the femoral guide at the center of the femur would create an over-resection of the posterior medial femoral condyle, which may lead to excessive “paradoxical” opening of the medial gap in flexion in a varus knee (Fig. 106-4A and B). The stretched lateral compartment will be better filled in flexion and anterolateral notching will be avoided if few degrees of flexion in the distal femoral cut are applied.
We prefer to remove the posterior cruciate ligament (PCL) and to use a posterior substituting implant for these advanced deformities. We believe that the PCL is part of these deformities. By removing the PCL, it is easier to address complex ligament balancing and to guarantee a reproducible, nonerratic postoperative pattern of kinematics.20 Only in advanced flexion contracture will PCL removal selectively open the flexion gap farther. This 2 to 3 mm gap opening can be filled by adding a few degrees of flexion to the femoral component, and by switching the femoral component rotational pivot point from central to medial.3
Calibrated laminar spreaders and spacer blocks can now be used to check gap symmetry both in flexion and in extension. In fixed deformities, it is common, in this phase of the procedure, to face the need for additional medial release for residual varus in extension. This is particularly evident if a combined fixed flexion deformity is present. The following soft tissue structures will be involved in the incremental medial release to balance the extension gap: the posterior capsule, the posteromedial corner with the posterior oblique ligament (POL), the semimembranosus (SM) direct tibial insertion, and the posterior fibers of the superficial MCL (Table 106-2).30 All these structures can be released with the knee in flexion. Using laminar spreaders, the posterior capsule can be addressed by a periosteal elevator from the femoral side. By holding the knee in deep flexion and applying a posterior drawer to the proximal tibia, it is possible to access the femoral insertion of the posterior capsule with a periosteal elevator. The posteromedial corner of the knee is safely exposed while the joint is held in the “figure four” position, with the foot externally rotated (Fig. 106-5). All of the tibial medial metaphysis is easily exposed, progressively involving the POL and SM insertions up to the posterior midline. If some residual medial tension remains, the distal insertion of the superficial MCL can be released from its posterior aspect in flexion or in extension. To reach this distal broad insertion, the elevator should be deepened distally on the tibial diaphysis at least 8 to 10 cm from the joint line. Alternatively, the MCL could be pie-crusted with a 16-gauge needle with multiple punctures, but progression of this type of release is not always achievable.9 In advanced fixed varus deformities, it is helpful to select a relatively small tibial size to lateralize the tibial component and remove the exposed medial sclerotic bone, which is tenting the medial structures both in extension and in flexion (Fig. 106-6).7 The resultant effect is similar to osteophyte removal, with a reduced need for ligamentous release. Paradoxical medial gap opening in flexion after ligament balancing may now indicate a technical mistake. The surgeon should recheck for a possible excessive external femoral rotation, a varus tibial resection, or full-thickness damage to the superficial MCL.
Table 106-2 Medial and Lateral Soft Tissue Structures of the Knee and Their Involvement in Flexion and Extension Gap Tension
| Extension Gap | Flexion Gap | |
|---|---|---|
| Medial Structures | ||
| Superficial MCL (anterior fibers) | − | + |
| Superficial MCL (posterior fibers) | + | − |
| Deep MCL | + | + |
| Posterior oblique ligament | + | − |
| Semimembranosus tendon | + | − |
| Pes anserinus tendons | + | − |
| Posteromedial capsule | + | − |
| Medial gastrocnemius head | + | − |
| Lateral Structures | ||
| Iliotibial band | + | − |
| Anterior iliotibial band fibers + Lateral retinaculum | − | + |
| Popliteal tendon | − | + |
| Lateral collateral ligament | + | + |
| Biceps tendon | + | − |
| Posterolateral capsule | + | − |
| Lateral gastrocnemius head | + | − |
MCL, Medial collateral ligament.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree